Introduction
Metastatic tumors of oral soft tissue are very rare, but it is a major morbidity in a cancer patient. It is reported that metastatic oral cancers are only 1%-8% among all oral cancers [
1]. Soft tissue involvement is mainly due to direct extension of the bone tumors of jaw. Gingiva is the most common site among oral cavity soft tissue for metastases [
2,
3]. We are presenting a case of Ewing sarcoma metastasizing to lower gingiva.
Case Report
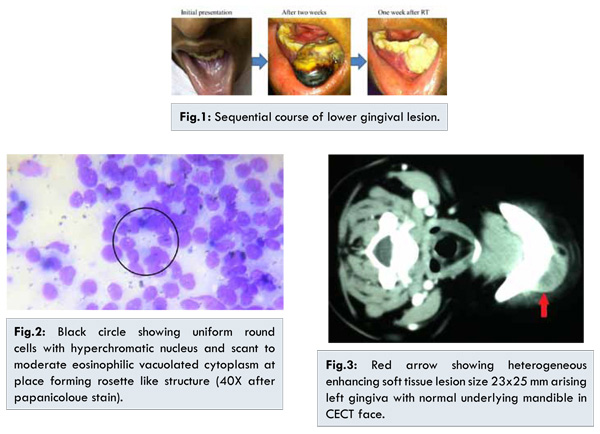
An 11-year old male child presented with pathological fracture of right fibula which was later diagnosed as Ewing’s sarcoma on histology. Metastatic workup was normal. Patient received four cycle of neo-adjuvant chemotherapy (VAC-IE) following which he underwent fibulectomy. Post-operatively he completed five more chemotherapy cycles as per POGS protocol for the duration of 51 weeks and, than he also received local external beam radiotherapy (60 Gy). After one year, he presented with an ulcer over the previous surgery scar which was fixed to the underlying tibia. PET-CT showed increased activity suggesting local recurrence for which he received six cycles of second line chemotherapy (tamozolomide + irinotecan) and underwent limb salvage surgery which has failed and below knee amputation was done. After five year of primary, he developed a swelling over lower gums, which was soft, free from bone and tender [Fig.1]. FNAC showed small round cells suggestive of metastatic Ewing’s sarcoma to gingiva [Fig.2]. CECT head and neck showed a hypodense lesion in gingiva of size 2.6x2 cm with normal underlying mandible [Fig.3]. Within three weeks, it doubled in size with blackish discoloration of mucosa. For the gingival lesion patient received radiotherapy 30 Gy in 10 fractions and it reduced by half within 1 week and then completely sloughed out. After that, he received palliative chemotherapy to control the symptoms.
Ewing sarcoma is a round cell tumor, primarily arising in skeletal system, which accounts for 4% to 10% of all bone tumors mainly in lower extremity. Among all oral malignancies, incidence of metastatic tumors is only about 1%-8%, and fewer among jaw tumors as 1% [
1,
3]. It mainly occurs in the posterior mandibular region, for more than 70% of all oral metastases [
4].
The epidemiological features vary in all reported cases. There is major difference of metastatic lesions between bone (65%-75%) and oral soft tissue (25%-35%) [
5]. This difference is due to preferential metastatic site of the specific primary tumor. In younger patients, jaw bones are more common for metastases compared to soft tissues. The primary tumors from the lung, breast, kidney and prostate prefer commonly to metastasize to skeleton rather than soft tissues of the oral cavity. The hematopoietic tissue of jaw bones is sinusoidal that favour easy penetration of the tumor cells. Gingiva is the most common site among oral cavity soft tissues (57%), followed by tongue (27%), tonsil (8%), palate, (4%), lip (3%), buccal mucosa (1%) and floor of mouth (1%) [
2,
3]. Usually, gingival or oral mucosal metastases occurs due to direct spread from mandibular or maxillary lesions or disruption of the periosteum to cause visible mass. Bone metastases to jaw from Ewing sarcoma is well reported, but only single case has been reported in English literature by McGlumphy et al. [
6]. The common primary sites causing oral cavity metastases are lung, kidney, bone, liver and prostate for men; and breast, lung, genital organs, kidney, and colo-rectum for women [
1,
2,
7].
