Introduction
Tuberculosis (TB) is one of the major burdens in developing country. Tuberculosis of central nervous system manifests as meningitis, meningoencephalitis, tuberculoma, cerebral abscess, or endarteritis. Rarely TB meningitis can present with cerebral venous thrombosis. At spinal level it can present as arachnoidities, spinal meningitis, Pott’s spine and syringomyelia. This case report describes an unusual association of tuberculous meningitis with cerebral venous thrombosis.
Case Report
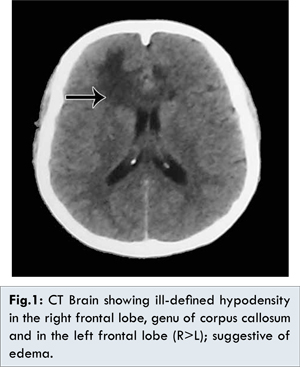
28 year old, one month postpartum lady presented with history of fever for one week duration, headache and altered sensorium for 1 day. On examination her vitals were normal. She was drowsy and disoriented. She had right sided hemiparesis, signs of meningeal irritation with normal fundus examination. Her breasts were soft. Her laboratory investigations revealed total count 8770/cumm, differential count: neutrophil 88%. Cerebrospinal fluid examination revealed 18 cells, lymphocyte: 99%, sugar 83 mg/dL and protein 21 g/dL. Suspected of partially treated/ viral meningitis, she was treated with antibiotics, steroids and antiviral drugs. Her computerized tomography brain showed ill-defined hypodensity in right and left frontal lobe (R>L), genu of corpus callosum suggestive of edema [Fig.1].
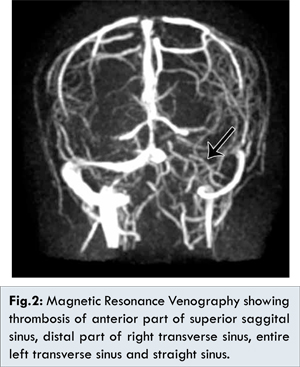
Anti-edema measures with antiepileptics were included. Her conscious level improved in 48 hours. Magnetic resonance venogram was done which revealed thrombosis of anterior part of superior sagittal sinus, distal part of right transverse sinus, entire left transverse sinus and straight sinus [Fig.2].
Injection low molecular weight heparin followed by oral anticoagulation was added. Because of persistent fever, repeat CSF examination was done which showed total count of 369 cells with lymphocytic predominance: L-96%, markedly elevated protein: 258 mg/dL, low glucose 38 mg/dL suggestive of tuberculous infection. Anti-tuberculous drugs (isoniazid, rifampicin, pyrazinamide, ethambutol) were added. The hypercoagulable state of TB meningitis resulting in cerebral venous thrombosis was considered. ATT, steroids, anticoagulants and antiepileptics were continued. Other causes of procoagulant state were ruled out. ANA, dsDNA, c-ANCA, p-ANCA, antiphospholipid antibody were negative. She showed remarkable improvement with repeat CT brain showed regression of cerebral edema [Fig.3].
Discussion
Cerebral venous thrombosis is more common in females in the age group of 20-35 years. It occurs mostly during pregnancy, puerperium and following intake of oral contraceptive pills. Common causes of prothrombotic conditions are either genetic or acquired, systemic lupus erythematosis, dehydration, malignancy and infection. Infection related septic cortical venous thrombophlebitis accounts for 6%-12% of cases, is more common following ear infection and sinusitis. Various etiologies for CVT have been proposed; still idiopathic CVT is seen in 13% cases [
1]. Mycobacterial infection especially, involving central nervous system and its relation with cerebral venous thrombosis is very rare. Mycobacterial infection increases the risk of CVT in a patient with prothrombin gene mutation [
2]. Other rare cause of CVT with lymphocytic meningitis is neurobrucellosis [
3].
