Introduction
Aspiration of a foreign body into upper airways is a life-threatening emergency which requires immediate intervention. These cases may admit to medical facilities immediately for acute and immediate symptoms or present late due to insidious onset of symptoms. Literature review shows most of the cases visit the physicians in the first day [
1]. The history is very important in those cases but at least 10-20% of patients had no history of aspiration despite of foreign bodies having been extracted later [
2].
Although seen exclusively in childhood, few cases are detected in adulthood with very variable symptoms according to localization of the material. When these objects occlude the main upper airways, they lead to acute respiratory distress but distal locations frequently lead to more generic symptoms such as cough, dyspnea, wheezing and fever [
3-
5]. When the diagnosis is suspicious, late admissions can lead to post-obstructive pneumonia, atelectasia, bronchiectasia, granulation tissue, brochus stricture, hemoptysis, and lung abscess [
5-
7] while some cases may mimic bronchial hypersensitivity and asthma. This report presents a case who had been followed and treated for difficult asthma.
Case Report
A 35-year-old female patient who had been followed up for difficult asthma for the last 5 years was referred to our pulmonary rehabilitation (PR) center. She had been on long-acting beta agonist and inhaled steroids and was given long acting muscarinic antagonist, theophylline and leucotriene antagonists 2 years ago, which unfortunately failed to control her symptoms and she was eventually referred to PR. Initial history revealed that she had been experiencing cough, wheezing and frequent infections since her childhood. She had progressive dyspnea for the last 2 years and recently experienced hemoptysis with sputum last week. She had undergone nasal polypectomy 17 years ago and had no allergy to analgesics. In the physical examination, her respiratory sounds were normal aside from marked stridor.
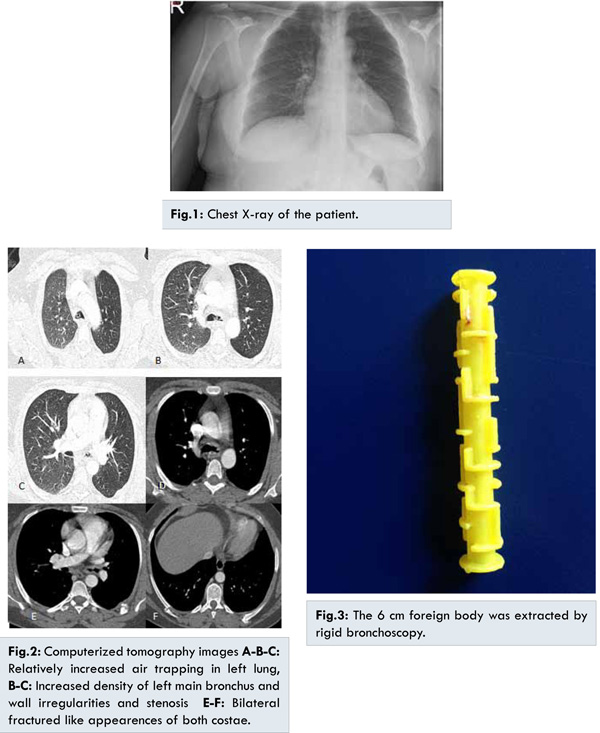
Her oxygen saturation at room was 95%. She denied smoking or occupational hazard history and showed negative early reversibility along with prick tests and positive delayed reversibility. Pulmonary function test (PFT) revealed as forced expiratory volume in the first second (FEV1) 57% (1.40 L), forced vital capacity (FVC) 82% (2.3 L) of predicted, FEV1/ FVC 60 of predicted ratio and peak expiratory flow (PEF) 2.43 L/sec. The PFT in the hospital discharge report stated the FEV1 as 59% (1.47 L), FVC 79% (2.26 L) of predicted with 64 of predicted ratio, PEF 2.68 L/sec, total lung capacity (TLC) 102% (4.20 L), residual volume (RV) 156% (1.96 L) of predicted, RV/TLC 46 of predicted ratio, diffusing capacity of lung for carbon monoxide (DLCO) 102% and DLCO/VA as 105% of predicted. Posteroanterior chest X-ray revealed no pathology [Fig.1]. Computerized tomography (CT) revealed bilateral fractured like appearences of both costae, relatively increased air trapping in left lung, increased density of left main bronchus and wall irregularities and stenosis [Fig.2]. She underwent a fiberoptic bronchoscopy which showed a yellow, plastic-made, tube-like rigid foreign body located at lower trachea and right main bronchus. Chest surgeons recommended rigid bronchoscopy during which the foreign body was extracted [Fig.3]. There was granulation tissue in left main bronchus. After the removal, the lung function test was repeated which yielded FEV1 71% (1.74 L), FVC 87% (2.47 L), FEV1/FVC ratio 70 and PEF 3.29 L/sec. She continuously denied any aspiration when asked about any foreign body aspiration. She also had no history of drug abuse, alcohol, syncope, epilepsy, and was reported to have no psychiatric disorder after psychiatry consultation.
