Introduction
Angiomyxoma is a rare infiltrative mesenchymal tumor of the pelvic region. It is more common in females than males with a 6:1 ratio. It was first described in 1983 by Steeper and Rosai [1] and there have been about 200 reported cases of aggressive angiomyxoma to date. This aggressive, rare and slowly growing tumor is usually an incidental finding in the perineal or pelvic region. Patients usually present with a dull aching pain, mass, or urinary symptoms like dysuria, urinary retention and possible dyspareunia. Treatment choices range from surgical resection to gonadotropin-releasing hormone (GnRH) inhibitors for recurrent tumors that are positive for estrogen and progesterone receptors. Selective estrogen receptor modulators (SERM) have also shown to be of some proven benefit. Considering the rare occurrence of this tumor it is considered important to closely observe the presentation and prognosis for better understanding of its progression. Understanding its natural course and occurrence pattern will help develop guidelines to guide physicians in its proper diagnosis and management.
Case Report
41 year old G1P1 was seen for her annual gynecological examination and was found to have a left sided vulvar mass. Upon further questioning patient reported it to be there for the past 2 years without any significant symptoms and very slow growth in its size. Patient denied any pain, skin changes, bleeding or discharge from the area. She reported to having monthly heavy menstrual periods, with passage of medium to large clots for the past one year with worsening symptoms in the last 6 months. These periods lasted for 5-7 days with changing pads/tampons every 2-3 hours for the first few days of her cycle. Upon review of the data her most recent Pap smear and HPV test were negative, recent mammogram was also found to be Breast Imaging Reporting and Data System (BIRADS) 1. Patient denied family history of any malignancy. She did have a personal history of melanoma of the back which was excised a few years ago with no recurrence. Patient’s past surgical history consisted of a tubal ligation and social history positive for daily smoking for the past 20 years.
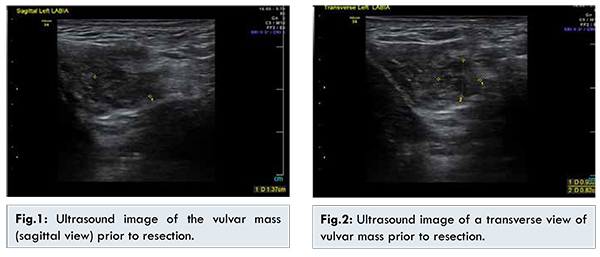
Based on initial examination findings, possible Bartholin gland cyst was suspected and conservative management was discussed along with a perineal ultrasound for better understanding of the mass. The perineal ultrasound showed a complex 1.4 cm nodule in the left labia which had nonspecific features, heterogeneous echotexture that contained mostly solid elements with several cystic areas [Fig.1,2]. Based on the ultrasound findings discussion was done with the patient regarding her management options and decision was made to proceed with surgical excision of the mass. The intra-operative findings revealed glistening surfaced mass with some fatty tissue deposits. The postoperative course was unremarkable and the final pathology report of the mass showed it to be aggressive angiomyxoma with positive margins.
Based on the pathology results, gynecologic oncologist consult was requested and MRI of the pelvis and abdomen was done. The MRI showed a uterus measuring 10.9x6.3x5.6 cm with a uterine stripe measuring 11 mm. There were multiple uterine masses possible leiomyomas, one of them measuring 2.7x2.8 cm and one exophytic in nature at the uterine fundus, another one was noticed in the posterior body of the uterus with submucosal extension into the endometrial canal measuring 2.5x3 cm, and lastly another at the posterior body of uterus measuring 2.1x1.8 cm. There was also 1.2x1.4x1.7 cm posterior vaginal wall cyst at the level of the external cervical os. Based on the MRI findings, pelvic ultrasound was requested and showed three uterine masses consistent with possible leiomyomas, measuring 3.3, 3.0 and 2.4 cm.
The ultrasound showed a stripe of 9.3 mm and uterus measuring 5.8x6x8.7 cm with a 1.7 cm cystic mass in the superior aspect of vagina. Further discussion was done with the patient regarding her management options and she decided to proceed with hysterectomy with preservation of her ovaries and also removal of the vaginal wall cyst. Prior to the scheduled surgery patient underwent an in office endometrial biopsy (EMB), that showed menstrual endometrium, negative for malignancy and hyperplasia.
Various hysterectomy routes were discussed with total versus partial hysterectomy and decision was made to proceed with robotic assisted total laparoscopic hysterectomy-bilateral salpingectomy (TLH BS) and vaginal cyst removal. Patient underwent the proposed procedure approximately two months after the initial diagnosis of angiomyxoma. She tolerated the procedure without any complications and postoperative recovery was unremarkable. Pathology results of the uterus and cervix showed a benign endometrial polyp, proliferative endometrium, leiomyomas that were subserosal and intramural, and benign cervix with immature squamous metaplasia. All specimens were negative for malignancy. The vaginal cyst which was removed vaginally with 2 layer closure was also proved to be benign in nature and not related to angiomyxoma.
