Introduction
Coronary artery anomalies and hypertrophic cardiomyopathy are a rare group of cardiac disorders associated with sudden death [
1]. Anomalous right coronary from opposite sinus (ARCOS) are mostly benign, but the inter-arterial type, a high risk anatomical variant, has been termed malignant because of its potential to cause myocardial ischemia and sudden cardiac arrest [
2].
Our review of literature revealed high association of sudden cardiac arrest with these disorders. Hence, we present a case of a patient with fracture distal end of radius with preoperative diagnosis of malignant ARCOS and hypertrophic cardiomyopathy with its subsequent management.
Case Report
A 38 year old, 70 kg male presented to our hospital’s orthopaedic emergency with fracture left distal end of radius. During preanaesthetic assessment patient gave history of occasional palpitations with a single episode of syncopal attack three months back for which he had not sought any treatment. Metabolic equivalents were greater than 4. Clinical examination revealed pulse rate of 88/min, regular with normal volume and blood pressure of 170/100 mm Hg in supine position. Electrocardiography showed T wave inversion in all the leads. Cardiologist consultation was sought who advised 2D echocardiography which revealed non-obstructive hypertrophic cardiomyopathy with ejection fraction of 75%. Hence, patient was started on tablet metoprolol 50 mg once daily orally. Patient’s blood pressure was controlled on ß-blocker and he was posted for closed reduction under fluoroscopic guidance with informed high risk consent. Tablet alprazolam 0.25 mg was administered as anxiolytic on night before procedure.
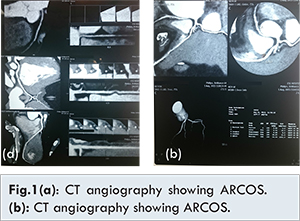
Patient was wheeled in the operation theatre and all standard ASA monitors were attached. ECG showed significant ST segment depression (-2.8mV) in lead II, III and aVF with blood pressure of 146/84 mm Hg and pulse rate of 68/min. Patient was again referred to cardiologist who advised cardiac enzymes, CT angiography and Holter monitoring. Cardiac enzymes were within normal limits. CT angiography revealed anomalous right coronary artery arising from left coronary cusp with abnormal course between aorta and pulmonary trunk with diffusely reduced caliber [Fig.1(a) and 1(b)]. Holter monitoring done under ß- blocker therapy revealed frequent atrial premature contractions and significant monomorphic ventricular ectopics with occasional couplets and bigeminy, more often at night. Tablet metoprolol dose was increased to 75 mg OD. Thus, diagnosis of malignant ARCOS associated with hypertrophic non-obstructive cardiomyopathy was made with high risk of perioperative major cardiac event.
The perioperative team of anaesthesiologist, cardiologist and orthopaedician counseled the patient about the high risk of perioperative sudden cardiac arrest and discussed the treatment options of both the conditions considering the risk benefit ratio. A consensus was reached for closed reduction of the fracture followed by referral to a cardiothoracic center for definitive management of malignant ARCOS. On the day of procedure patient was taken into operation theatre with cardiology backup. Standard ASA monitors were attached. Patient had a baseline blood pressure: 148/88 mm Hg, pulse rate: 64/min and SpO2: 100%. An 18G intravenous line was secured and ringer lactate was started. A venturi mask provided FiO2 of 0.4. Injection midazolam 1 mg intravenously was administered. Ultrasound guided [Sonosite M-Turbo® ultrasound] supraclavicular brachial plexus block was given with 15 ml of 0.75% ropivacaine, 10 ml of 0.5% levobupivacine. Orthopaedician performed closed reduction under C-arm guidance. The whole procedure took 30 minutes and the peri-procedural course was uneventful.
Check X-ray of the patient confirmed acceptable reduction of fracture. Patient was referred to a cardiothoracic center on ß blocker therapy for further management but the patient opted for medical management for ARCOS. Patient was discharged with instructions to refrain from any strenuous work and not to participate in competitive athletics. Follow up after 6 weeks revealed fracture union and patient well controlled on ß blocker therapy.
Discussion
Hypertrophic cardiomyopathy and coronary artery anomalies are the most common cause of sudden death in young athletes [
1]. ARCOS arising from left sinus with an incidence of 0.92% [
2] can anatomically traverse its course as inter-arterial, retro-aortic, or anterior to the pulmonary trunk [
3]. They are mostly benign, except the inter-arterial type which with a variable incidence between 0.026% and 0.250% is classified as malignant due to its association with sudden death [
4].
