Introduction
Imperforate hymen is the commonest female genital tract malformation and the incidence is approximately 1 in 2000 females [
1]. Imperforate hymen, is a condition where the hymen, a thin membrane in the shape of a half moon, covers the entire opening of the vagina [
2]. There can be delayed diagnosis of this condition as the patient remains asymptomatic for a long time and if symptomatic can present with one or many, of a variety of symptoms. Symptoms can range from mild abdominal pain and tenesmus to urinary retention and a palpable lump in abdomen due to hematometra, hematocolpos or hydrocolpos. Haematocolpos is a rare condition seen with imperforate hymen or vaginal atresia in peripubertal age, where the vagina is filled with menstrual blood [
3]. In hydrocolpos, secretions are believed to result from the maternal estrogen effect on the vaginal and/or cervical glands and are mostly seen in newborn. Although the most common age of presentation of imperforate hymen is around puberty, diagnosis in-utero and during the newborn period and childhood are also reported. Mostly imperforate hymen is sporadic in nature but there are reports of familial cases showing dominant as well as recessive inheritance [
4]. In this case we present a young female of 13 years old with acute urinary retention and large palpable lump in abdomen as a result of imperforate hymen.
Case Report
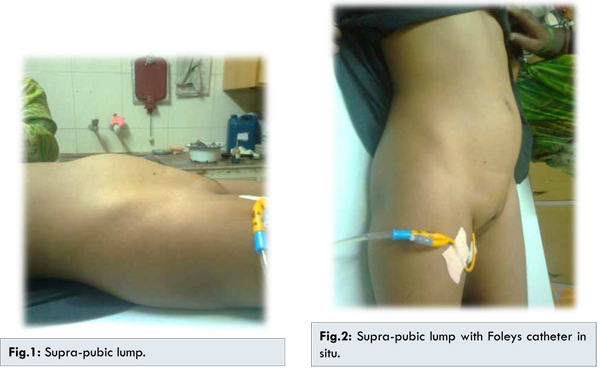
A 13 year old pre-menarchal female presented to the emergency department with history of acute urinary retention since 6 hours associated with suprapubic pain. She also gave history of lump in lower abdomen since last 4 months, which gradually increased to present size [Fig.1]. There was history of cyclical colicky lower abdominal pain with backache since last 6 months for which she took medication from local hospital. For last one month there was increased frequency and difficulty in micturition. She denied any poor oral intake, nausea, vomiting or problem with bowel movements. There was no previous history of urinary retention or trauma or any surgery. Her birth history and developmental history were unremarkable. Here secondary sexual characters were well developed. On routine blood investigations, hemoglobin was 8.5 gm%, total leucocyte count was 13,400/mm3 and renal function test were within normal limits. She was catheterized with 10 french unit (fr) Foleys catheter, which drained 700 cc clear urine. Here suprapubic pain was relieved after catheterization. On abdominal examination, suprapubic mass corresponding to approximately 14 weeks pregnant uterus was palpable [Fig.2]. The mass was arising from pelvis and had mild tenderness and was cystic on palpation.
Perineal examination revealed normal external urethral opening and a bulging bluish colored bulge with a covering membrane over the vagina [Fig.3]. The bulge in perineum was exaggerated on pressing the suprapubi clump and by performing Valsalva maneuver [Fig.4]. The mass was found to be anterior to rectum and was cystic on per rectal examination.
The ultrasonography of abdomen and pelvis reported an 11.5x8x7.2 cm3 large fluid collection with fine internal echos (suggestive of blood) in dilated and enlarged vagina and uterus and was not related to bowel [Fig.5]. The cervical canal was seen widely open. There was no free fluid in peritoneal cavity. These findings were suggestive of hematocolpos and hematometra. Bilateral mild hydroureteronephrosis was noted on renal ultrasound.
After proper anesthetic evaluation she was posted for surgery. Needle aspiration from the bulging hymenal membrane confirmed the aspirate as collected blood. A cruciate incision was taken through the membrane which drained approximately 700 cc of collected chocolate colored blood passively, suggestive of menstrual products. After drainage the suprapubic lump disappeared. The incised quadrants of the hymenal membrane were excised laterally. Margins of vaginal mucosa were approximated with absorbable vicryl sutures [Fig.6].
Local analgesic cream and intravenous antibiotic were given. She had an uneventful postoperative period and was discharged on 4th day after removal of the catheter. She had menstruation after two months and is asymptomatic in follow up examination.
