|
|
|
|
|
Unexpected Neurological Sequelae following Cerebral Fat Embolism Syndrome
|
|
|
Ali Veysel Kara1, Yasar Yildirim1, Süreyya Yilmaz2, Zulfukar Yilmaz1, Ali Kemal Kadiroglu1, Mehmet Emin Yilmaz1
Department of Nephrology1 and Chest Diseases2, Faculty of Medicine, Dicle University, Diyarbakir, Turkey. |
|
|
|
|
|
Corresponding Author:
|
Dr. Ali Veysel Kara
Email: aliveyselkara@hotmail.com
|
|
|
|
|
|
|
|
|
Received:
15-JAN-2015 |
Accepted:
18-APR-2015 |
Published Online:
10-MAY-2015 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Fat embolism syndrome is the most common form of non-thrombotic embolism and often described by presence of fat globules blocking small vessels in lung, skin or brain. The classical triad of fat embolism syndrome is respiratory manifestations, neurological signs and symptoms and petechial rash. Almost all neurological deficits are transient and fully reversible. Early diagnosis and supportive therapy is crucial for management of FES to decrease mortality and morbidity. We present a case of fat embolism syndrome due to multiple fractures recovered with neurological sequelae. |
|
|
|
|
|
Keywords :
|
Fat Embolism, Purpura, Thrombosis, Exanthema, Brain.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff649406000000ad03000001000f00 6go6ckt5b5idvals|461 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Fat embolism was first defined by Zenker [1] as fat droplets in pulmonary vascular beds in an autopsy of patient after crush injury and in 1873, von Bergmann [2] described fat embolism syndrome as a clinical syndrome in a patient with femur fracture. Fat embolism is the most common form of non-thrombotic embolism and often described by the presence of fat globules blocking small vessels in lung, skin or brain. It is caused by many conditions especially trauma or surgery of long bones and pelvis. Many patients who have fat emboli are often asymptomatic and only a small percentage of patients have symptoms such as dyspnea, altered mental status and petechiae. This clinical situation is defined as fat embolism syndrome and can be lethal with an overall mortality of 5%-15% [3]. We present a case of fat embolism syndrome due to multiple fractures with neurological sequelae
Case Report
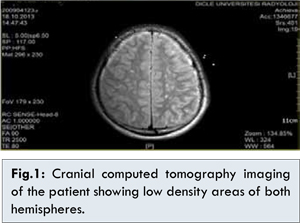
A 20 year old male patient with no significant past medical history was admitted to the emergency service after a traffic accident. When he was admitted, he had multiple orthopedic injuries and no signs of craniocerebral injury. He had complete fractures of bilateral femur, left tibia and fibula fractures, right fibula fracture, split fracture of metatarsal of right foot. At admission, patient was alert and Glasgow coma scale score was 15, blood pressure was 140/90 mm Hg and neurological examination was normal. After 12 hours of admission, sudden deterioration in consciousness was noticed which was accompanied by generalized tonic clonic seizures and soon followed by dyspnea. Re-evaluated Glasgow coma scale score was 6 (E1V1M4). No abnormality was noted in chest X-ray, however, thoracic computed tomography (CT) angiography revealed focal patchy infiltrates on bilateral upper lobes and superior segments of lower lobes of lungs without any evidence of thromboembolism. Cranial magnetic resonance imaging (MRI) of patient revealed multiple foci with reduced diffusion on brain stem, bilateral cerebral and cerebellar hemispheres, basal ganglia, centrum semiovale and white matter. On cranial CT imaging of patient, there were low density areas on both cerebral hemispheres, basal ganglia and brain stem [Fig.1]. Preoperative arterial blood gas analysis showed pH: 7.39, pO2: 58.8, pCO2: 26.4, HCO3: 17.8 (with 2 L/min nasal oxygen support). Patient was taken to the operation for the transient fixation surgery. External fixations were made to bilateral femur, left tibia and left humerus and open reduction was made to right foot lisfranc fracture. After the operation, there was no improvement in the patient’s status. Subsequently, patient was intubated and transferred to the internal medicine intensive care unit with the diagnosis of traffic accident, multiple bone fractures and fat embolism syndrome and mechanical ventilation was initiated. Petechiae also appeared on the anterior chest wall and axillary regions. Patient’s situation was evaluated as cerebral fat embolism syndrome after cranial MRI and neurological consultation in addition to findings such as respiratory deterioration and wide spread petechiae on the upper part of body. Supportive treatment was started in the ICU. One unit of red blood cell (RBC) transfusion for decreased hemoglobin level and 3 units of fresh frozen plasma (FFP) were given for mild prolongation of prothrombin time (PT). High dose corticosteroids and albumin were also given to the patient for the fat embolism syndrome. Daily consultations with related specialties were made. After 1 month of admission, corrective orthopedic operation was made and patient was weaned off from mechanical ventilation. Gradually improvement in patient’s neurological status was noted and physiotherapy was started.