Myocardial ischemia in the inter-arterial variant can occur due to coronary spasm, intramural course of ARCOS within the aortic wall [
2] or compression of the proximal segment due to aortic and pulmonary dilatation with increased cardiac output [
5]. Narrow ostium of the aberrant artery with slit like orifice and acute angle take off is also known to compromise blood flow [
6]. Hypertrophic non-obstructive cardiomyopathy may be associated with latent left ventricular outflow obstruction, aggravated under physiological or pharmacological stress with reduction in left ventricle end diastolic volume or increase in left ventricle contractility [
7].
Most registries have diagnosed these disorders retrospectively [
1] either after a major cardiac event or on autopsy. Perioperative myocardial ischemia has been reported in patients taken up for surgery [
8]. Preoperative risk stratification of a patient with cardiac disease is aimed at identifying the risk benefit ratio of surgery versus cardiac disease and any changes in perioperative management, if required. In our case, diligent pre-anaesthethic workup and team based approach helped in timely and accurate diagnosis of these concurrent conditions.
ACC/AHA guidelines advocate surgical correction of malignant ARCOS [
9]. ß blocker therapy is the main stay of medical management for both these cardiac disorders [
10,
11]. Current AHA/ACC guidelines for a patient of cardiac disease remain silent on the perioperative management of patients with these disorders coming for non-cardiac surgery [
12]. In our case, peripheral nerve blockade under ultrasound guidance proved to be a boon. Dynamic visualization of the anatomy helped in providing good quality anaesthesia and analgesia with lesser dose of local anaesthestic. This leads to better haemodynamic stability and minimal risk of side effects.
Conclusion
Diligent pre-anaesthetic assessment with teamwork is vital in diagnosis and management of rare high risk medical conditions. The knowledge and skill of ultrasound guided nerve blocks is a boon in patients with significant co-morbidities.
References
- Williams RA. The historical background of sudden death in athletes. In: Williams RA, The Athlete and Heart Disease: Diagnosis, Evaluation & Management. Philadelphia: Lippincott Williams & Wilkins; 2000:1-8.
- Angelini P, Velasco JA, Flamm S. Coronary anomalies: incidence, pathophysiology, and clinical relevance . Circulation. 2002;105:2449-2454.
- Kim SY, Seo JB, Do KH, Heo JN, Lee JS, Song JW, et al. Coronary anomalies: classification and ECG-gated multi-detector row CT findings with angiographic correlation. Radiographics. 2006;26(2):317-334.
- Greet B, Quinones A, Srichai M, Bangalore S, Roswell RO. Anomalous right coronary artery and sudden cardiac death. Circulation: Arrhythmia and Electrophysiology. 2012;5: e111-e112.
- Kaku B, Kanaya H, Ikeda M, Uno Y, Fujita S, Kato F, et al. Acute inferior myocardial infarction and coronary spasm in a patient with an anomalous origin of the right coronary artery from the left sinus of Valsalva. Jpn Circ J. 2000;64:641-643.
- Taylor AJ, Rogan KM, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol. 1992;20:640-647.
- Shah JS, Esteban MT, Thaman R, Sharma R, Mist B, Pantazis A, et al. Prevalence of exercise-induced left ventricular outflow tract obstruction in symptomatic patients with non-obstructive hypertrophic cardiomyopathy. Heart. 2008;94:1288e94.
- Daher M, Zanatta AR, Henz BD, Silva MC, Santos SN, Leite LR. Sudden cardiac arrest in general anesthesia as the firstmanifestation of anomalous origin of the left coronary artery. Rev Bras Anestesiol. 2012;62:878-884.
- Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation. 2008;118:2395-2451.
- Kaku B, Shimizu M, Yoshio H, Ino H, Mizuno S, Kanaya H, et al. Clinical features of prognosis of Japanese patients with anomalous origin of the coronary artery. Jpn Circ J. 1996;60(10):731-741.
- Maron BJ. Hypertrophic cardiomyopathy: a systematic review. JAMA. 2002;287:1308- 1320.
- Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing non cardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64.