|
|
|
|
|
A Rare Case of Metastasis of Merkel Cell Carcinoma to the Jejunum
|
|
|
Yuta Ogura1, Takeharu Enomoto1, Shinya Mikami1, Hiroyuki Hoshino1, Akiyoshi Noda1, Osamu Saji1, Tsunehisa Matsushita1, Shinya Ishigouoka2, Masaki Yamashita2, Saeko Naruki3, Takashi Fujino3, Tetsu Fukunaga1, Takehito Otsubo1
1Division of Gastroenterological and General Surgery, 2Division of Gastroenterological Internal Medicine, 3Department of Pathology; St. Marianna University School of Medicine, Kawasaki, Japan. |
|
|
|
|
|
Corresponding Author:
|
Dr. Takeharu Enomoto
Email: takeharu@marianna-u.ac.jp
|
|
|
|
|
|
|
|
|
Received:
31-MAR-2016 |
Accepted:
08-JUN-2016 |
Published Online:
15-AUG-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
We describe a rare case of metastasis of Merkel cell carcinoma (MCC) to the jejunum. The patient was a 79-year-old man with a chief complaint of dizziness and palpitation. He sought medical attention 3 days after the dizziness and palpitation had manifested and was admitted to our hospital. His medical history included MCC, prostate carcinoma, abdominal aortic aneurysm, and stroke. We performed an enteroscopic examination and found a neoplastic lesion in the upper jejunum. Evidence of bleeding led us to perform emergency laparoscopic surgery. Pathologic examination revealed small round cells forming a nodule, and immunostaining for epithelial marker CK20 and neuroendocrine marker synaptophysin were positive. The final diagnosis based on histopathologic examination of the resected jejunal tumor was metastatic MCC. Such metastasis is indeed rare, and we consider our patient’s tumor in light of the literature. |
|
|
|
|
|
Keywords :
|
Dizziness, Jejunum, Laparoscopy, Merkel Cell Carcinoma, Skin Neoplasms, Stroke.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff685e0f0000008c03000001000500 6go6ckt5b5idvals|647 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Merkel cell carcinoma (MCC) is a neuroendocrine carcinoma that arises in the dermoepidermal junction. It is an uncommon but aggressive skin cancer. The prognosis is poor because the cancer often metastasizes to lymph nodes and distant organs such as the liver, lungs, bone and brain. We report an unusual case of metastasis to the jejunum.
Case Report
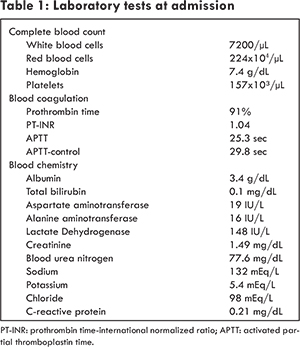
The patient was a 79-year-old man with a chief complaint of dizziness and palpitation. He also complained of sporadic passage of dark, tarry stools over a period of a few months. He sought medical attention 3 days after the dizziness and palpitation had manifested and was admitted to our hospital. His medical history included MCC of the right arm, prostate carcinoma, abdominal aortic aneurysm and stroke. Laboratory tests performed upon admission revealed anemia and dehydration [Table 1]. We performed upper endoscopy, colonoscopy, and computed tomography, the results of which were negative. Unexplained anemia prompted us to perform an enteroscopic examination, and in so doing, we found a neoplastic lesion in the upper jejunum. Contrast-enhanced computed tomography revealed stenosis of the small bowel [Fig.1]. We decided to perform emergency laparoscopic surgery. In first examining the abdominal cavity, we recognized a tumor that was located approximately 60 cm from the Treitz ligament on the anal side. Thus, we resected part of the jejunum and anastomosed the two cut ends by the Gambee technique. We were satisfied that the ulceration had been confined to the tumor.
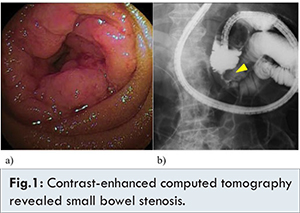
The lesion was 25x21 mm. Pathologic examination revealed small round cells forming a nodule, and immunostaining for epithelial marker CK20 and neuroendocrine marker synaptophysin were positive [Fig.2]. Lymphoid markers CD3 and CD20 and thyroid transcription factor 1 (TTF-1) were negative. The final diagnosis based on histopathologic examination of the resected jejunal tumor was metastatic MCC.
The post-operative course was good, and the patient was discharged 12 days after surgery. Currently, chemotherapy and radiotherapy are considered ineffective for MCC of the jejunum. Thus, we did not administer chemotherapy or radiotherapy postoperatively. Follow-up at eight months have shown no sign of recurrence.
Discussion
Merkel cells are dermal sensory receptors at the basal epidermal layer and were first described by Frederick Merkel in 1875. Surrounding unmyelinated cutaneous nerve endings, Merkel cells are thought to be involved in contact sensation. MCC was first reported by Toker in 1972. Discovery by Tang and Toker of a distinctive core of dense granules in the cytoplasm of the tumor cells allowed the entity to be defined as a neuroendocrine cell tumor derived from Merkel cells [ 1, 2].
