Introduction
Rosacea is a chronic acneiform disorder affecting the skin and eyes [
1]. Skin findings in rosacea vary from flushing, nontransient erythema and telangiectasia, papules, pustules to phymatous changes [
2,
3]. Ocular findings in rosacea include telangiectasia and erythema of the lid margin, meibomian gland dysfunction, conjunctival hyperemia, episcleritis, scleritis, peripheral corneal infiltrates/vascularization, superficial punctate keratitis, or even perforation [
1-
3].
Rosacea is generally found in patients aged 30-60 years old with a slight female preponderance, although it can be encountered in younger patients and is often underdiagnosed [
1]. Rosacea appears to be quite common in fair-skinned people [
1,
2], affecting as many as 14 million people in the United States, and has 10% prevalence in Sweden [
2,
4]. There is no current data from Asian countries [
5]. Ocular rosacea affects half of more of patients with rosacea, although an incidence as low as 8% has recently been reported [
3].
Although it has relatively frequent association with blepharitis and/or aqueous tear dysfunction, it is infrequently diagnosed by ophthalmologists. This case series aim to highlight ocular rosacea as one of the causes of external ocular problem. Better understanding of diagnosis and management will produce better outcome of ocular rosacea in daily clinical practice.
Case Report
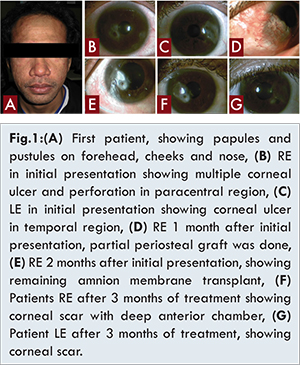
Two cases of corneal ulcer due to ocular rosacea were observed. First case was 34-year old male who presented with multiple corneal ulcers on both eyes sparing visual axis, epithelized corneal perforation of right eye, and severe acne [Fig.1]. There were episodes of recurrent red eye, facial and chest acne since last 10 years and at times had transient episodes of flushing, especially after exposure to hot air. He was diagnosed as bilateral multiple corneal ulcers with epithelized perforated corneal ulcer of right eye (RE), and was treated with levofloxacin ED 6xBE, timolol maleate 0.5% 2xRE, sulphas atrophine 1% 3xRE, and underwent partial periosteal graft of RE. Three weeks postoperatively, periosteal graft was detached with loose suture, exposing epithelial defect size 1x1.5 mm without any infiltrates. Anterior chamber was deep, and pupil was slightly retracted to wound site. Corneal infiltrate on left eye (LE) has disappeared, but there were neovascularization and corneal scar. First suspicion of ocular rosacea was noted 5 weeks after his initial presentation. Patient was consulted to dermatology department and was assessed as severe acne vulgaris, treated with clindamycin 2x300 mg. Two weeks afterward, there were multiple corneal ulcers on RE; with the largest size 3x3 mm, perforated and located in temporal aspect. There were also multiple corneal ulcers on LE, each measuring 2 mm. Despite assessment from dermatovenerology department, the patient was diagnosed as ocular rosacea and treated with levofloxacin ED hourly RE, 6xLE, artificial tears 6xBE, sulphas atropine 1% 3xBE, bandage lens of RE, and doxycycline 2x100 mg. One week afterwards patient showed signs of improvement, but perforation occurred on the following week. He then underwent amnion membrane transplantation, and showed signs of improvement. Afterwards, he was lost to follow up. Seven months following his last visit, the patient came again with bilateral blepharoconjunctivitis. He was not on any medication. He was then treated with antibiotic and steroid ED 6xBE, chloramphenicol EO 3xBE, artificial tears 6xBE, and doxycycline 2x100 mg. Two weeks afterward all signs and symptoms have diminished and visual acuity was 6/7.5 RE and 6/9.5 LE.
