Introduction
Ovary hyperstimulation syndrome (OHSS) is generally an iatrogenic complication of assisted reproductive technology (ART) with exogenous gonadotropins. It is a serious and potentially life-threatening physiological complication that is characterized by insufficient blood volume and hypercoagulation. Severe forms such as thromboembolic complications, renal failure and severe respiratory failure are observed in 0.5%-5% of women treated with ART [1]. This is one of the few reported cases that illustrates the delivery of healthy baby in patient of cerebral vein thrombosis secondary to OHSS. This is the first in our hospital since 2000.
Case Report
A 38-year-old woman presented with secondary infertility for 10 years. She had an irregular menstrual history, with menstrual cycle 32-37 days and mild to moderate dysmenorrhea. Her basal FSH was 10.06 U/L, and CA125 elevated as 106.2 U/L.
The couple came for assisted reproductive technology because of male factor infertility. Sperm routine test showed that total sperm concentration (TSC) 2.6 M/ml and PR (progressive rate) 16% and second check showed that TSC<2M/ml. The karyotype of male was normal (46,XY). Her physical and gynecological examinations, body mass index (BMI) 19.5 kg/m2 were unremarkable. Antral follicle count was 4 in left ovary and 5 in right ovary. The patient was allergic to sea food.
The women underwent ultra-long protocol intracytoplasmic sperm injection (ICSI) in our center. After two doses of gonadotropin releasing hormone agonist (GnRHa), Gonadotropin 150U per day was administered for 13 days. Recombinant human chorionic gonadotrophin (rHCG) (Ovidrel) 250 µg was given when at least 3 follicles =17 mm in diameter were seen by transvaginal ultrasound monitoring. Serum E2 was more than 4862 pg/mL. Follicular puncture was performed 36 hours after the hCG administration. Eighteen oocytes were recovered, 18 of which were at the metaphase II stage and were microinjected with ejaculatory spermatozoa. 7 oocytes were normally fertilized. Three fresh embryos with good score (6, 7, 8-cell stage and grade 2) were transferred on day 3. The other 3 embryos were cryopreserved. The patient received luteal phase progesterone supplementation (P in oil, 60 mg IM daily). The patient came back in clinic at 9 days after embryo transfer (ET) and complained of nausea, decreased appetite, increasing abdominal distension and decreased urine output for last 3 days. This was not accompanied by dyspnea, vomiting, headache or dizziness. Transabdominal ultrasound showed that right ovary 72x59 mm, left ovary 57x51 mm, moderate ascites with depth of 45 mm. Urine routine test showed that specific gravity (SG) 1.028, with negative red blood cell (RBC) and white blood cell (WBC) and protein (PRO). Table 1 mentions routine hematological and hypercoagulability screening results. The patient was diagnosed as moderate OHSS with early pregnancy and advised hospitalization. Human albumin 10 g and hydroxyethyl starch 500 ml were prescribed. About half an hour after admission in the ward, the patient suddenly suffered syncope for few seconds without predisposing factors and followed by symptoms of dizziness and corner to the right skew and left upper limb weakness. The patient vital signs were as follows: respiratory rate 20/min, heart rate 88 beat/min, blood pressure 125/75 mmHg, and body temperature 36.3°C.
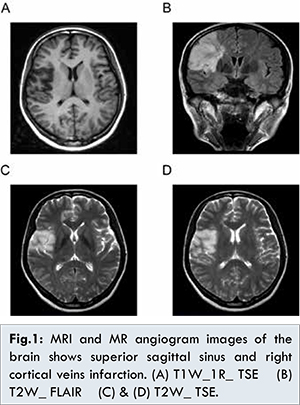
Neurology consultation was acquired immediately and turned to nerve internal medicine treatment. Neurological examination showed intact consciousness with normal vision and language function, and a left-sided hemiparesis. Muscle strength was zero in the left upper limb and grade 5- in the left lower limb. Intracranial bleeding was ruled out by emergency cranial computed tomography (CT). Ischemic cerebral apoplexy was diagnosed. Nuclear magnetic resonance (NMR) examination demonstrated embolism in the right forehead frontal and parietal part, as well as thrombosis of the superior sagittal sinus and right cortical veins [Fig.1]. The head MRI+A+V showed acute cerebral infarction in right frontal parietal lobe; right basal ganglia, right half oval central cerebral infarction, and MRA and MRV were not clearly abnormal. The quantitative measure of ACA IgG was increased and PS was decreased in coagulation profile [Table 1].