The pathophysiology of metastases is a complex biological process that includes detachment from the surrounding cells, regulation of cell motility, invasion, survival, proliferation and evasion of the immune system [
8]. There are several pathways of oral soft tissue metastases. Haematogenous spread is through inversion of the cervical Batson’s plexus venous flow. Alternatively, the retrograde migration of exfoliating cancer cells from primary or metastatic lesions of lung occurs which implants in the oral mucosa [
9].
The common clinical symptoms are rapidly progressive swelling with pain, or paraesthesia. Initially, it appears as hyperplastic or reactive lesion such as pyogenic granuloma, peripheral giant cell granuloma or fibrous epulis. The rapid progressive gingival swelling in a previously diagnosed or treated cancer patient is more in favour of metastatic lesion than benign lesion [9]. Morphologically it appears as soft, polypoid or exophytic and highly vascularized mass [
8]. The chronic inflammation of gingiva increases the capillary network, which slows the blood flow which favours the condition for metastases, including cellular transformation, promotion, survival, proliferation, invasion and angiogenesis [
3]. The preference of gingival metastases of maxilla rather than mandible is still unclear [
2].
In our case, there was a painful rapidly increasing swelling without paraesthesia. However, metastases to the oral cavity are in 20%-35% of cases the first indication of an otherwise occult malignancy [
1]. It can present as first presenting feature of an occult malignancy in 20%-35% of cases which is challenging to diagnose [
5]. Fine needle aspiration is the best option to prove the diagnosis as in our case [
8]. The average duration from the diagnosis of primary cancer and metastases is too long with a wide range of 2 to 13 years which was five years in our case. The purpose of the treatment is mainly palliative, to reduce the pain and control bleeding. Radiotherapy is the best option available response which is effective within a short duration [
10]. In our case, after radiotherapy size decreased by more than 50% and requirement of analgesia also reduced significantly. The median survival with gingiva metastatic tumors is very poor, about 4 to 6 months is reported in literature with less than 5% of five-year survival [
10].
Conclusion
Gingival metastases arises from skeletal Ewing’s sarcoma is an extremely rare case. Although, its early recognition and local treatment by radiotherapy helps in improving quality of life but it carries a poor prognosis.
Acknowledgement
We are thankful to patient’s father to give consent for the publication and his patience for that kind of repairable loss.
References
- Van-der-Waal RI, Buter J, van-der Waal I. Oral metastases: review of 24 cases. Br J Oral Maxillofac Surg. 2003;41:3-6.
- Seoane J, Van der Waal I, Van der Waal RI, Cameselle-Teijeiro J, Anto´n I, Tardio A, et al. Metastatic tumours to the oral cavity: a survival study with a special focus on gingival metastases. J Clin Periodontol. 2009;36:488-492.
- Hirshberg A, Leibovich P, Buchner A. Metastatic tumors to the jawbones: analysis of 390 cases. J Oral Pathol Med. 1994; 23:337-341.
- Ancieto GS GarcíaPeñín A, de la Mata Pages R, Montalvo Moreno JJ. Tumors metastatic to the mandible: analysis of nine cases and review of the literature. J Oral Maxillofac Surg. 1990;48:246-251.
- Jham BC, Salama AR , McClure SA, Ord RA. Metastatic Tumors to the Oral Cavity: A Clinical Study of 18 Cases. Head and Neck Pathol. 2011;5:355-358.
- McGlumphy EA, Zysset MK, Montgomery MT. Ewing’s sarcoma metastatic to the gingiva. J Oral Maxillofac Surg. 1987;45:444-447.
- Hirshberg A, Buchner A. Metastatic tumours to the oral region. An overview. Eur J Cancer B Oral Oncol. 1995;31B:355-360.
- Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Metastatic tumors to the oral cavity-pathogenesis and analysis of 673 cases. Oral Oncol. 2008;44:743-752.
- Chossegros C, Blanc JL, Cheynet F, Bataille JF, Tessier H. Metastatic localization in the buccal cavity: case report and literature review. Rev Stomatol Chir Maxillofac. 1991;92:160-164.
- Watanabe E, Touge H, Tokuyasu H, Kawasaki Y. Gingival metastasis of adenocarcinoma from the lung. Respiratory Medicine CME. 2008;1:103-106.