Discussion
The hymen is a vestigial membrane at the junction between the sinovaginal bulb and the urogenital sinus. Normally it ruptures partially at the inferior portion during 8th week of gestation to establish connection between the vaginal lumen and exterior. When there is complete failure to of the inferior end of the vaginal plate to canalize, then diagnosis of imperforate hymen is made. Hymen provides innate immunity as it provides barrier to ascending infections [
5]. Imperforate hymen is rarely associated with other female genital tract malformations but Mullerian duct malformations should be ruled out. Although it is mostly found in pubertal females, it can also be diagnosed with help of obstetric ultrasonography in fetus and in newborn by careful examination of the perenium. On ultrasonography findings of such as hematocolpos, hematometra, hematosalpinx, or hydrometrocolpos in newborn, suggest the diagnosis. Commonly pubertal girls present after menarche when menstrual blood trapped in the vagina behind the imperforate hymen which is known as hematocolpos creating a bluish bulge at the introitus. With cyclic menstruation, the vaginal canal becomes greatly distended, and the cervix may begin to dilate and allow formation of a hematometra and hematosalpinx thus forming lump in abdomen. This can lead to mass effect causing to urinary outflow obstruction or rarely intestinal obstruction. The largest reported size of hematocolpometra mass in a imperforate hymen case was of 24x12x16 cm3 on ultrasonography by Joanna Mercado-Alvarado et al. [
11]. If patient or parents refuse genital exam evaluation, imaging studies can greatly help with diagnosis. According to Lui et al. [
6] mean age of presentation is 12 years and 13.2 years by Liang et al. [
7].
The common mode of presentation of imperforate hymen includes (i) Amenorrhea, which may be primary due to obstruction by imperforate hymenal membrane. (ii) Recurrent cyclical lower abdominal/pelvic pains due to continued distension of the vagina and uterus by accumulating menstrual blood [8]. (iii) Acute urinary obstruction due to compression effect by the lump on urethra and angulation of the bladder neck [9]. (iv) Chronic urinary retention causing hydroureteronephrosis leading to renal failure in long term [
10]. (v) Lymphovenous obstruction and intestinal obstruction in rare cases. The differential diagnosis of imperforate hymen includes lower transverse vaginal septum, distal vaginal atresia, complete vaginal atresia, phimosis of the cervix and mucocolpos.
In cases of imperforate hymen presenting with urinary retention, retention should always be treated via Foleys catheterization until definitive treatment via hymenotomy can be achieved. Because hymen is a symbol of virginity, its destruction during hymenotomy can lead to social problems for girls [
12]. Different types of incision are proven effective for hymentomy in literature such as cruciate incision, longitudinal incision, or excision of part of membrane. Hymenotomy is a minor procedure that does not cause significant morbidity and provides complete relief of all the symptoms. Follow up is always necessary to make sure there is no refusion of the hymen.
Conclusion
Even though imperforate hymen is the most common congenital abnormality of the female genital tract, it is a rare cause of acute urinary retention or abdominal pain in children and adolescents. It is a diagnosis that can easily be overlooked in the fast paced setting of the Emergency Department. It must be included, particularly, in the differential diagnosis of every pre-pubertal young female with abdominal pain or acute urinary retention. Hymenotomy, a simple surgical procedure is all that needed for the treatment of imperforate hymen patients who can present with acute surgical emergency.
References
- Schorge JO, Schaffer JI, Halvorson LM, Hoffman B, Bradshaw K. Anatomic disorders. In: Schorge JO (eds). Williams Gynecology. 1st ed. New York: McGraw Hill Medical; 2008:412-413.
- Children’s Hospital Boston (2013) Imperforate hymen. Retrieved From. Dickson CA, Saad S, Tesar JD. Imperforate hymen with hematocolpos. Annals of Emergency Medicine. 1985;14:467-469.
- Deligeoroglou E, Iavazzo C, Sofoudis C, Kalampokas T, Creatsas G. Management of hematocolpos in adolescents with transverse vaginal septum. Archives of Gynecology and Obstetrics. 2012;285(4):1083-1087.
- Sakalkale R, Samarakkody U. Familial occurrence of imperforate hymen. Journal of Pediatric and Adolescent Gynecology. 2005;18:427-429.
- Basaran M, Usal D, Aydemir C. Hymen sparing surgery for imperforate hymen: case reports and review of the literature. J Pediatr Adolesc Gynecol. 2009;22(4):61-64.
- Lui CT, Chan TWT, Fung HT, Tang SYH. A retrospective study on imperforate hymen and hematocolpos in a regional hospital. Hong Kong J Emerg Med. 2010;17(5):435-440.
- Liang CC, Chang SD, Soong YK. Long-term follow-up of women who underwent surgical correction for imperforate hymen. Arch Gynecol Obstet. 2003;269:5-8.
- Dane C, Dane B, Erginbas M, Cetin A. Imperforate hymen-a rare cause of abdominal pain: two cases and review of the literature. J Pediatr Adolesc Gynecol. 2007;20(4):245-247.
- Ercan CM, Karasahin KE, Alanbay I, Ulubay M, Baser I. Imperforate hymen causing hematocolpos and acute urinary retention in an adolescent girl. Taiwan J Obstet Gynecol. 2011;50(1):118-120.
- Nagai K, Murakami Y, Nagatani K, Nakahashi N, Hayashi M, Higaki T, et al. Life threatening acute renal failure due to imperforate hymen in an infant. Pediatr Int. 2012;54(2):280-282.
- Mercado-Alvarado. Imperforated Hymen: An Unexpected Cause of Pediatric Abdominal Pain: Case Report and Review of Literature. Trop Med Surg. 2013;1:5.
- Abu-Ghanem S, Novoa R, Kaneti J, Rosenberg E. Recurrent urinary retention due to imperforate hymen after hymenotomy failure: a rare case report and review of the literature. Urology. 2011;78:180-182.