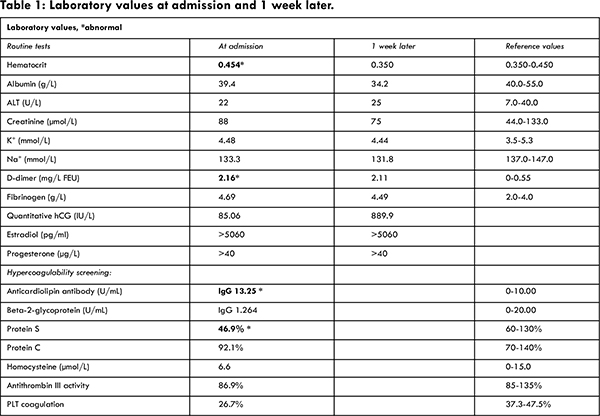
In view of the diagnosis of cerebral vein thrombosis, considering pregnancy may exaggerate the severity of thrombosis and some vital medicine may be teratogenic, patient was advised to terminate pregnancy as soon as possible several times. However, the couple deeply understood the related risks; they were eager to have a baby and refused to terminate pregnancy. The patient decided to continue with pregnancy despite the risk of recurrent stroke. At the same time, all the luteal supplementation protocol was withheld and patient was continued on anticoagulant and rehabilitation therapy. The patient was treated with low-molecular-weight heparin subcutaneously twice daily. Serum hCG was 469.85 IU/L at 13 days after embryo transfer. Transvaginal ultrasound showed a single gestation sac and heart beat at 4 weeks after embryo transfer (ET). Abdominal circumference and total amount of fluid in and out were closely monitored. Abdominal ultrasound showed the ovaries had increased in size with ascites effusion depth to 87.4 mm, while the symptoms of OHSS were relieved mostly. Laboratory results 1 week after admission are showed in Table 1. Twelve days after admission, the patient was symptomatically better with improvement of muscle power to grade 5 in all four limbs and hemiparesis. Given her general good condition, she was discharged from the hospital. Aspirin enteric-coated tablets and clopidogrel were prescribed for 2 weeks. The patient was suggested to have regular follow-up visit at neurological clinic and obstetric outpatient department. Anticoagulation was continued for the duration of her ongoing pregnancy until 3 days before termination of pregnancy. The nuchal translucency (NT) examination was normal but Down’s syndrome screening by blood test was at high risk (1/10, normal range<1/250). Therefore, transamniotic puncture was done, and the fetal karyotype was 46, XY (Y=21). All the transabdominal obstetric ultrasound results were normal. At 38+2 weeks, the patient delivered a healthy 2.89 kg boy by Cesarean section. Apgar score was 10, 10 at 1 minutes and 5 minutes respectively.
Discussion
OHSS is an iatrogenic complication of ART generally with exogenous gonadotropins, although there were natural conceptions of OHSS as case reports [2]. The exact etiopathogenesis is not completely understood, common risk factors predisposing for the development of OHSS are younger age, low body mass index, PCOS, allergy, retrieval of more than 20 oocytes, higher doses of exogenous gonadotropins, high serum E2 levels, conception and previous history of OHSS [3]. However, there were no significant risk factors of OHSS in this reported case. The shift of fluids into the extracellular space leads to intravascular depletion and hemoconcentration, which is associated with increased blood viscosity and coagulation [4]. OHSS is characterized by some important features including marked ovarian enlargement, ascites, pleural effusion, renal and liver dysfunction, and rarely thromboembolic complications [5].
OHSS is self-limiting, and treatment is primarily supportive with an aim to reduce the incidence of associated complications. Intensive care may be required for management of thromboembolic complications [6-8], renal failure and severe respiratory failure. To our knowledge, there have been only very few studies in English language medical literature that describe cerebral venous thrombosis [9,10]. The studies seldom report good prognosis. In our center, since year 2000, of 13000 infertile couples, this case was the first and only case of cerebral venous thrombosis secondary to OHSS.
OHSS incurs a 100 fold increase in risk of venous thrombosis over natural conceptions [3]. Venous thrombosis is usually related to one of three factors: reduced blood flow, changes in vessel wall integrity, or changes in the blood composition [4]. Factors leading to thrombosis are classified as either genetic or acquired. Puerperium and oral contraceptives are examples of the acquired factors. Protein C and S deficiency accounted for some cases of the congenital thrombophilia. As shown in this case, protein S was lower than the normal range.