Fat embolism syndrome classically presents 24-72 hours after the injury and it occurs rarely as early as 12 hours or as much as 2 weeks later [4]. The classical triad of fat embolism are respiratory changes [5] (variable severity of symptoms such as dyspnea, tachypnea, hypoxemia etc. but a number of cases may progress to respiratory failure), neurological signs and symptoms [6,7] (a spectrum from mild confusion to severe seizures but fortunately, almost all neurological deficits are transient and fully reversible) and petechial rash [8] (due to embolization of small dermal capillaries causing extravasation of erythrocytes and especially seen in oral mucous membranes, conjunctiva and skin folds of upper body especially neck and axilla). Less frequent symptoms and signs such as pyrexia, myocardial depression, coagulation abnormalities, retinal and renal changes can be seen in the course of syndrome [3,9].
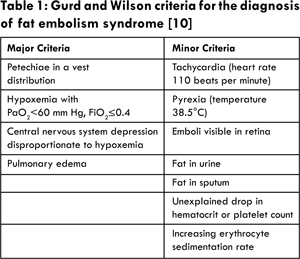
The diagnosis of fat embolism syndrome is usually based on clinical findings but some biochemical changes may aid to diagnosis. The mostly accepted guidelines for the diagnosis of fat embolism syndrome is proposed by Gurd and Wilson which require at least one major or four minor criteria (Table 1) [10]. Some other criteria’s for diagnosis of fat embolism syndrome have been proposed recently such as Schonfeld’s criteria [11] and Lindeque’s criteria [12].
Fat embolism syndrome is fat in the circulation associated with an identifiable clinical pattern of symptoms and signs [3]. Classical triad of fat embolism syndrome can also be seen in other critical illnesses and diagnosis of fat embolism syndrome is often made by exclusion. The presentation of fat embolism syndrome can vary from mild to fulminant lethal form. Fulminant fat embolism syndrome is caused by sudden intravascular obstruction of pulmonary vasculature by fat globules and leading to right heart failure, shock and also death within the first 1-12 hours of injury and milder forms of fat embolism syndrome may go undetected clinically [13,14].
FES is associated with trauma to long bones or pelvis or surgical trauma in 90% of patients and in 5% of cases; it has an atraumatic cause (e.g. none marrow transplantation, pancreatitis, sickle cell disease, high dose corticosteroids) [15]. Rare causes of FES include hepatic trauma, liposuction, lipectomy, external cardiac compression, gas gangrene, decompression sickness and lipid infusions [15,16]. Pinney SJ et al.[17] reported a FES rate of only 4% in a study of 274 consecutive patients with isolated femoral shaft fractures. The present patient had multiple long bone fractures which is the most common cause of fat embolism syndrome. The risk of fat embolism syndrome after bilateral femur fractures is higher than isolated long-bone fractures [18]. In our case, he had multiple long bone fractures. The fat embolism syndrome is characterized by an asymptomatic period of 12-72 hours (commonly 36 hours, although up to 6 days has been described) following bony injury or manipulation of the fracture site, and a symptomatic period which includes respiratory effects (95%), cerebral effects (60%) and petechiae (33%) [19]. In the present case; there was a 12 hour asymptomatic period and respiratory (hypoxia) and cerebral symptoms (deterioration in consciousness, seizure) developed after 12 hours of trauma and petechiae developed after 24 hours of trauma.
Capillaries especially on venous side are affected mainly in the FES. Hence, the lung is the most commonly affected organ in the fat embolism syndrome. However, the fat globules and chylomicrons gain access to the systemic circulation and can also affect heart, brain, skin and retina [20]. There are several explanations for this such as passing of deformed fat globules through pulmonary capillaries [21], pulmonary A-V malformations [22], patent foramen ovale and re-opening of closed patent foramen ovale [23]. In the present case, patient’s ECHO was normal and the other mechanisms except for cardiac causes might play role.