CVT presents with three major syndromes: isolated intracranial hypertension syndrome (headache with or without vomiting, papilledema, and visual problems), focal syndrome (focal deficits, seizures, monoparesis or hemiparesis) and encephalopathy (multifocal signs, mental status changes, stupor or coma). There are reports of pulmonary, abdominal, neurologic presentation of tuberculosis with hypercoagulable state. Disseminated tuberculosis with pulmonary infiltrates, epididymitis, meningitis and associated cerebral venous thrombosis has been reported [
4,
5]. Few cases of tuberculous meningitis with CVT have been reported which includes one case of chronic granulomatous meningitis with multiple cranial nerve palsy [
6].
The hypercoagulable state in TB has been infrequently described in the literature. An association of deep vein thrombosis (DVT) and CVT with TB has been reported. The incidence of clinically apparent DVT has been reported to be 3% to 4% in adults with pulmonary TB [
7]. The true occurrence is possibly higher, due to asymptomatic DVT. Despite TB being widely prevalent in developing countries, data on the association with a hypercoagulable states are less, possibly reflecting less awareness of this association.
The pathogenesis behind the association of hypercoagulability in disseminated TB is the interaction of peripheral blood mononuclear cells with mycobacterial products inducing an increased synthesis of tumour necrosis factor-alpha and interleukin-6. These pro-inflammatory cytokines activate the vascular intima rendering the endothelium thrombogenic, inducing the hepatic acute-phase response, leading to deranged levels of coagulation proteins. Other proposed mechanisms are blood stasis in the intracranial sinus because of low-pressure system, increased platelet aggregability.
A transition G A at position 20210 is associated with elevated prothrombim concentration, mutation in this gene and presence of factor V Leiden mutation may increase 5-10 fold risk of venous thrombosis. However, both mutations when alone are not high risk factors for venous thrombosis. Arteries running though the subarachnoid space may show obliterative end-arterites with inflammatory infiltrates in their walls, and marked intimal thickening leading to endothelial injury of intracranial veins [
8]. Other hypercoagulable state and its association with CVT have been reported, such as anti-phospholipid antibodies, factor V leiden mutation, lupus anticoagulant. In our patient though she was in puerperal period, tuberculous infection added risk for causing CVT.
Conclusion
Infection related cerebral venous thrombosis is rare due to emergence of newer antibiotics. Patients with underlying hypercoagulable state such as pregnancy and puerperium, mycobacterial infection precipitates the occurrence of thrombotic events.
References
- Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004;35:664.
- Verma R, Lalla R, Patil TB, Tiwari N. A rare presentation of cerebral venous sinus thrombosis associated with tubercular meningitis. BMJ Case Rep 2013.
- Radwan Zaidan, Abdel-Rahman Al Tahan. Cerebral Venous Thrombosis: A New manifestation of Neurobrucellosis. Clinical Infectious Diseases. 1999;28:399-440.
- Pinto L, Ashok PP, Deshpande RB, Mahashur AA. Patient with Hypercoagulable State due to Tuberculosis. Indian J Chest Dis Allied Sci. 2009;51:49-51.
- Jose Antonio Fiorot Junior, Andre Carvalho Felício, Marcia Mauimi Fukujima, Celso Arraes Rodrigues, Vânia Maria Morelli, Dayse Maria Lourenço, et al. Tuberculosis: An uncommon cause of cerebral venous thrombosis? Arq Neuropsiquiatr. 2005;63:852-854.
- Finsterer J, Kladosek A, Nagelmeier IE, et al. Chronic granulomatous meningitis with multiple cranial nerve lesions hydrocephalus, stroke, sinus thrombosis, and epilepsy. South Med J. 2000;93:1108-1111.
- Robson SC, White NW, Aronson I, Woollgar R, GoodmanH, Jacobs P. Acute-phase response and the hypercoagulable state in pulmonary tuberculosis. Br J Haematol. 1996;93:943-949.
- Aundhakar SC, Mahajan SK, Mane MB, Agrawal S. Cortical venous thrombosis - a rare complication of tuberculous meningitis. Internet Journal of Medical Update. 2013;8:31-33.