Introduction
Renal papillary necrosis (RPN) is the coagulative necrosis of the renal medullary pyramids and papillae brought on by a host of associated conditions and toxins that exhibit synergism towards the development of ischemia. The clinical course of RPN varies depending on the degree of vascular impairment, associated casual factors, health of the patient, unilateral or bilateral involvement and specifically the number of affected papillae. RPN is potentially disastrous and in the presence of bilateral involvement or an obstructed solitary kidney, may lead to renal failure. The infectious sequel of RPN is more serious if the patient has multiple medical problems, particularly diabetes mellitus.
Materials & Methods
A retrospective study of autopsy cases of adults was done over a period of 3 years and we archived 4 cases from the total of 650 autopsies which showed bilateral renal papillary necrosis at autopsy.
Results
Table 1 gives brief history of these 4 cases with clinical presentation, cause of death, gross and microscopic features of kidneys. There were 3 males and 1 female, age ranging between 40 to 55 years and in one case, the patient was a 15 year old boy.
Discussion
In 1877, Friedrich [
1] first described renal papillary necrosis in a patient with urinary obstruction resulting from hypertrophy of the prostate, since then, researchers have reported the patients with renal papillary necrosis have diabetes, severe urinary tract obstruction as well as with analgesics and drug abuse nephropathy. Researchers report that 17%-90% of all patients with renal papillary necrosis have diabetes and 25%-73% of patients have severe urinary tract obstruction [
2].
RPN is classified as one end of a spectrum of changes associated with pyelonephritis and tubulointerstitial nephritis. RPN is often considered as a complication or extension of severe pyelonephritis that is more devastating than usual because of associated disease states particularly diabetes and urinary tract obstructions. Infection is a frequent and important finding in the most of the cases, contributing significantly to the clinical presentation of RPN. (i.e fever and chills in approximately two third of patients). However, RPN can occur in the absence of infection which indicates that infection may not be the primary process in the pathogenesis. Conversely, infection likely is a complication of RPN, the necrotic papillae acts as nidus for infection and lithogenesis [
3]. Infection within necrotic material and calculi is often definitively treated with antibiotics alone, and infection often recurs as RPN progresses to chronic pyelonephritis.
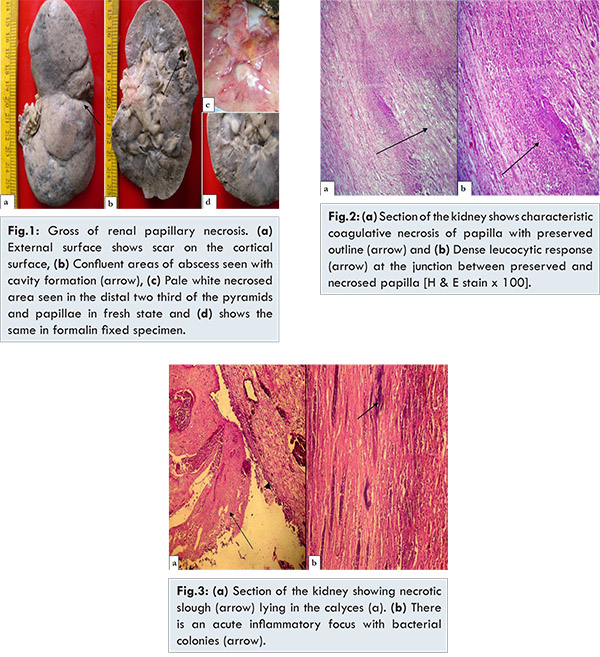
In our four cases, the pathologic findings on a cut section of kidney grossly showed white to yellow necrosis on the tips in the distal two third of the pyramids [Fig.1]. Microscopically, the kidneys showed features of acute pyelonephritis with cortical abscesses and the sections from the papillae, the tissue showed characteristic coagulative infarction and necrosis, with preserved tubule outline [Fig.2]. The leucocytic response is limited to the junction between preserved and destroyed tissue. In septicaemia cases, there could be bacterial colonies in the background of acute inflammatory exudates [Fig.3]. After the acute phase, scars that can be observed on the cortical surface as a fibrous depression replace the inflammatory foci. This pyelonephritic scar is usually associated with inflammation, fibrosis and deformation of underlying calyces and pelvis which was seen in our case of 55 year old male who had underlying diabetes [Fig.1a].
