Introduction
Preeclampsia complicates 1% to 5% pregnancies with mild and severe preeclampsia prevalence of 1.42% and 0.49% and contributing greatly to maternal and neonatal morbidity and mortality [
1-
4]. In Cipto Mangunkusumo (RSCM) hospital it contributes to 11% of patients in the emergency unit since 2010. The etiology of preeclampsia remains unknown. One popular hypothesis is that imbalance in circulating placental anti-angiogenic protein and growth factors (pro-angiogenic protein) contributes to the pathogenesis of preeclampsia. This change in the balance results in vascular lesions and endothelial dysfunction, involving many important organs, including the eyes [
4-
6].
Visual disturbance may occur in up to 25% of severe preeclampsia patients with blurred vision being the most common complaint [
7-
9]. It is most frequently affects the chorioretinal vasculature in 40% to 98% of all cases [
8]. This may manifest as decreased retinal arteriole-to-venule ratio, arterio-venous nicking, cotton-wool spots, intraretinal hemorrhages, Elschnig’s spots and serous retinal detachments [
7]. Ocular sequelae may be observed in 30% of patients [
10].
About 26% of the 2250 consultations coming to the Ophthalmology Department in the emergency unit of RSCM hospital in 2013 were visual disturbances in preeclampsia. There is no specific treatment for ocular manifestations and management primarily consists of treating the underlying systemic condition, as the chorioretinopathy generally resolves swiftly post-partum. However, this condition may result in permanent visual loss, mainly caused by optic atrophy or cerebral infarct due to ischemia [
8-
10]. The purpose of this report is to demonstrate the clinical course, management and monitoring of patients with hypertensive chorioretinopathy in preeclampsia.
Case Report
A 27-year-old primigravida in final month of pregnancy consulted Ophthalmology Department of Cipto Mangunkusumo (RSCM) Hospital with chief complaint of blurred vision. There was no history of floaters, photopsia, redness, pain or diplopia. She denied history of trauma, allergy, seizure, smoking, prescribed eyewear, eye surgery or laser photocoagulation. Family history showed no hypertension, diabetes or any pregnancy related problems.
Prior to her pregnancy the patient had no history of hypertension or diabetes mellitus. She has had regular antenatal care, and only in the final month her blood pressure increased, reaching 220/120 mmHg upon arrival to the emergency unit. Blood sugar levels remained normal. Her laboratory results revealed a low platelet count, elevated liver enzymes, elevated LDH, proteinuria 3+, hypoalbuminemia, elevated fibrinogen and D-dimer. She was diagnosed with severe preeclampsia and hemolysis, elevated liver enzymes and low platelets (HELLP) syndrome and received preeclampsia protocol treatment.
On ophthalmologic bedside examination her vision was 3 meters finger-counting in both eyes, and the fundoscopic examination showed decreased retinal arteriole-to-venule ratio, cotton-wool spots and intraretinal hemorrhages. Intraocular pressure and other parts of both eyes were within normal limits. She was assessed with grade 3 hypertensive retinopathy of both eyes, and received no specific treatment from the Ophthalmology Department except for blood pressure regulation by the Obstetrics and Gynaecology Department.
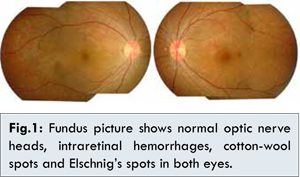
She underwent caesarean surgery in the emergency unit of RSCM that day at 37 weeks of gestation. She gave birth to a healthy term baby girl weighing 2150 grams. After giving birth she experienced a small improvement of her eyesight, but still had blurry vision in both eyes. On ophthalmologic examination 3 weeks after delivery, her best corrected visual acuity was 6/15 in her right eye and 6/12 in her left eye, the intraocular pressure and anterior segment findings were unremarkable. The optic nerve heads and blood vessels were normal but there were still some intraretinal hemorrhages, cotton-wool spots and hyperpigmented patches in the choroid surrounded by rings of hypopigmentation called Elschnig’s spots [Fig.1].
