Introduction
Hemophagocytic syndrome (HPS), also termed as hemophagocytic lymphohistiocytosis (HLH) [
1], is an uncommon life-threatening clinical syndrome characterized by fever, pancytopenia, splenomegaly and hemophagocytosis, in which the activated macrophages engulf erythrocytes, leukocytes, platelets and their precursor cells in bone marrow, liver, or lymph nodes [
1,
2]. HPS is associated with collagen vascular diseases, malignancies and viral, bacterial, fungal and parasitic infections [
3-
6]. We report a case of Epstein-Barr virus induced hemophagocytic syndrome.
Case Report
A 19 year old boy presented with dry cough and loss of appetite for 2 weeks and high grade intermittent fever for one week duration. He has been treated as dengue fever one month ago. But the dengue NS1 antigen has been negative and on discharge he has had a bicytopenia of WBC 2.3x109/L and platelet 52x109/L with hemoglobin 12.5 g/dL. On examination he was ill, febrile (38.50C) and pale. There was no icterus, lymphadenopathy or skin rash. Pulse rate was 104 beats/ min, blood pressure 96/70 mmHg. Lungs were clear. Liver was palpable 3 cm below the right costal margin.
Laboratory studies showed the following values: WBC 1.7x109/L, platelet 31x109/L, hemoglobin 9.6 g/dL. Peripheral blood film showed leucopenia with reactive lymphocytosis without any atypical lymphocytes, normocytic normochromic red cells and moderate thrombocytopenia. Reticulocyte count was 1.4%. Liver function tests showed AST 48 U/L, ALT 24 U/L, serum albumin 3.6 g/dL. INR was 1.01. APTT was 34.3 seconds. Blood urea, serum electrolytes, serum creatinine, chest X-ray, ECG and urine full report was normal. CRP was 59 mg/dL (<5 mg/dL), ESR was 55 mm in first hour. Blood and urine cultures were negative. 2D echocardiogram was normal.
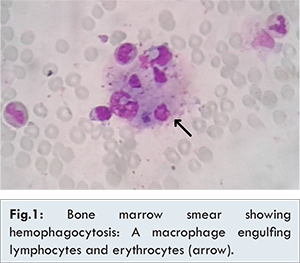
Ultrasound scan of abdomen revealed mild hepatosplenomegaly. Bone marrow aspiration showed atypical lymphoid infiltrate and histiocytes with increased activity showing prominent hemophagocytosis [Fig.1]. Mantoux test was negative. Serologies for dengue, hepatitis B, C and HIV were negative. Antinuclear antibody was negative. Antibody to Epstein-Barr virus (EBV) specific viral capsidic antigen was positive. There were elevated levels of triglycerides: 408.5 mg/dL (10-200), serum ferritin: 786 ng/mL (28-397) and normal plasma fibrinogen: 175 mg/dL (150-350).
The diagnosis of EBV associated hemophagocytic syndrome was made. Criteria in favour were fever (>38.50C), splenomegaly, cytopenias, elevated triglycerides, hemophagocytosis in bone marrow, serum ferritin >500 ng/mL and positive EBV serology. With hematology opinion he was given a course of oral dexamethasone for total 8 weeks (10 mg daily, 5 mg daily, 2.5 mg daily, 1.25 mg daily each for two weeks) and etoposide (150 mg/m2, 5 doses in every third day in first two weeks then 150 mg/m2 weekly for 5 weeks). However he was not started on antiviral drugs. Following treatments, he made clinical improvement and laboratory parameters were normalized.
Discussion
Hemophagocytic syndrome is an uncommon disease; high index of suspicion is required for diagnosis. Histiocyte society has revised the diagnostic guidelines to be used for diagnosis of HLH [Table 1] [
7]. This syndrome is categorized into primary or genetic HPS and secondary or reactive HPS, which is the disease entity associated with infections, malignancies and autoimmune diseases [
2,
8]. Viral agents triggering HPS include Epstein-Barr virus (EBV) which is the commonest, cytomegalovirus, herpes simplex virus, varicella zoster virus, human herpes virus 6 & 8, HIV, influenza virus, parvo virus, hepatitis virus and entero virus [
8].
In EBV induced HPS, there is a deficiency in producing EBV specific cytotoxic T cells due to infected primary CD8+ cells, suggesting an impaired or absent function of NK cells and cytotoxic T cells [
9]. These cytotoxic T cells are needed to regulate EBV infected B cells. Due to poor regulation of B cells there is persistence of EBV infection. As a result, there is a sustained immune response with persistently high pro-inflammatory cytokines levels (such as interferon ?, tumour necrosis factor a, interleukin 6, 8, 10, 16, 18, and macrophage colony stimulating factor) leading to hemophagocytosis and multi organ failure [2,8].
The Histiocyte society (HS) has proposed and revised the treatment protocol for HLH in 2004 (HS-2004) and with this protocol there is significant improvement in overall survival [
7]. According to HS therapeutic guidelines the mainstay of treatment is based on corticosteroids and immunoglobulin infusions in patients with less severe disease and etoposide, dexamethasone and cyclosporine in more severe disease. Etoposide inhibits EBV nuclear antigen in EBV-infected cells showing an important role in the management of EBV induced HLH [
8]. Antiviral agents like acyclovir do not appear to be useful in the treatment of EBV-associated HPS [
1,
8]. Even though EBV induced HPS has poor prognosis if untreated, mortality due to hemorrhage and fatal infections [
1,
10], early recognition and appropriate aggressive therapy has yielded good long term out come with reduced morbidity and mortality.
Conclusion
HPS is an uncommon fatal clinical syndrome associated with genetic, collagen vascular, neoplastic disorders and wide variety of infections, particularly EBV infection. Clinicians need to be aware of this uncommon condition for early diagnosis and prompt aggressive treatment with steroids and etoposide based chemotherapy, which could be lifesaving. Thus better outcome relies on clinical acumen and appropriate management.
References
- Fisman DN. Hemophagocytic syndromes and infection. Emerging Infect Dis. 2000;6(6):601-608.
- Janka GE. Hemophagocytic syndromes. Blood reviews. 2007;21(5):245-253.
- Dhote R, Simon J, Papo T, Detournay B, Sailler L, Andre MH, et al. Reactive hemophagocytic syndrome in adult systemic disease: Report of twenty-six cases and literature review. Arthritis Care & Research. 2003;49(5):633-639.
- Morris JA, Adamson AR, Holt PJ, Davson J. Still’s disease and the virus associated haemophagocytic syndrome. Ann Rheumatol Dis. 1985;44:349-353
- Risdall RJ, McKenna RW, Nesbit ME, Krivit W, Balfour HH, Simmons RL, et al. Virus associated hemophagocytic syndrome. Cancer. 1979;44:993-1002.
- Rasdall RJ, Brunnng RD, Hernandez JI, Gordon DH. Bacteria associated hemophagocytic syndrome. Cancer. 1984;54:2968-2972.
- Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124.
- Rouphael NG, Talati NJ, Vaughan C, Cunningham K, Moreira R, Gould C. Infections associated with haemophagocytic syndrome. Lancet Infect Dis. 2007;7:814-822.
- Kasahara Y, Yachie A. Cell type specific infection of Epstein–Barr virus (EBV) in EBV-associated hemophagocytic lymphohistiocytosis and chronic active EBV infection. Critical Reviews in Oncology/ Hematology. 2002;44(3):283-294.
- Imashuku S, Teramura T, Tauchi H, Ishida Y, Otoh Y, Sawada M, et al. Longitudinal follow-up of patients with Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Haematologica. 2004;89:183-188.