Fat embolism syndrome is a clinical diagnosis of exclusion. No pathognomonic test will confirm the diagnosis of FES but routine blood investigations may show a decrease in Hg and hematocrit, thrombocytopenia and features of disseminated intravascular coagulation (DIC) [19]. In our patient, thrombocytopenia, mild form of DIC, hypoxia with hypocarbia and respiratory alkalosis was seen. CT brain may be normal, or with minimal brain edema, or diffuse white matter petechial hemorrhages [3]. In the present case, brain CT was normal. In diffusion-weighted MRI; multiple infarcts could be seen in patients with FES [24,25]. In our patient, there was multiple foci with reduced diffusion on brain stem, cerebral and cerebellar hemispheres. CT scans of chest wall are usually normal but generalized pulmonary interstitial or alveolar opacifications may develop [26]. In our case, there was focal patchy infiltrates on both upper lobes and superior segments of lower lobes of lungs.
There is no specific therapy for the fat embolism syndrome. Supportive therapy such as maintenance of adequate oxygenation, normal blood levels, hydration and prevention of complications are the mainstay of therapy. In the present case, all of the supportive measures were made such as RBC transfusion for decreased Hg levels, FFP transfusion for a mild DIC, and mechanical ventilation for respiratory failure. Intravenous albumin and high dose corticosteroid therapy were given to the patient. According to the literature, albumin and corticosteroids have some beneficial effects on patient outcomes [6,22,24]. Another key step in the management of fat embolism syndrome is the early fixation of fractures within 24 hours [27]. In a study by Pinney SJ et al. [17], 60 patients who underwent surgery within 10 hours of injury, none of the patients was diagnosed as FES. In the present case, patient was taken to the operation for early surgical fixation after 12 hours of trauma. The timing of early stabilization of fractures may be important for prevention of fat embolism syndrome.
Severe neurological impairment in a trauma patient without initial major head injury may be due to FES. Cerebral fat embolism should always be suspected in these patients especially with long bone fractures. Cerebral dysfunction associated with FES are usually reversible in the majority of reports in the literature [28-30]. In our patient, neurological impairment was not fully recovered. Some sequelae such as difficulty in speech, impairment in short term memory have been observed after 3 months of therapy.
In conclusion, early diagnosis and supportive therapy are crucial for management of FES to decrease mortality and morbidity. FES is a clinical diagnosis of suspicion so it should be suspected in all trauma patients especially with long bone fractures accompanied by neurological and respiratory impairments.
References
- Zenker FA. Beitrage zur Anatomie und Physiologie der Lunge. J Braundorf 1861.
-
Von Bergmann EB. Ein fall todlicher fettembolie. Klan Wochenschr 1873;10:385-387.
-
Mellor A, Soni N. Fat embolism. Anaesthesia 2001;56:145-154.
-
Carr J, Hansen S. Fulminant fat embolism. Orthopedics. 1990;13(2):258-261.
-
King MB, Harmon KR. Unusual forms of pulmonary embolism. Clin Chest Med. 1994;15:561-580.
-
Müller C, Rahn BA, Pfister U, Meinig RP. The incidence, pathogenesis, diagnosis, and treatment of fat embolism. Orthop Rev. 1994;23:107-117.
-
Richards RR. Fat embolism syndrome. Can J Surg. 1997;40:334-339.
-
Sulek CA, Davies LK, Enneking FK, Gearen PA, Lobato EB. Cerebral microembolism diagnosed by transcranial Doppler during total knee arthroplasty: correlation with transesophageal echocardiography. Anesthesiology. 1999; 91:672-676.
-
Van den Brande FG, Hellemans S, De Schepper A, De Paep R, Op De Beeck B, De Raeve HR, et al. Post-traumatic severe fat embolism syndrome with uncommon CT findings. Anaesth Intensive Care. 2006;34(1):102-106.
- Gurd AR, Wilson RI. The fat embolism syndrome. J Bone Joint Surg Br 1974;56:408-416.
-
Schonfeld SA, Ploysongsang Y, DiLisio R, Crissman JD, Miller E, Hammerschmidt DE et al. Fat embolism prophylaxis with corticosteroids. A prospective study in high-risk patients. Ann Intern Med. 1983;99(4):438-443.