The risk of thrombosis during pregnancy is high compared to that in the overall population. As in IVF-ET cycle, superphysiological high-level plasma estrogen is crucial in the blood coagulation activity that results in the occurrence of thrombosis. With the use of reproductive hormones and as a consequence of ovarian stimulation, patients in IVF-ET cycles are at high risk of thrombosis [11,12]. The incidence of thromboembolic events is 0.2%-0.4% in-vitro fertilization cycles and 10%-12% in severe OHSS [13]. Pregnancy is closely associated with a hypercoagulable state that predisposes to thrombosis, increased especially in patients with OHSS [12]. Simultaneously, neurologist and obstetric doctor interviewed the couple several times, explaining the risk about hypercoagulation during ongoing pregnancy which may exaggerate stroke. Luckily, no complication occurred during pregnancy although the ultra-long protocol was used and the luteal progesterone supplementation was stopped since stroke occurred.
Prevention of venous thrombus embolism (VTE) during pregnancy should be offered to women with specific risk factors. And it is recommended that prophylactic anticoagulation be considered for all patients with severe disease. Although thromboembolic events are not frequently encountered in the course of OHSS, they are strikingly serious in a proportion of affected patients,
and we agree with the recommendation by Grygoruk, et al. that anticoagulant therapy should be prophylactically administered in all OHSS patients [14]. In the case of thromboembolism related to OHSS in a pregnant patient, there is currently no indication to terminate a pregnancy that results in OHSS. Pregnancy sometimes is terminated due to progressive thrombosis and further complications despite anticoagulation therapy. Earlier diagnosis, intensive monitoring and institution of supportive therapy may help in preventing complications.
Conclusion
Physicians should be aware of the increased risks of VTE and the need to take a careful medical history to identify additional co-existing risks, and should be able to diagnose VTE and know how to approach its prevention.
References
- Nicolini A, Perazzo A, Gatto P, Santo M, Bonfiglio M. Acute respiratory failure following ovarian hyperstimulation syndrome. Italian Journal of Medicine. 2013;7:43-47.
- Sridev S, Barathan S. Case report on spontaneous ovarian hyperstimulation syndrome following natural conception associated with primary hypothyroidism. J Hum Reprod Sci. 2013; 6(2):158-161.
- Nelson SM.Venous thrombosis during assisted reproduction: novel risk reduction strategies. Thromb Res. 2013;131: Suppl 1:S1-3.
- Garcia-Velasco JA, Pellicer A. New concepts in the understanding of the ovarian hyperstimulation syndrome. Curr Opin Obstet Gynecol. 2003;15:251-256.
- Vloeberghs V, Peeraer K, Pexsters A, d’Hooghe T. Ovarian hyperstimulation syndrome and complications of ART. Best Pract Res Clin Obstet Gynaecol. 2009;23:691-709.
- Bartkova A, Sanak D, Dostal J, Herzig R, Otruba P, Vlachova I, et al. Acute ischaemic stroke in pregnancy: a severe complication of ovarian hyperstimulation syndrome. Neurol Sci. 2008; 29:463-466.
- Alasiri SA, Case AM. Thrombosis of subclavian and internal jugular veins following severe ovarian hyperstimulation syndrome: a case report. J Obstet Gynaecol Can. 2008;30:590-597.
- Ravel P, Marcaggi X, Ferrier N, Vignancour S, Clerfond G, Boch C, et al. Myocardial infarction and ovarian stimulation:Case report. Annales de Cardiologie et d’Ang_eiologie. 2009;58:313-317.
- Zhao Jing, Li Yanping. Middle cerebral artery thrombosis after IVF and ovarian hyperstimulation: a case report. Fertility and Sterility. 2011;95(7):2435.e13-e15.
- BL Man, ACF Hui. Cerebral venous thrombosis secondary to ovarian hyperstimulation syndrome. Hong Kong Med J. 2011;17:155-156.
- Ohashi R, Sugimura M, Kanayama N. Estrogen administration enhances thrombin generation in rats. Thromb Res. 2003;112(5-6): 325-328.
- Chan WS, Ginsberg JS. A review of upper extremity deep vein thrombosis in pregnancy: unmasking the ‘ART’ behind the clot. J Thromb Haemost. 2006; 4(8):1673-1677.
- Rova K1, Passmark H, Lindqvist PG. Venous thromboembolism in relation to in vitro fertilization: an approach to determining the incidence and increase in risk in successful cycles. Fertil Steril. 2012;97(1):95-100.
- Grygoruk C, Mrugacz G, Grusza M, Grusza-Golatowska I, Stasiewicz-Jarocka B, Pietrewicz P. Thrombosis in the course of ovarian hyperstimulation syndrome. Med Wieku Rozwoj. 2012;16(4):303-306.