Introduction
Eye movements bring visual stimuli to the fovea and maintain fovea fixation on a moving target or during head movements. These movements are performed by the ocular motor system that consists of ocular motor nerves and brainstem nuclei. The ocular motor system is classified according to anatomic location into infranuclear, nuclear, internuclear, and supranuclear components [
1]. Supranuclear disorders result from lesions above the level of the ocular motor nerve nuclei and account for almost 10% of all patients with disorders of eye movements [
1-
4]. Supranuclear disorders are characterized by gaze palsies, tonic gaze deviation, saccadic and smooth pursuit disorders, vergence abnormalities, nystagmus, and ocular oscillations [
1,
5]. Gaze palsy refers to weakness of the conjugate movement of the eyes in a particular direction [
5]. When we found patient with vertical gaze palsy and intact vestibulo-ocular reflex, differential diagnosis involving supranuclear lesion must be come to our mind. The aim of this case report is to demonstrate a rare case of vertical gaze palsy and investigate the location and etiology of the lesion.
Case Report
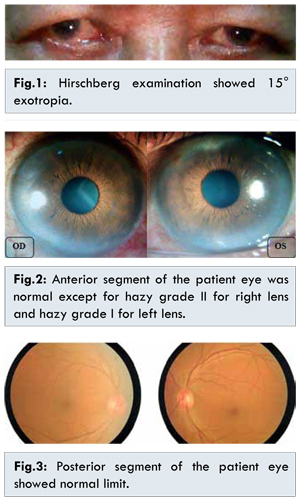
A 62 years old male came with chief complaint of sudden onset inability to move his eyes vertically. One month back, suddenly the patient felt severe headache (Visual Analog Score 8) while working. He went to general practitioner nearby and was diagnosed as hypertensive. A couple hours later, the patient began to feel that he couldn’t move his eyes up and down position even voluntarily, but had no double vision. The family noticed squint in right eye to outside. Patient had blurred vision especially on his right eye since a year, he described it as smoke covering his right eye. He had history of hypertension and dyslipidemia known since 3 months earlier but was not on regular medication. He has been smoking since teenager and had one cigaratte pack on average every day. He had no hemiparesis, hemiplegia or syncope. From ophthalmological status, the visual acuity of his right eye was 6/20 which became 6/12f2 after S +1.50 D correction and for left eye 6/20 became 6/6f2 after S+1.50 D, C-0.75 D x 120° correction. The position of his eye was 15° exotropia [Fig.1], with positive cover test, uncover test, and alternate cover test. Prism cover test result was 25?D base-in. Intraocular pressure of his right eye was 13 mmHg and left eye 17 mmHg. Anterior segment of the eye was within normal limit except the lens was hazy grade 2 for right eye and grade 1 for left eye [Fig.2]. Patient had normal pupillary response and no relative afferent pupillary defect. The posterior segment was within normal limit in both eyes [Fig.3].
On eye movement test, the patient had no difficulty in moving his eye to the left and right gaze but there were bilateral similar movement restriction at upper gaze and no movement at all at down gaze [Fig.4]. Patient also couldn’t move his eyes on convergence test but he had an intact vestibulo-ocular reflex. The MRI test revealed that there were acute infarct at left thalamus and left-right basal ganglia, without any midbrain involvement [Fig.5]. The patient was prescribed aspirin, simvastatin, amlodipine, and valsartan. After 6 months of starting systemic medication, no improvement was noted [Fig.6]. We suggested the patient to have a regular follow up at another 3 months to evaluate if there was any improvement of the eye movement and to consume the systemic medication regularly. We also explained the possibility of bad prognosis regarding patient’s vertical gaze palsy.
Discussion
A prominent clinical finding in our patient was an acute isolated vertical gaze palsy. The patient had bilateral symmetric gaze palsy and intact vestibulo-ocular reflex so the lesion causing the gaze palsy is supranuclear. Lesion at nuclear oculomotorius can be excluded because there were no sign of ptosis, dilated pupil on light reflex test and palsy at adduction in this patient. An acute onset vertical gaze palsy is most often due to midbrain infarction. If in isolation, the infarct is typically due to microvascular ischaemia in the territory of the thalamic-subthalamic paramedian artery, which originates from the posterior cerebral artery [
6]. However, in our case there were no other clinical evidence of midbrain ischemia such as a third nerve palsy, and MRI did not reveal evidence of ischemia of the midbrain, the midbrain/thalamic junction, pons nor the cerebral hemisphere like common cases found [
5]. Instead there were infarcts at left thalamus and left-right basal ganglia, as shown at Fig.5.
