Introduction
Cysticercosis is the infection caused by Cysticercus cellulosae, the larvae of the tapeworm Taenia solium, which affects humans mainly by accidental ingestion of eggs containing infective oncospheres [
1]. It is the most common parasitic disease of the central nervous system and endemic in our country [
1,
2].
We report a case of 42 year old male who presented with complaints of weakness of bilateral lower limbs since 3 months. Magnetic resonance imaging (MRI) showed a multilobulated intradural intramedullary cyst in thoracic cord with eccentric scolex at D9-D10 vertebral level and multiple ring enhancing lesions with eccentric scolex in brain. Based on a brief review of the literature, clinical and radiological aspects of spinal cysticercosis with differential diagnosis are discussed.
Case Report
A 42 year middle aged male was admitted with complaints of weakness of bilateral lower limbs since 3 months. Patient was apparently alright 3 months back when he had low backache. He developed weakness of limbs starting from left leg, then progressed to right leg after 15 days. He had log like sensation of both lower limbs. He had no bowel/bladder involvement.
For his complaints patient underwent MRI lumbosacral spine performed on 1.5 Tesla Magnetom Avanto, Siemens using an oval spine coil. T1-weighted (TR/TE/n=550/15/3) and T2-weighted (TR/TE/n=2200/20,80/1) images were obtained in sagittal plane and axial plane with a slice thickness of 3 mm interslice gap of 0.3 mm, and a 256 x 256 matrix. Post-contrast T1 weighted images were obtained after injection of Gd-DTPA in the dose of 0.1 mmol/kg bodyweight. Brain MRI was done by using head coil with axial images with slice thickness of 5 mm, interslice gap 0.5 mm, and matrix 192 x 256 matrix.
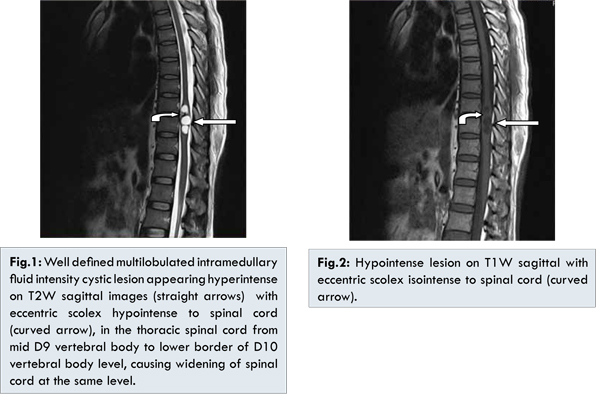
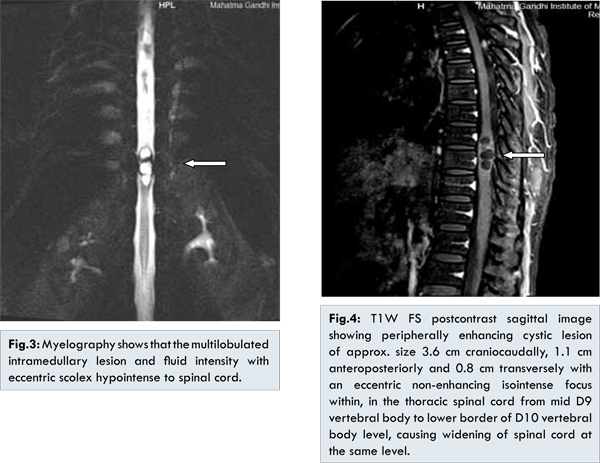
Spinal MR images fig.1 to fig.4 showed a well-defined multi-lobulated intramedullary peripherally enhancing cystic lesion of approx. size 3.6 cm craniocaudally, 1.1 cm anteroposteriorly and 0.8 cm transversely with an eccentric non-enhancing focus within iso-intense to cord, in the thoracic spinal cord from mid D9 vertebral body to lower border of D10 vertebral body level, causing widening of spinal cord at the same level. On T2W images [Fig.1] and T1W image [Fig.2], cyst fluid was isointense to cerebrospinal fluid (CSF) and there was an eccentric nodule isointense to cord within the cyst on T1W images [Fig.2]. The lesion showed ring enhancement on contrast study [Fig.4]. These features were suggestive of vesicular stage of cysticercosis.
Due to diagnostic difficulty, MRI brain was also performed, and fig.5 to fig.7 revealed similar multiple lesions within the brain parenchyma at grey-white matter junction in bilateral occipital, left frontal, right lentiform and bilateral parietal regions suggestive of neurocysticerosis, again in vesicular stage.
Discussion
The usual way in which NCC involves the spinal cord is from an extramedullary (racemose) formation, as a result of dissemination of the vesicles through the subarachnoid space from the posterior cranial fossa [
3]. Intramedullary cysticercal involvement usually solitary, most probably occurs through arterial circulation. The site of infection could be proportional to regional blood flow and this would help explain why the most common region of intramedullary cysticercosis is thoracic, followed by cervical, lumbar and sacral regions [
1]. The neurological consequences of spinal cord involvement in NCC are due to two different mechanism different mechanisms: irritation and mass effect [
3,
4].