Discussion
Aggressive angiomyxoma was initially presented in nine separate cases, all with similar microscopic appearance. This consisted of spindle or stellate cells that were separated by loose myxoid stroma that was rich in collagen fibrils; also with a vascular component. The spindle cells were consistent with myofibroblastic differentiation under ultrastructural study. The differential diagnosis for this unusual tumor ranged from myxoma, myxoid liposarcoma, sarcoma botryoides, and other soft tissue tumors with myxoid changes. It was termed aggressive angiomyxoma due to the neoplastic nature of the blood vessels and the highly infiltrative and recurrent nature of the presenting tumor [1].
Most individuals usually present with nonspecific symptoms which lead to misdiagnosis of Bartholin gland cyst, lipoma or hernia. It has a mass-like feeling that is gelatinous in texture. It usually arises in the vulvovaginal area, perineum or pelvis. It can be positive for estrogen and progesterone receptors and it has been noted that there may be a chromosomal translocation at 12q13-15 band involving the High Mobility Group AT-Hook 2 (HMGA2) gene. Due to the tumor cells being positive for estrogen and progesterone receptors, some cases have been reported being responsive
to Gonadotropin-releasing hormone (GnRH) agonist [2].
Many cases have been reported where GnRH agonist have been successful in preventing the recurrence. In 1998, Nyam and Pemberton examined treatment of radiotherapy prior to surgical resection and intraoperative radiation but the prognosis of the patient was difficult to assess due to failure to follow up [3]. Another case presented by Htwe suggested that there is a hormonal component present in the tumor which was noticed due to the increasing size of tumor in a pregnant female [4]. In 1996, it was taken a step further by reporting that the tumor had estrogen and progesterone receptors and it was the first case to use a GnRH agonist for treatment that was shown to be successful in preventing recurrence [5].
Since the introduction of GnRH agonists as a treatment for aggressive angiomyxoma there have been many reports of other successful cases. An example of GnRH therapy is shown in this case involving a 34 year old woman who had an excision of an aggressive angiomyxoma of perineum was treated with Leuprolide for 12 months. Three months after completion of GnRH agonist treatment the tumor recurred, patient was restarted on GnRH agonist and complete resolution was shown after further three months of treatment. The bothersome side effects are the obstacle in long term treatment with GnRH agonist such as osteoporosis, depression, and menopausal symptoms. It would be worthy to explore if intermittent therapy with GnRH agonist be a choice of treatment after surgical resection [6].
Conclusion
By examining this case in collaboration with other case reports about aggressive angiomyxoma, many physicians can gain a better understanding of incorporating aggressive angiomyxoma into their differential diagnosis and on how to diagnose and treat it with a proper guideline. Many patients are unaware of the vulvar mass until it is found on a routine gynecological examination. It is important to keep aggressive angiomyxoma as part of the differential diagnosis when patient’s present with painless vulva mass. The current literature supports the current recommendations for treatment of aggressive angiomyxoma with a surgical resection and GnRH agonist treatment following resection. The duration of GnRH agonist treatment is unknown at the moment, whether or not a short course or intermittent treatments are necessary. There are no guidelines available currently for follow up imaging post-surgical resection in order to surveillance a patient for reoccurrence. For our case the patient declined GnRH agonist treatment at this time but would return in 6 months for a follow up pelvic MRI or ultrasound. It is important to closely follow the patient with imaging of MRI or ultrasound since aggressive angiomyxoma has a high reoccurrence rate.
Acknowledgement
WBGH medical records and radiology department; Dr. Qi Shi at The Wright Center for Graduate Medical Education for her help and support.
References
- Steeper T, Rosai J. Aggressive angiomyxoma of the female pelvis and perineum: report of nine cases of a distinctive type of gynecologic soft-tissue neoplasm. Am J Surg Pathol. 1983;7(5):463-475.
- Sutton B, Laudadio J. Aggressive angiomyxoma. Archives of Pathology & Laboratory Medicine. 2012;136(2):217-221.
- Nyam D, Pemberton J. Large aggressive angiomyxoma of the perineum and pelvis: an alternative approach. Report of a case. Diseases of the Colon and Rectum. 1998;41(4):514-516.
- Htwe M, Deppisch L, Saint-Julien J. Hormone-dependent, aggressive angiomyxoma of the vulva. Obstetrics And Gynecology. 1995;86(4 Pt 2):697-699.
- Fine B, Munoz A, Litz C, Gershenson D. Primary medical management of recurrent aggressive angiomyxoma of the vulva with a gonadotropin-releasing hormone agonist. Gynecologic Oncology. 2001;81(1):120-122.
- Shinohara N, Nonomura K, Ishikawa S, Seki H, Koyanagi T. Medical management of recurrent aggressive angiomyxoma with gonadotropin-releasing hormone agonist. International Journal Of Urology: Official Journal Of The Japanese Urological Association. 2004;11(6):432-435.