Reasons for this might include the fact that the lesion was too small to be detected by the thickness of our MRI slices. Another postulation is that the thalamic lesion may have produced the vertical gaze palsy by interrupting supranuclear inputs. There were also another study that found vertical gaze palsy with thalamic infarct without midbrain involvement [
7-
10]. They suggested that the vertical gaze palsy was secondary due to interruption of supranuclear fibers as they cross the medial thalamus en route to the pretectal and prerubral areas. Vertical gaze palsy could be an initial manifestation in many etiologies involving supranuclear lesion. In the acute setting, brainstem ischemia, hemorrhage, and demyelination are the most common causes. In the chronic setting, neurodegenerative and metabolic disease are most common. A few etiologies are vascular lesion, Parinaud syndrome, Parkinson disease, Whipple disease, progressive supranuclear palsy (PSP) [
1]. Parinaud syndrome can be excluded because our patient did not have any sign besides vertical gaze palsy. There was no lid retraction (Collier sign), downward gaze preference (setting-sun sign), convergence-retraction nystagmus, nor the dilated pupils [
11]. Parkinson’s disease also can be excluded because our patient did not have any disturbance in saccadic movement. Blink and pupillary reflex were also good in our patient. Whipple disease can be excluded because the patient had no systemic complaint also the oculomasticatory myorrhythmia that is hallmark for diagnosing this condition is not found in our case [
4]. In order to exclude PSP, we should have a long term follow up.
There is no treatment of vertical gaze palsy itself, so the disease or condition causing the gaze palsy must be treated [
2]. In our case, the underlying disease of the vertical gaze palsy is infarct at left thalamus and left-right basal ganglia due to vascular lesion. The risk factor known from this patient is hypertension grade II, dyslipidemia and smoking. The patient was prescribed systemic medications and also suggested to stop smoking. The prognosis of a lesion in the visual neural pathways that cause conjugate gaze palsy varies greatly. Depending on the nature of the lesion, recovery may happen rapidly or may never progress. There has been a previous case reported of transient vertical gaze palsy with resolution of symptoms within three hours, highlighting the role of the thalamus in vertical gaze [
12]. In one case report, improvement of vertical gaze palsy was seen 4 days after onset of stroke. The writer postulated that the hyperacute stage of midbrain infarction was the cause of the palsy [
13]. Another case report found that vertical gaze palsy almost disappeared one month after sudden-onset of double vision and unilateral infarct in the thalamo-mesencephalic junction [
14]. Contrary from the case report above, our patient showed no improvement of vertical gaze palsy up to 6 months after the onset. The primary cause of vertical gaze palsy in our patient was infarct lesion but the neurodegenerative process such as PSP still cannot be ruled out which may explain why this patient did not show any improvement until 6 months after onset.
Conclusion
Patient with vertical gaze palsy needs thorough clinical neuro-ophthalmological examination together with neuroimaging to establish the etiology and investigate the location of the lesion. In this case, MRI revealed infarct on thalamic-basal ganglia which was considered to contribute in vertical gaze palsy by interrupting supranuclear inputs.
References
- Daroff RB, Troost BT, Leigh RJ. Supranuclear disorders of eye movements. In: Glaser JS (ed). Neuro-ophthalmology. Lippincott Williams & Wilkins: Philadelphia; 1990. pp.299-324.
-
Kandel ER, Schwartz JH, Jessel TM. In: Principles of Neural Sciences. 4th ed. McGraw-Hill Co: New York; 2000. pp.234-239.
-
Karatas M. Internuclear and supranuclear disorders of eye movements: clinical features and causes. European Journal of Neurology. 2009;16:1265-1277.
-
Walsh FB, Hoyt WF, Miller NR. In: Clinical Neuro-ophthalmology: The Essentials. 2nd ed. Lippincott Williams & Wilkins: Philadelphia; 2008. pp.358-366.
-
Kommerell G. Supranuclear disorders of ocular motility. In: Schiefer U, Wilhelm H, Hart WM (eds). Clinical Neuroophthalmology - A Practical Guide. Springer: Berlin; 2009. pp.155-170.
-
Janet Crucker. Neural control and clinical disorders of supranuclear eye movements. ACNR Journal. 2012;12(3):12-14.
-
Guberman A, Stuss D. The syndrome of bilateral paramedian thalamic infarction. Neurology. 1983;33:540-546.
-
Gentilini M, DeRenzi E, Crisi G. Bilateral paramedian thalamic artery infarcts: report of eight cases. J Neurol Neurosurg Psychiatry. 1987;50:900-999.
-
Clark JM. Vertical gaze palsies from medial thalamic infarctions without midbrain involvement. Stroke. 1995;26:1467-1470.
-
Khan M, Sidiropoulos C, Mitsias P. Unilateral thalamic infarction presenting as vertical gaze palsy: a case report. Journal of Medical Case Reports. 2011;5:535.
-
Karatas M, Karakurum B, Tuncer I. A case of Parinaud syndrome due to the remote effect of small cell carcinoma. Int J Neurosci. 2009;114:291-297.
-
Blitshteyn S, Hentschel K, Czervionke LF, Eidelman BH. Transient vertical diplopia and nystagmus associated with acute thalamic infarction. Clin Imaging. 2009;30:54-56.
-
Takamatsu K, Takizawa T, Sato S, Yoshihisa KT, Miyamoto T. A case of transient vertical gaze palsy following right thalamic and midbrain infarction. Brain and Nerve. 1993;45(11):1055-1059.
-
Ijima M, Hirata A, Tadano Y, Kamakura K, Nagata M. A case of vertical gaze palsy associated with a unilateral infarct in the thalamo-mesencephalic junction on MR imaging. Clinical Neurology. 1994;34(4):356-360.