-
Lindeque BG, Schoeman HS, Dommisse GF, Boeyens MC, Vlok AL. Fat embolism syndrome: A double blind therapeutic study. J Bone Joint Surg Br. 1987;69:128-131.
-
Hagley SR. The fulminant fat embolism syndrome. Anaesth Intens Care. 1983;11:167-170.
-
Muntoni F, Cau M, Ganau A, Congiu R, Arvedi G, Mateddu A, et al. Brief report: Fulminating fat emboism syndrome caused by paradoxical embolism through a patent foramen ovale. N Engl J Med. 1993;329:926-929.
-
Dudney TM, Elliott CG. Pulmonary embolism from amniotic fluid, fat, and air. Prog Cardiovasc Dis. 1994; 36:447-474.
-
Levy DL. The fat embolism syndrome: a review. Clin Orthop 1990;2612:281-286.
-
Pinney SJ, Keating JF, Meek RN. Fat embolism syndrome in isolated femoral fractures: Does timing of nailing influence incidence? Injury. 1998; 29:131-133.
-
Nork SE, Agel J, Russell GV, Mills WJ, Holt S, Routt ML Jr. Mortality after reamed intramedullary nailing of bilateral femur fracture. Clin Orthop Relat Res. 2003;415:272-278.
-
Bulger EM, Smith DG, Maier RV, Jurkovich GJ. Fat embolism syndrome (a 10-year review). Arch Surg. 1997;132:435-439.
-
Jacob George, Reeba George, Dixit R, Gupta RC, Gupta N. Fat embolism syndrome. Lung India. 2013;30(1):47-53.
-
Schemitsch EH, Jain R, Turchin DC, Mullen JB, Byrick RJ, Anderson GI, et al. Pulmonary effects of fixation of a fracture with a plate compared with intramedullary nailing. J Bone Joint Surg Am. 1997;330:642-643.
-
Gossling HR, Pellegrini VD Jr. Fat embolism syndrome: A review of the pathophysiology and physiological basis of treatment. Clin Orthop. 1982;165:68-82.
-
Pell AC, Hughes D, Keating J, Christie J, Busuttil A, Sutherland GR. Brief report: Fulminant fat embolism syndrome caused by paradoxical embolism through a patent foramen ovale. N Engl J Med. 1993;329:926-969.
-
Tsai IT, Hsu CJ, Chen YH, Fong YC, Hsu HC, Tsai CH. Fat embolism syndrome in long bone fracture: Clinical experience in a tertiary referral center in Taiwan. J Chin Med Assoc. 2010;73:407-410.
-
Habashi NM, Andrews PL, Scalea TM. Therapeutic aspects of fat embolism syndrome. Injury. 2006;37:68-73.
-
Liljedahl SO, Westermark L. Aetiology and treatment of fat embolism. Report of five cases. Acta Anaesthesiol Scand. 1967;11:177-194.
-
Bone LB, Johnson KD, Weigelt J, Scheinberg R. Early versus delayed stabilization of femoral fractures: A prospective randomised study. J Bone Joint Surg. 1989;71:336-340.
-
Needham AP, McLean AS, Stewart DE. Severe cerebral fat embolism. Anaesth Intensive Care. 1996;24:502-504.
-
Erdem E, Namer IJ, Saribas O, Aras T, Tan E, Bekdik C, et al. Cerebral fat embolism studied with MRI and SPECT. Neuroradiology. 1993;35:199-201.
-
Ibanez CN, Collado NR, Gavina SI, De Medrano ML, Chicharro FM. Fat embolism syndrome without respiratory failure. Clinical Intensive Care. 1999;10:101-103.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Kara AV, Yildirim Y, Yilmaz S, Yilmaz Z, Kadiroglu AK, Yilmaz MEUnexpected Neurological Sequelae following Cerebral Fat Embolism Syndrome.JCR 2015;5:207-211 |
|
Kara AV, Yildirim Y, Yilmaz S, Yilmaz Z, Kadiroglu AK, Yilmaz MEUnexpected Neurological Sequelae following Cerebral Fat Embolism Syndrome.JCR [serial online] 2015[cited 2025 Oct 27];5:207-211. Available from: http://www.casereports.in/articles/5/1/Unexpected-Neurological-Sequelae-following-Cerebral-Fat-Embolism-Syndrome.html |

|
|
|
|
|