The progression of the spinal cord lesion begins with inflammation due to the presence of the parasitic toxin [3,4]. The resultant mass effect causes spinal cord compression syndrome, caused by the increase in the size of vesicles [
3]. Finally arachnoiditis fibrosa leads to medullary vascular insufficiency [
3]. Inflammatory reaction against the dead parasite is associated with perilesional edema, which can damage medullary parenchyma [
1]. Obstruction of cerebrospinal fluid pathways due to scarring of the subarachnoid space can also cause symptoms [
2].
Differential diagnosis of an intramedullary cystic lesion in a patient presenting with back pain is extensive and includes neoplastic (e.g. ependymoma), infectious (e.g. abscess), inflammatory (e.g. multiple sclerosis), post-traumatic spinal cord changes (e.g. syringomyelic cavitation), parasitic infestations (e.g. hydatid cysts) [
1]. The presence of eosinophils in the cerebrospinal fluid may be taken as strong evidence of parasite disease [
5].
MRI can identify characteristic features of intramedullary cysticercosis [
6] and this is of great diagnostic importance. It is the preferred image method for visualization of intramedullary lesions and also correlates with cysticercal pathological stages (vesicular, colloidal vesicular, granular nodular and calcific nodule) [
1]. On MRI, intact intramedullary cysts in vesicular stage typically shows cystic areas within the substance of spinal cord with intensity of cyst fluid similar to that of CSF on both T1 and T2-weighted images [Fig.1,2]. A subtle hypointense rim may surround the intramedullary cyst on T2-weighted images. Occasionally the scolex can be identified as a mural nodule within the cyst cavity on T1-weighted images [Fig.2]. The scolex is isointense to spinal cord parenchyma on T1-weighted acquisitions and may not be visualized on T2-weighted images because it becomes isointense to the surrounding cyst fluid. As in the brain, degenerating cysticercotic cysts within the spinal cord may show evidence of irregular peripheral enhancement after IV gadolinium administration [
7]. Surrounding perilesional edema is seen in colloidal vesicular and granular nodular stages, sometimes in nodular calcified stage. Lesions in nodular calcified stage appear hypointense on all MRI sequences with no contrast enhancement. MR myelography also shows the intramedullary location of the lesion [Fig.3]. Similar cystic lesions were demonstrated in our case in the thoracic spinal cord from mid D9 vertebral body to lower border of D10 vertebral body level, causing its widening along with concomitant lesions in brain. Sequences like STIR and FLAIR further confirmed the fluid signal intensity of the lesion. Spinal cysticercosis seems to almost always be associated with concomitant intracranial involvement, although isolated spinal involvement has been described [
7].
According to the American Society for Microbiology Current Consensus Guidelines for Treatment of Neurocysticercosis, the treatment of spinal cysticercosis, intra- or extramedullary, is primarily surgical [
8]. Postoperative treatment with anticysticercal agents would be warranted. Our patient was given a course of albendazole, an anticysticercal agents with dexamethasone to attenuate treatment-associated inflammatory reactions, however as the spinal lesion showed no response, he was managed surgically. Postoperatively patient showed improvement in his signs and symptoms with no complications.
Conclusion
MRI is the imaging modality of choice for spinal and neural cysticerosis as it can detect the location of lesion whether intramedullary or extramedullary, confirm the stage of the cysticerosis (vesicular, colloidal vesicular, granular nodular and calcific nodule), help in monitoring response to treatment as well as postoperative follow up.
References
- Guedes-Correa JF, Macedo RC, Vaitsman RP, Mattos JG, Agra JM. Intramedullary spinal cysticercosis simulating a conus medullaris tumor: case report. Arquivos de neuro-psiquiatria. 2006;64(1):149-152.
- Alsina GA, Johnson JP, McBride DQ, Rhoten PR, Mehringer CM, Stokes JK. Spinal neurocysticercosis. Neurosurgical Focus. 2002;12(6):e8.
- Isidro-Llorens A, Dachs F, Vidal J, Sarrias M. Spinal cysticercosis. Case report and review. Paraplegia. 1993;31(2):128-130.
- Colli BO, Assirati Junior JA, Machado HR, dos Santos F, Takayanagui OM. Cysticercosis of the central nervous system. II. Spinal cysticercosis. Arquivos de neuro-psiquiatria. 1994;52 (2):187-199.
- Hesketh KT. Cysticercosis of the dorsal cord. Journal of neurology, neurosurgery, and Psychiatry. 1965;28(5):445-448.
- Gaur V, Gupta RK, Dev R, Kathuria MK, Husain M. MR imaging of intramedullary spinal cysticercosis: A report of two cases. Clinical Radiology. 2000;55(4):311-314.
- Leite CC, Jinkins JR, Escobar BE, Magalhaes AC, Gomes GC, DibG, et al. MR imaging of intramedullary and intradural-extramedullary spinal cysticercosis. American Journal of Roentgenology. 1997;169(6):1713-1717.
- Garcia HH, Evans CA, Nash TE, Takayanagui OM, White AC Jr, Botero D, et al. Current consensus guidelines for treatment of neurocysticercosis. Clinical Microbiology Reviews. 2002;15(4):747-756.