The material was examined in detail for the suspicion of a forgotten medical instrument part during previous polypectomy. Bone mineral densitometry performed due to multiple fractures in costae and history of previous steroid use revelaed osteopenia and orthopedics consultation suspected these fractures of trauma origin, but she again denied any trauma history. After the removal of foreign body, she recovered completely and was discharged on second day after the bronchoscopy. She was completely well and symptom-free at one month follow-up visit.
Discussion
Because most of the cases of foreign body aspiration involved children, studies extensively used pediatric patients. In a study of 174 patients, diagnosis after 30 days was 19.6% and complication rate was 60% [
8]. The most common causes of foreign body aspiration in adults were mental retardation, epilepsy, parkinson disease, cerebral tumours and dental procedures under local anestesia [
9]. Twenty five percent of cases which were diagnosed after 4 days had persistent cough and wheezing [
8] which was in the form of dry nonproductive irritative episodes. When the material is located in the bronchi, the severity of symptoms diminish. Breathlessness, cyanosis, stridor and fever are other symptoms [10]. Our case had chronic cough starting from childhood and had experienced hemoptysis and frequent recurrrent pneumonia episodes recently.
The first test to be done in case of a suspicion of a foreign body aspiration is chest X-ray which has a sensitivity of 60%-85% and specificity of 52%-68% [
11,
12]. Posteroanterior chest X-ray has a sensitivity of 75%-97% [
13-
14]. Metal bodies are easily identified in these X-ray films but most of those aspirated bodies are radiolucent. In these cases, indirect findings such as segmental or lobar collapse, post-obstructive infiltration, hyperlucent one sided lung fields due to air entrapment can also be found [
15]. In case of partial obstruction of the bronchial lumen there would be air trapping appearane in the X-ray [
16,
17]. The most common radiologic findings are unilateral increased aeration and atelectasia [
18]. In a study of 28 patients, it was reported that 21.8% of patients had their diagnosis made after 30 days. All those patients had chronic cough, and half of them had rhonchus, crepitation, increased aeration, atelectasia, mediastinal shift while 63% had complications such as pneumonia, bronchiectasia or bronchoesophageal fistula formation [
19]. Because the mobile foreign body in our case had a central tube like lumen which lead to sufficient aeration of the distal respiratory system, the patient might not have experienced atelectasia, bronchiectasia or fistula formation. Chest X-ray was unanabe to identify plastic made foreign body in our patient. CT had showed relatively increased aeration in the left lung and had she undergone expiration-phase X-ray, it would have shown air trapping.
Virtual bronchoscopy with multislice CT is a new diagnostic modality which can show whole tracheobronchial tree and give foreign bodies’ 3D location and has a sensitivity and specificity of nearly 100% [
11,
20]. In our case, CT was not perfomed under virtual bronchoscopy mode so no foreign body was observed but some secondary signs such as increased aeration and stenosis in bronchial lumen was evident.
Formation of granulation tissue is another important complication after a foreign body aspiration. Although the exact timing of aspiration was not clear on this case, it was reckoned to be 2 years ago as there had been no complication because the foreign material was tube like and mobile. Otorhinolaryngology consultation reported that the material could not be a medical leftover from the polypectomy operation done in 1998. As the foreign body resembled a toy and was 6 cm it could not have been swallowed during childhood period (could have caused asphyxia). She had no psychiatric or neurologic disorder. Thorax CT showed multiple costae fractures, but the initial thought of traumatic aspiration aside from long-term chronic steroid use might have been the cause, was not justified afterwards.
The bodies in tracheobroncial tree may mimick many pathologic conditions specifically, bronchial asthma [
21]. Wrong diagnosis may lead to inappropriate interventions and sometimes catastrophic consequences such as lung resection in a case of an undiagnosed foreign body aspiration [
22]. Our case was using all the available bronchodilator treatment including chronic steroids. After the removal, she has been followed with only low dose steroid and long acting beta agonist and had no major symptoms, episode or admission to hospital.