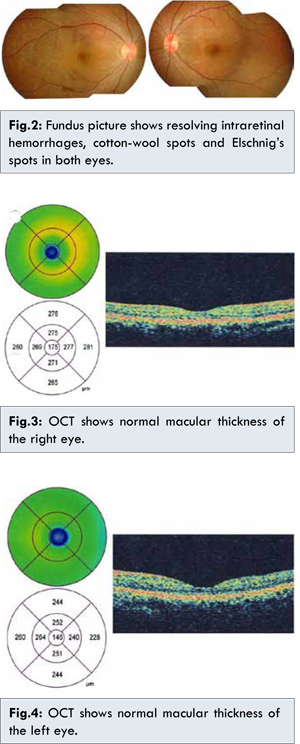
The patient was diagnosed with hypertensive chorioretinopathy in preeclampsia of both eyes. She was referred to the internist to have blood pressure control. Five weeks after delivery she had improving eyesight. She was given captopril 2x12.5 mg and amlodipine 1x10 mg as anti-hypertensive medication by the internist and her blood pressure was within the normal limits. Her best corrected visual acuity was 6/12 in her right eye and 6/6 in her left eye. The fundoscopy examination showed the optic nerve heads were normal and the intraretinal hemorrhages and Elschnig’s spots were resolving in both eyes [Fig.2]. The macular optical coherence tomography (OCT) showed normal results in her both eyes [Fig.3,4].
Seven weeks postdelivery, her best corrected visual acuity improved to 6/10 in her right eye and 6/6 in her left eye. The fundoscopy examination showed normal optic nerve heads and resolving intraretinal hemorrhages and Elschnig’s spots [Fig.5]. A follow up visit at 10 weeks post-delivery showed 6/6 vision in both eyes with normal posterior segment and diminishing Elschnig’s spots [Fig.6].
Discussion
Preeclampsia is seen in about 18% of primiparas with 59% having a severe type [
11-
12]. Preeclampsia is a heterogenous and multifactorial disorder with no clear etiology and pathophysiology. Determinants of preeclampsia rates include a bewildering array of risk and protective factors, including familial factors, sperm exposure, maternal smoking, pre-existing medical conditions and miscellaneous reasons such as plurality, older maternal age and obesity [
2].
The patient in this case was a 27-year old primipara without history of hypertension, smoking or obesity. Her blood pressure reached 220/120 mmHg. Her laboratory results revealed a low platelet count, elevated liver enzymes, elevated LDH, proteinuria, hypoalbuminemia, elevated fibrinogen and D-dimer. She was then diagnosed with severe preeclampsia and HELLP syndrome. HELLP syndrome stands for hemolysis, elevated liver enzymes and low platelets, and the patient’s laboratory results matched with this condition. Prevalence of HELLP syndrome in severe preeclampsia is 40% and it contributes to perinatal morbidity and mortality [
13].
In a normal pregnancy, the vascular endothelial growth factor (VEGF) and the placental growth factor (PlGF) are released by uterine natural killer cells and increase in the maternal circulating level to help maintaining a quiescent endothelial state under the increased inflammatory and stress of pregnancy, and to promote angiogenesis and induce nitric oxide and vasodilatory prostaglandins [
1,
7]. Placental derived soluble fms-like tyrosine kinase 1 (sF1t1), a soluble antagonistic receptor of VEGF and PlGF, appears to be upregulated and strikingly increased in pre-eclamptic patients [
6,
14].
Because sFlt1 antagonizes VEGF and PlGF by binding them and decreasing their unbound serum levels, elevated circulating sF1t1 levels correlate with lower circulating levels of VEGF and PlGF [
1]. Hypothesis state that a high level of sFlt1 and lower concentrations of VEGF and PlGF contribute to systemic endothelial dysfunction in preeclampsia [
5,
15]. Damaged endothelial cells secrete substances that increase the sensitivity to vasopressors and promote coagulation, which causes thrombocytopenia.