Second case was 14 years old girl who presented with corneal ulcer of RE, recurrent redness of RE since last 3 months and accompanied with stinging sensation of chin, cheeks and nose since 10 months before admission [Fig.2] which exacerbated mostly after sunlight exposure, during menstrual periods, and after consumption of spicy food. Physical examination showed visual acuity of 3/60 RE and 6/6 left eye (LE). There was central corneal ulcer of RE extending to inferonasal size 4x3 mm, 2/3 stromal depth with positive fluorescein staining and neovascularization, meibomian gland dysfunction grade II was also present. Gram stain showed gram-positive cocci. The patient was initially diagnosed as bacterial corneal ulcer and was given levofloxacin ED hourly RE, gentamycin EO 2xRE, sulphase atrophine 1% 3xRE, timolol maleate 0.5% ED 2xRE and artificial tears 3xRE. One week afterwards, visual acuity was 6/24 on RE and 6/6 on LE. There were corneal epithelial defect with signs of epithelization. She was assessed as corneal ulcer rosacea RE, and was given levofloxacin ED 4xRE, prednisolone acetate 4xRE, timolol maleate 0.5% 2xRE, artificial tears ED 3xRE, and doxycycline 2x100 mg. Ten days afterwards, visual acuity was 6/18 on RE and epithelial defect was reduced. Patient was consulted to dermatovenerology department and assessed with acne rosacea, was given SPF 30 sunblock and AHA 10% twice daily. She came again 22 days after starting doxycycline therapy and admits that pain on her eyes has diminished. Visual acuity was 6/18 on RE, eyelid and bulbar conjunctiva were quiet and there were only corneal scar and neovascularization on RE.
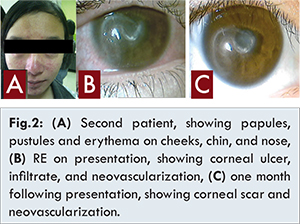
Both patients were given doxycycline 2x100 mg after diagnosed as ocular rosacea. Time from first presentation to diagnosis of ocular rosacea was 8 weeks for first patient while one week for second patient. Both patients were also given artificial tears, antibiotic, and steroid eye drops. Our first patient underwent two surgical interventions; partial periosteal graft and amnion membrane transplant, while second patient did not require surgical intervention.
Final best corrected visual acuity (BCVA) of first patient was 6/6 on right eye and 6/9 on left eye 3 months after surgery and medication. Final BCVA of second patient was 6/18 on RE after 1 month of medication. Visual acuity of first patient was not much affected in both eyes despite history of recurring perforated corneal ulcer due to the lesion being out of the visual axis. In second patient although the diagnosis was made earlier, not much improvement in vision was due to the lesion affecting central part of the cornea. On both patients, eyes and skin lesions improved significantly after treatment with oral doxycycline.
Discussion
Ocular rosacea is most frequently diagnosed when cutaneous signs and symptoms are present; however it is not perquisite of diagnosis. Ocular manifestation may occur before cutaneous manifestation in up to 20% of cases [
2]. Corneal involvement in ocular rosacea is quite rare, Akpep et al. [
6] shows that corneal involvement of varying degree occur in 41% of patients. However, 5% develop corneal ulcer, and 1.5% develop perforation [
6]. Lack of classic cutaneous sign in corneal ulcer caused by ocular rosacea may delay diagnosis of ocular rosacea, and therefore withhold doxycycline treatment.
In first patient papuopustular skin manifestations, mixed with those of acne vulgaris were present, which usually differentiated by the absence of comedones in rosacea. However, both rosacea and acne may occur concomitantly, and such patients may have comedones as well [
2]. Cutaneous signs in second patient are more typical, and therefore diagnosis of ocular rosacea were made much faster. Considering that in 20% of patients ocular signs may precede cutaneous signs, suspicion of ocular rosacea shall be raised in patients with peripheral ulcerative keratitis and sterile corneal ulcer. Trial of doxycycline therapy may be given in such patients and improvement of signs and symptoms may confirm the diagnosis of ocular rosacea.
