|
|
|
|
|
Gastric Malignancy Presenting as Post-renal Acute Kidney Injury
|
|
|
H Satish, C Jaswant, BH Srinivas1, M Pazhanivel2, P Sreejith, PS Priyamvada
Department of Nephrology, Pathology1 and Gastroenterology2; Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. H Satish
Email: satish.haridasan@gmail.com
|
|
|
|
|
|
|
|
|
Received:
13-FEB-2016 |
Accepted:
13-APR-2016 |
Published Online:
25-MAY-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Retroperitoneal fibrosis (RPF) encasing the ureters, is a rare cause of post-renal acute kidney injury. Fibrosis entraps the ureters, vessels and intestine leading to abdominal pain, ascites, pedal oedema and renal failure. It can be idiopathic or secondary to several factors including drugs or malignant diseases. Index case presented with abdominal distension and abdominal pain followed by oligo-anuria. Investigations revealed autoimmune thyroiditis and bilateral hydro-ureteronephrosis due to extensive RPF. Image guided biopsy from RPF showed metastases from adenocarcinoma, later confirmed to have primary signet-ring cell carcinoma in the stomach by endoscopy and histology. Retroperitoneal fibrosis and renal failure is an uncommon presentation for an occult gastric malignancy and vice versa. |
|
|
|
|
|
Keywords :
|
Abdominal Pain, Acute Kidney Injury, Carcinoma, Retroperitoneal Fibrosis, Thyroiditis.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64ed0c0000008304000001000800 6go6ckt5b5idvals|611 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Retroperitoneal fibrosis (RPF) is a rare inflammatory disease that leads to extensive fibrosis throughout the retroperitoneum. Two-thirds of patients with retroperitoneal fibrosis are considered to have idiopathic disease and others are due to drugs, connective tissue disorders or malignancy. Also known as Ormond’s disease, sclerosing fibrosis, or sclerosing retroperitonitis, RPF is composed of proliferating fibrous tissue dissecting through adipose tissue. The branches of the common iliac vessels ensheath the abdominal aorta and ureters leading to ascites and hydroureteronephrosis.
Case Report
45 year old was admitted to this hospital with pedal oedema, abdominal distension and anuria. She was apparently normal until approximately one month before admission, when she started having abdominal distension. During next 2 weeks she developed diffuse abdominal pain and constipation. One week before admission she had facial puffiness and oliguria followed by anuria for 3 days. Other symptoms included loss of appetite, loss of weight and dyspepsia of 1 month. There was no history of vomiting, hematuria, frothing of urine, nocturia, fever, or burning micturition. She was not a diabetic or hypertensive and did not smoke, drink alcohol or use illicit drugs. There was no other clinically significant past medical history or family history.
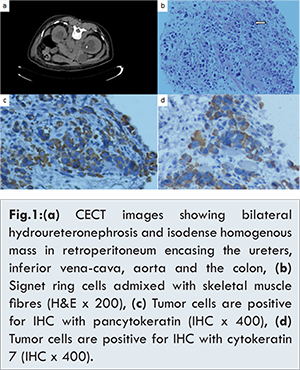
On examination she was uncomfortable with abdominal pain and shortness of breath. Blood pressure was 132/86 mm Hg, pulse rate 102 per minute, temperature was 37 degree Celsius and respiratory rate 20 per minute. She had pallor, facial puffiness, non-pitting pedal oedema and ascites. Bowel sounds were hypoactive and there was no peripheral lymphadenopathy or hepatosplenomegaly. There was a diffuse firm swelling of thyroid with delayed relaxation of ankle jerk. Her haemoglobin was 8 g/dL, total count 7.5 × 109 per L, blood urea nitrogen 26.4 mmol/L (74 mg per dL), serum creatinine 707.2 µmol/L (8 mg per dL), AST/ALT 24/20 U/L, and normal chest X-ray. Therapy was started with hemodialysis. Ultrasonography showed bilateral hydroureteronephrosis, subcentrimetric peri- and para aortic lymph nodes, gross ascites, normal bladder and no calculi. Subsequently, contrast-enhanced CT showed diffuse infiltrating isodense mass in the infrarenal area encasing the common iliac veins, inferior venacava, aorta, both ureters and the descending colon, with mild hydronephrosis [Fig.1a]. Ascitic fluid malignant cytology was negative.
She underwent double-J stenting of both ureters on 4th day of admission, following which her urine output improved, pedal oedema subsided, serum creatinine improved to 442 µmol/L (5 mg per dL) and dialysis was discontinued. Further investigation for goitre revealed TSH of 67.7 IU/L, strongly positive anti-TPO antibodies (>1300 IU/mL) and colloid goitre in guided aspiration cytology. Thyroxine 100 µg/day was initiated with a diagnosis of Hashimoto’s thyroiditis. On 7th hospital day, CT guided biopsy of retroperitoneal mass was done. Histopathology showed fibrous tissue infiltrated by tumour cells positive for pan cytokeratin (CK) and CK 7 and negative for CK 20 and CA 125 suggesting adenocarcinomatous deposits [Fig. 1b-d].
In search for an occult primary and symptoms of persistent anorexia with dyspepsia, an upper GI endoscopy was done. There were oedematous and thickened gastric folds with nodularity in the stomach, and biopsy specimen was taken from a suspicious area. Histopathology revealed poorly differentiated signet ring cell carcinoma of stomach [Fig 2].