Visual disturbance is seen in upto 25% of patients with severe preeclampsia syndrome, with blurred vision and hypertensive retinopathy being most common sign and symptom respectively [
7,
8,
14]. The earliest changes are focal spasms of the retinal arterioles which progress to generalized narrowing. Other retinal manifestations, such as cotton-wool spots, intraretinal hemorrhages, retinal edema and optic nerve edema, are usually seen in severe cases of preeclampsia [
11].
Our patient’s vision was 3 meters finger-counting in both eyes and fundoscopy showed decreased retinal arteriole-to-venule ratio, cotton-wool spots and intraretinal hemorrhages which likely suggested hypertensive retinopathy. She was assessed with grade 3 hypertensive retinopathy of both eyes. Severe arteriolar spasms from focal to generalized are the most common fundoscopic finding, occurring in 50-70% of preeclampsia cases. These spasms will likely recover to a normal state as the blood pressure decreases swiftly into normal post-partum. If the condition is prolonged and hypertension exceeds the capacity of the vessels to auto-regulate, this system mechanism fails and the capillary bed is exposed to elevated pressures. This will lead to occlusion of terminal arterioles, areas of capillary nonperfusion, extravasation, as well as increased vascular permeability, disruption of blood-retinal barrier, retinal ischemia, cotton-wool spots, hemorrhages and retinal edema [
7,
8,
14,
16].
Perfusion abnormalities may range from focal infarction to larger arterioles necrosis [Fig.8]. Smaller infarcts, due to ischemia to the overlying retinal pigment epithelium and outer retina, produce small patches of atrophy, which become hyperpigmented and surrounded by a margin of hypopigmentation called Elschnig’s spots. Serous retinal detachment, as a secondary phenomenon from increased vascular permeability, leakage of proteins, and fluid into the subretinal space, is seen in approximately 1% of patients with preeclampsia [
17-
19].
There was improvement on 3 weeks after delivery, our patient’s best corrected visual acuity was 6/15 in her right eye and 6/12 in her left eye. In the funduscopy there were still some intraretinal hemorrhages, cotton-wool spots and Elschnig’s spots. The macular Optical coherence tomography (OCT) was performed on our patient, which showed normal results; this could be attributed to the fact that the patient’s condition already improved to a normal state, weeks after delivery of the baby. The patient was diagnosed with hypertensive chorioretinopathy in preeclampsia of both eyes.
Specific treatments for the ocular manifestations of preeclampsia are not generally indicated. Treatment is more directed to the underlying systemic disease [
14]. Treatment of systemic arterial hypertension is essential in reducing or reversing these ocular manifestations of the disease. Immediate delivery is the only definitive treatment, as the signs and symptoms of preeclampsia are reversible after delivery [
10].
Our patient received no specific treatment from the Ophthalmology Department, but only received blood pressure regulation by the Obstetrics and Gynaecology Department. The patient underwent a Caesarean surgery in the emergency unit of RSCM that day, and her blood pressure returned to normal, as well as the complaint of visual disturbance. Follow-up examinations for 2.5 months showed good improvement of her visual acuity into 6/6 in both eyes with mostly normal fundus appearance, except for fading Elschnig’s spots.
Prognosis of chorioretinopathy in preeclampsia is quite good. Even though there is still 1-3% possibility of permanent damage, most patients with preeclampsia recover their vision within a few weeks after delivery, and after normalization of blood pressure. Permanent blindness from retinal vascular changes is rare, and cortical blindness is also generally reversible. However, sequelae have been reported in 30% of the cases. Some may have residual retinal pigment epithelium changes, like Elschnig’s spots. Although rare, optic atrophy may also develop if chorioretinal atrophy is widespread [
7,
8,
14,
20].