RPN is considered a sequel of ischemia occurring in renal papillae and in the medulla. A host of insults generates this ischemia, one of which may be infection. The boggy inflammatory interstitium of the pyelonephritic kidney compress the medullary vasculature and, thus predisposes the patient to ischemia and RPN. This vasculature can become compressed, attenuated or impaired from several other associated diseases, most notably diabetes mellitus, urinary obstruction and analgesic nephropathy [
4]. Therefore RPN is a distinct clinical and pathophysiological entity primarily caused by ischemia that can develop without pyelonephritis or urinary tract infection and is likely a focus of infectious complications. RPN primarily is a bilateral process, as is expected when considering the systemic nature of the associated disease and the ischemic pathophysiologic mechanism of RPN. True unilateral RPN occurs when the predisposing factor is infection or obstruction that is limited to one kidney [
4]. RPN generally affects elder patients with mean age of 53 years. Nearly 90% cases occur in the individuals older than 40 years [
3]. RPN is uncommon in younger population and in paediatric group, except in patients with sickle cell hemoglobinopathy [
5], hypoxia, dehydration and septicemia and substance abuse [
6]. We have encountered renal papillary necrosis in a very young boy of 15 year old who had sickle cell anaemia and expired due to sickle cell crisis and acute renal failure.
Mandel [
2] organised the first comprehensive review to focus attention on RPN. In his series, which examined 160 cases of RPN from the world wide literature, 96 (60%) patients had diabetes mellitus, 48 (30%) patients had urinary tract obstruction and 15 (9.4%) patients had both. In 1945, Spuhler and Zollinger [
7] documented the first description of analgesic nephropathy. Since then, analgesic abuse has been increasingly significant in the development of papillary necrosis. In one of the four cases, there was a 45 year old female was on analgesics since last 15 years for rheumatoid arthritis in whom there was a bilateral papillary necrosis and presented as acute renal failure which was fatal.
Analgesic nephropathy is more common in females than in males. It is the one of the most common and preventable factor. A classic factor (drug) is phenacetin, with its highly toxic metabolite, P-Phenetidin [
8]. Recently, however, the rising popularity of non-steroidal anti- inflammatory drugs (NSAIDS), particularly, those that inhibit cyclo-oxygenase (COX-1, COX-2) pathway, has led to a relatively high frequency of adverse events in patients at risk for RPN [
8]. Thus most of the patients with RPN have a multifactorial origin and physician must consider the pathogenesis of RPN, a combination of detrimental factors that overlap and operate to cause RPN.
RPN has variable clinical course that ranges from a chronic, protracted and relapsing form to an acute, rapidly progressive form. The acute progressive is particularly rare, but the effects are devastating, resulting in death from septicaemia and renal failure. Patients with more common chronic form may remain asymptomatic until diagnosed incidentally through the appearance of ring shadow on a radiographic image [
9], by the passage of sloughed papillae in the urine or during autopsy as noted in our cases.
The symptomatic form manifests as an episode of pyelonephritis and hydronephrosis and it mimics nephrolithiasis. The most common presenting symptoms of symptomatic patients are fever and chills, flank and/or abdominal pain and hematuria. Acute renal failure and oliguria or anuria occurs, but when it does, the disease may be fulminant, requiring dialysis and potentially resulting in death.
Conclusion
If the renal functions deteriorate suddenly in the patient with confirmed diabetes or a patient with a known history of chronic obstructive uropathy and/or pyelonephritis, consider the diagnosis of papillary necrosis.
References
- Friedrich N. Ueber necrose der nierenpapillen bei hydronephrose. Virchows Arch A Path Anat. 1877;69:308-312.
- Mandel EE. Renal medullary necrosis. Am J Med. 1952;13:322-327.
- Vijayaraghavan SB, Kandasamy SV, Mylsamy A, Prabhakar M. Sonographic features of necrosed renal papillae causing hydronephrosis. J Ultrasound Med. 2003;22:951-956.
- Abe K, OzonoY, Miyazaki M, Furusu A, Shioshita K, Sasaki O, et al. Prostaglandin E1for renal papillary necrosis in a patient with diabetes mellitus. J Int Med Res. 1999;27(2):90-95.
- Zadeii G, Lohr JW. Renal papillary necrosis in a patient with sickle cell trait. J Am Soc Nephrol. 1997;8(6):1034-1039.
- Strang J. Substance Abuse: The size of the Problem. Medicine. 1995;23:41-45.
- Spuhler O, Zollinger HU. Chronic interstitial nephritis. Z Klin Med.1953;151(1):1-50.
- Bing RJ. Cyclooxygenase-2 inhibitors: Is there an association with coronary or renal events? Curr Atheroscler Rep. 2003;5(2):114-117.
- Voulgarelis M, Ziakas PD. Images in clinical medicine. Renal papillary necrosis unmasking sickle cell disease. N Engl J Med. 2005;352(12):1237-1251.