Discussion
Retroperitoneal fibrosis is a rare clinical condition characterized by the presence of pathologic collagen plaque around the abdominal aorta and iliac vessels, as well as the inferior vena-cava and the ureters. In most cases of RPF secondary to malignant disease, abnormal collagen plaque in the retroperitoneum results from an exuberant desmoplastic response to retroperitoneal metastases. Macroscopically, RPF appears as a grey-white fibrous plaque usually arising between the level of aorta and iliac arteries in the retroperitoneal space. There are reports of association of RPF with gastrointestinal malignancies and with Hashimoto’s thyroiditis. Neither the appearance of the mass nor localization permits definitive differentiation between benign lesions and malignancies such as lymphoma, sarcoma or metastatic adenopathy. In CT scan, features suggestive of RPF is the ring of soft tissue around aorta and inferior venacava between level of kidney and sacrum, spreading to involve the ureters, causing varying degrees of obstruction. The fat plane between the mass and the psoas muscle is obliterated and RPF tends not to displace aorta anteriorly. The mass may show varying degrees of enhancement depending on the stage of the disease. Our patient who presented with AKI and ascites had Hashimoto’s thyroiditis and extensive RPF due to metastases from unknown primary. Flank pain, constipation, ascites and pedal oedema were possibly due to encasement of the inferior vena-cava and colon by fibrotic tissue.
Retroperitoneal fibrosis is etiologically classified as primary idiopathic or secondary to known causes. Primary RPF, supposed to be due to lipid leak through arterial wall, is associated with several autoimmune diseases including Hashimoto’s thyroiditis [ 1]. Among the secondary causes for RPF, malignancies like carcinoid, lymphoma and retroperitoneal metastases (breast, lung, thyroid, GI tract) can incite desmoplastic response culminating in fibrosis. So, in such a scenario RPF is an advanced metastatic stage of malignancy. Histopathology of RPF with special stains is indicated to establish the diagnosis. The cytokeratin 7/20 profile of a particular tumor has proved to be a useful aid in differential diagnosis of carcinomas, since primary and metastatic tumours tend to retain the cytokeratin profiles of the epithelium from which they arise. Cytokeratins are group of approximately 20 proteins that consist of a type of intermediate filament and are differentially expressed in epithelia. In a recent study by Bayrak et al. the largest proportion of gastric carcinomas was of the CK7+/CK20+ phenotype (48%), and a substantial proportion was of the CK7+/CK20- phenotype (32%) [ 2], which was the pattern in this case.
The RPF secondary to gastric malignancy is associated with poor prognosis. From our knowledge, there are only ten reported cases of gastric carcinoma presenting with RPF [ 3- 6]. Among the gastric malignancies, signet ring cell carcinoma appears to present at later stages, with a greater proportion of patients presenting at advanced TNM stage, and higher tumor grade. Management of metastatic gastric adenocarcinoma is palliative chemotherapy in view of radio resistance of carcinoma stomach but our patient could not receive chemotherapy in view of renal failure. Although corticosteroid is the treatment for idiopathic RPF, there is no evidence of effectiveness when RPF is secondary to malignancy. The index case is an uncommon presentation of carcinoma stomach as AKI due to RPF. Our patient was planned for supportive care after consultation with oncology. In conclusion, retroperitoneal fibrosis is an important cause for post-renal AKI, and all suspicious cases should undergo retroperitoneal biopsy with tumor markers. One should meticulously search for occult malignancies even in presence of common associated conditions like Hashimoto’s thyroiditis.
References
- Lee JE, Han SH, Kim DK, Moon SJ, Choi KH, Lee HY, et al. Idiopathic retroperitoneal fibrosis associated with Hashimoto’s thyroiditis in an old age man. Yonsei Med J. 2008;49:1032-1035.
- Bayrak R, Hacer H, Sibel Y. The value of CDX2 and cytokeratins 7 and 20 expression in differentiating colorectal adenocarcinomas from extraintestinal gastrointestinal adenocarcinomas: cytokeratin 7-/ 20+ phenotype is more specific than CDX2 antibody. Diagnostic Pathology. 2012;7:9.
- Yokoyama R, Tazaki R, Morita H, Nishitani H, Ariumi S, Osuga S, et al. Retroperitoneal fibrosis in a patient with gastric cancer manifested by lower extremity edema and hydrocele. Intern Med. 2012;51:2157-2160.
- Karbasi A, Karbasi-Afshar R, Ahmadi J, Saburi A, et al. Retroperitoneal fibrosis as a result of signet ring cell gastric cancer: a case-based review. J Gastrointest Cancer. 2013;44:94-97.
- Amrouche L, Gornet JM, Lascoux C, George C, Florea L, Farge D, et al. From retroperitoneal fibrosis to gastric linitis. Rev Med Interne. 2009; 30:443-445.
- Peixoto RD, Al-Barrak J, Lim H, Renouf D. Gastroesophageal cancer and retroperitoneal fibrosis: Two case reports and review of the literature. World J Gastrointest Oncol. 2013;5(3):68-70.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Satish H, Jaswant C, Srinivas BH, Pazhanivel M, Sreejith P, Priyamvada PSGastric Malignancy Presenting as Post-renal Acute Kidney Injury.JCR 2016;6:222-225 |
|
Satish H, Jaswant C, Srinivas BH, Pazhanivel M, Sreejith P, Priyamvada PSGastric Malignancy Presenting as Post-renal Acute Kidney Injury.JCR [serial online] 2016[cited 2025 Apr 26];6:222-225. Available from: http://www.casereports.in/articles/6/2/Gastric-Malignancy-Presenting-as-Post-renal-Acute-Kidney-Injury.html |

|
|
|
|
|