The mainstay therapy of ocular rosacea is tetracyclines, which have anti-inflammatory properties that include suppression of leukocyte migration, reduced production of nitric oxide and reactive oxygen species, inhibition of matrix metalloproteinases, and inhibition of phospholipase A2. In addition, tetracycline may reduce irritative free fatty acids and diglycerides by suppressing bacterial lipases [
1]. The most common drugs currently used (tetracycline, doxycycline, minocycline) have never been tested to placebo and therefore the dosing is empirical. Alvarenga suggested the use of doxycycline, 100 mg twice daily for 2-3 weeks, then tapering to 100 mg/day and later to 50 and 25 mg per day [
3]. Tetracyclines however, are contraindicated for patients under 8 years old [
7,
8]. Miguel et al. suggested the use of erythromycin for patients under 8 years old, and used it on their case series of two patients. In his study, Chammaillard et al. [
7] used metronidazole for patients below 12 years old, stating that the use of erythromycin in their clinical practice resulted in partial remission of ocular rosacea symptoms that may lead to recurrence of symptoms soon [
7]. Other systemic medications (metronidazole, clindamycin, erythromycin, clarithromycin, ampicillin, retinoids, clonidine, rilmenidine) have been used with success [
3].
Ocular topical therapy ranges from artificial tears, nonsteroid anti-inflammatory drugs, corticosteroids, combination of antibiotic/anti-inflammatory suspensions and ointments, antibiotics, and cyclosporine ophthalmic emulsion based on the specific problem [
4]. The use of lubricants in patients with ocular rosacea helps decrease inflammatory reaction that is triggered by dry environment and help increase tear clearance, thereby decreasing inflammatory mediators. Non-preserved artificial tears are preferable, and the ideal dosage should be individually tailored. Ideally it shall be used with high frequency initially and then tapered. Patient compliance can be low when frequent long term dosing is needed, and therefore needs constant reassurance of the importance of treatment [
3].
Ulcerative keratitis in rosacea can have sterile inflammation etiology or caused by infectious agents. Once it is ascertain that ulceration is noninfectious, topical steroid can play a significant role in reducing sterile inflammation and enhancing epithelization of the cornea, but it shall be used judiciously [
1,
3].
Conclusion
Early diagnosis of ocular rosacea will allow better and prompt treatment, prevent devastating complications that might cause severe visual loss, shorten the length of therapy, and lessen the number of procedures. Suspicion of ocular rosacea shall be raised in patients with peripheral ulcerative keratitis and sterile corneal ulcer without any typical skin manifestation of rosacea. Trial of doxycycline therapy may be given in such patient and improvement of signs and symptoms may confirm the diagnosis of ocular rosacea.
References
- American Academy of Ophthalmology Staff. Ocular surface disease: diagnostic approach, In: American Academy of Ophthalmology Staff. External eye disease and cornea. San Francisco: American Academy of Ophthalmology; 2011-2012. p. 69-71.
- Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002;46:584-587.
- Alvarenga LO, Mannis MJ. Ocular Rosacea. The Ocular Surface 2005;3(1):41-58.
- Oltz M, James C. Rosacea and its ocular manifestation. Optometry. 2011;82:92-103.
- Tan J, Berg M. Rosacea: current state of epidemiology. J Am Acad Dermatol. 2013;69:S27-35.
- Akpep EK, Merchant A, Pinar V, Foster CS. Ocular rosacea patient characteristic and follow up. Optometry. 2011;82:92-103.
- Chamailard M, Mortemesque B, Boralevi F, Da Costa CM, Aitali F, Taieb A. Cutaneous and ocular signs of childhood rosacea. Arch Dermatol. 2008;144(2):167-171.
- Miguel AIM, Salgado, MB, Lisboa MS, Henriques F, Paiva MC, Castela GPL. Pediatric ocular rosacea: 2 cases. Eur J Ophthalmol. 2012;22 (4):664-666.