Conclusion
The symptoms observed in foreign body aspiration are usually non-specific and generic and can lead to erroneous or delayed diagnosis. Detailed history and elaborate physical examination constitutes the mainstay of diagnosis. Differential diagnosis of difficult asthma and recurrent pneumonia should also include foreign body aspiration.
References
- Blazer S, Naveh Y, Friedman A. Foreign body in the airway. Am J Dis Child. 1980;134:68-71.
- Brkic F, Delibegovic-Dedic S, Hajdarovic D. Bronchoscopic removal of foreign bodies from children in Bosnia and Herzegovina: experience with 230 patients. Int J Pediatr Otorhinolaryngol. 2001;60:193-196.
- Friedman EM. Tracheobronchial foreign bodies. Otolaryngol Clin North Am. 2000;33:179-185.
- Steen KH, Zimmermann T. Tracheobronchial aspiration of foreign bodies in children: a study of 94 cases. Laryngoscope. 1990;100:525-530.
- Karakoc F, Cakir E, Ersu R, Uyan ZS, Colak B, Karadag B, et al. Late diagnosis of foreign body aspiration in children with chronic respiratory symptoms. Int J Pediatr Otorhinolaryngol. 2007;71:241-246.
- Mise K, Jurcev Savicevic A, Pavlov N, Jankovic S. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc. 2009;23:1360-1364.
- Dong YC, Zhou GW, Bai C, Huang HD, Sun QY, Huang Y, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med. 2012;51:2515-2519.
- Karakoc F, Karadag B, Akbenlioglu C, Ersu R, Yildizeli B, Yüksel M, et al. Foreign body aspiration: what is the outcome? Pediatr Pulmonol. 2002;34:30-36.
- Yilmaz A, Akkaya E, Damadoglu E, Gungor S. Occult bronchial foreign body aspiration in adults: analysis of four cases. Respirology. 2004;9:561-563.
- Erikci V, Karacay S, Arikan A. Foreign body aspiration: a fouryears experience. Ulus Travma Derg. 2003;9:45-49.
- Haliloglu M, Ciftci AO, Oto A, et al. CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration. Eur J Radiol. 2003;48:188-192.
- Kosucu P, Ahmetoglu A, Koramaz I, et al. Low-dose MDCT and virtual broncoscopy in pediatric patients with foreign body aspiration. Am J Roentgenol. 2004;183:1771-1777.
- Silva AB, Muntz HR, Clary R. Utility of conventional radiography in the diagnosis and management of pediatric airway foreign bodies. Ann Otol Rhinol Laringol. 1998;107:834-838.
- Gürsu S, Sirmali M, Gezer S, ve ark. Yetiskinlerde trakeobronsiyal yabanci cisim aspirasyonlari. Turkish J Thorac Cardiovasc Surg. 2006;14:38-41.
- Zissin R, Shapiro-Feinberg M, Rozenman J, Smorjik J, Hertz M. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol. 2001;11:602-611.
- Lima JAB, Fisher GB. Foreign body aspiration in children. Paediatr Respir Rev. 2002; 3:303-307.
- Girardi G, Contador AM, Castro-Rodriguez JA. Two new radiological findings to improve the diagnosis of bronchial foreign-body aspiration in children. Pediatr Pulmonol. 2004;38:261-264.
- Pasaoglu I, Dogan R, Demircin M, Hatipoglu A, Bozer AY. Bronchoscopic removal of foreign bodies in children: retrospective analysis of 822 cases. Thorac Cardiovasc Surg. 1991;39:95-98.
- Saquib MM, Rauf KA, Al-Bassam A. Late presentation of tracheobronchial foreign body aspiration in children. J Trop Pediatr. 2005;51:145-148.
- Hong SJ, Goo HW, Roh, JL. Utility of spiral and cine CT scans in pediatric patients suspected of aspirating radiolucent foreign bodies. Otolaryngol Head Neck Surg. 2008;138:576-580.
- Çelikel S. Endobronsial nedenler. Turk Toraks Derg. 2013;14:22-23.
- Kaya S, Yalçinkaya I, Moldibi B, ve ark. Trakeobronslial yabanci cisim aspirasyonlari. Solunum Hastaliklari. 1991;2:255-264.