Our case shows an excellent outcome of hypertensive chorioretinopathy in preeclampsia. Preeclampsia is an emergency condition involving acute visual loss. To avoid serious or life-threatening conditions, it is important to promptly evaluate pregnant women that suffer from blurry vision, to refer them for appropriate treatment in a timely manner.
References
- Cunningham FG. Hypertensive disorders in pregnancy. In: Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD. Williams obstetrics. 22nd ed. New York: McGraw-Hill Companies; 2007. pp.773-823.
- Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of preeclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Cl Ob. 2011;25(4):391-403.
- Xiao J, Shen F, Xue Q, Chen G, Zeng K, Stone P, et al. Is ethnicity a risk factor for developing preeclampsia? An analysis of the prevalence of preeclampsia in china. J Hum Hypertens. 2014; 28(1):11-15.
- Young BC, Levine RJ, Karumanchi SA. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010; 5:173-192.
- Noori M, Donald AE, Angelakopoulou A, Hingorani AD, Williams DJ. Prospective study of placental angiogenic factors and maternal vascular function before and after preeclampsia and gestational hypertension. Circulation. 2010;122:478-487.
- Rana S, Karumanchi A, Lindheimer MD. Angiogenic factors in diagnosis, management, and research in preeclampsia. Hypertension. 2014;63:198-202.
- Samra KA. The eye and visual system in the preeclampsia/eclampsia syndrome: what to expect? Saudi J Ophthalmol. 2013;27:51-53.
- Somerville-Large LB. A case of permanent blindness due to toxemia of pregnancy. Br J Ophthalmol. 1950;34:431-434.
- Moseman CP, Shelton S. Permanent blindness as a complication of pregnancy-induced hypertension. Obstet Gynecol. 2002;100(5):943-945.
- Ober RR. Preeclampsia-eclampsia syndrome. In: Ryan SJ (ed). Retina. 4th ed. Philadelphia: Elsevier; 2006. p. 1367-1376.
- Amaral WT, Souza SS, Peracoli JC. Gestational hypertensive syndromes: risk factors identification and complications in a primiparous population. Int J Womens Cardiovasc Heal. 2012;2(3):335.
- Reddy SC, Nalliah S, George SRK, Who TS. Fundus changes in pregnancy-induced hypertension. Int J Ophthalmol. 2012;5(6):694-697.
- Gupta T, Gupta N, Jain J, Gupta S, Bhatia P, Bagla J. Maternal and perinatal outcome in patients with severe preeclampsia/eclampsia with and without hellp syndrome. J Univ Coll Med Sci. 2013;1(4):7-12.
- Klesert TR, Schachat AP. Pregnancy-induced hypertension. In: Joussen AM, Gardner TW, Kirchhof B, Ryan SJ (eds). Retinal vascular disease. Heidelberg: Springer; 2007. pp. 691-699.
- Thadhani R. First trimester placental growth factor and soluble fms-like tyrosine kinase 1 and risk for preeclampsia. J Clin Endo. 2004;89(2):770-775.
- Errera MH, Kohly RP, Cruz L. Pregnancy-associated retinal diseases and their management. Surv Ophthalmol. 2013;58(2):127-142.
- Skuta GL, Cantor LB, Weiss JS. Retina and vitreous. San Francisco: American Academy of Ophthalmology; 2011. p. 108-109, 182-186.
- Gundlach E, Junker B, Gross N, Hansen LL, Pielen A. Bilateral serous retinal detachment. Br J Ophthalmol. 2013;97(7):939-940.
- Kuhl D, Schwartz SG, Sheth BP, Mieler WF. Ocular manifestations of pregnancy. In: Arevalo JF (ed). Retinal and choroidal manifestations of selected systemic diseases. Berlin: Springer; 2013. p. 465-477.
- Do DV, Rismondo V, Nguyen QD. Reversible cortical blindness in preeclampsia. Am J Ophthalmol. 2002;134(6):916.