Clinically, the lesions are most likely to appear in areas of sun exposure, especially around the eyelids and on the extremities in the elderly. Lesions are described as indolent, glossy, bright red to rose nodes that increase in size within a short time period [ 2, 3]. Exposure to ultraviolet light and immunosuppression are implicated in the development of MCC [4]. Immunohistologically, MCC is positive for neural system markers chromogranin A and synaptophysin and epithelial marker cytokeratin-20. Staining for CK20 yields a characteristic perinuclear speckled pattern. MCC is negative for lymphocyte markers and S100 protein and also for TTF-1, a transcription factor expressed specifically in lungs and thyroid [ 5].
The current approach to treatment of MCC includes extensive resection, lymph node dissection, and radiation or chemotherapy. Randomized clinical trials for MCC have not been conducted to date, and the gold standard for treatment of the carcinoma is yet to be established [ 4]. The regional recurrence rate is 25%, and the distant metastasis rate is 35%. The main sites of metastasis are the dermis, lymph nodes, liver, lungs, bones, and brain. Metastasis to the digestive tract including the small intestine is extremely rare [ 2, 3, 6]. Recurrence often occurs even for early-stage MCC, and the prognosis is poor. Progression is unpredictable because regional recurrence and local lymph node metastasis are quite indolent. Reports of metastasis of MCC to the small intestine are few. A search of the literature turned up only 5 cases in the US and Japan, including the case we report herein [Table 2]. Median age of the patients was 66.7 years, and all of the initial nodules appeared on the extremities and face [ 3, 4, 6- 10].
It is reasonable to surmise that the pathways of metastasis are lymphogenous and/or hematogenous, considering the fact that proximal lymph node metastasis has preceded digestive tract or multiple organ metastasis in every case. As noted above, the gold standard for treatment of MCC is yet to be established. At the first occurrence of MCC in our patient, radiation was delivered to the tumor area in the axilla and front of the right arm, but recurrent lesions were found in the same area of the right arm and in the small intestine. Eight months have passed since the enterectomy, no radiation or chemotherapy has been administered, and the postoperative course thus far has been uneventful. The potential for recurrence and multiple organ metastasis is high in cases of MCC. Thus, regular hospital visits and follow-up imaging studies are important for MCC patients. Abdominal symptoms in patients with a history of MCC can indicate metastasis to the small intestine.
Conclusion
In searching the literature published both in and outside of Japan, we found only two reported cases of metastasis of MCC to the jejunum. Although such metastasis is rare, our encounter with it leads us to believe that this distinct clinical entity should be brought to the attention of physicians, surgeons, and gastrointestinal pathologists who may encounter MCC in clinical practice.
Acknowledgment
We thank Tina Tajima for her critical reading of the manuscript.
References
- Toker C. Trabecular carcinoma of the skin. Arch. Dermatol. 1972;105:107-110.
- Wada N, Kawasaki M, Ogawa M, et al. A case of Merkel cell carcinoma of an axillary lymph node [In Japanese with English abstract]. Nihon Rinsho Geka Gakkai Zasshi. 2011;72:2813-2816.
- Matkowskyj KA, Hosseini A, Linn JG, Yang GY, Kuzel TM, Wayne JD. Merkel cell carcinoma metastatic to the small bowel mesentery. Rare Tumors. 2011;3:e2.
- Canales LI, Parker A, Kadakia S. Upper gastrointestinal bleeding from Merkel cell carcinoma. Am. J. Gastroenterol. 1992;87:1464-1466.
- Hizawa K, Kurihara S, Nakamori M, Nakahara T, Matsumoto T, Iida M. An autopsy case of Merkel cell carcinoma presenting aggressive intraabdominal metastasis and duodenal obstruction. Nihon Shokakibyo Gakkai Zasshi. 2007;104:1383-1386.
- Naunton Morgan TC, Henderson RG. Small bowel metastases from a Merkel cell tumor. Br J Radiol. 1985;58:1212-1213.
- Foster R, Stevens G, Egan M. An unusual pattern of metastases from Merkel cell carcinoma. Australas Radiol. 1994;38:231-232.
- Shalhub S, Clarke L, Morgan MB. Metastatic Merkel cell carcinoma masquerading as colon cancer. Gastrointest Endosc. 2004;60:856-858.
- Cheung M, Lee H, Purkayastha S, Goldin R, Ziprin P. Ileocaecal recurrence of Merkel cell carcinoma of the skin: A case report. J Med Case Rep. 2010;4:43-47.
- Olivero G, Franchello A, Pacchioni D, Enrichens F, Mao P, Benedetto G. A rare case of Merkel’s tumor with intestinal metastases. Ann Ital Chir. 1990;61:277-280.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Ogura Y, Enomoto T, Mikami S, Hoshino H, Noda A, Saji O, Matsushita T, Ishigouoka S, Yamashita M, Naruki S, Fujino T, Fukunaga T, Otsubo TA Rare Case of Metastasis of Merkel Cell Carcinoma to the Jejunum.JCR 2016;6:378-381 |
|
Ogura Y, Enomoto T, Mikami S, Hoshino H, Noda A, Saji O, Matsushita T, Ishigouoka S, Yamashita M, Naruki S, Fujino T, Fukunaga T, Otsubo TA Rare Case of Metastasis of Merkel Cell Carcinoma to the Jejunum.JCR [serial online] 2016[cited 2026 Jan 5];6:378-381. Available from: http://www.casereports.in/articles/6/3/A-Rare-Case-of-Metastasis-of-Merkel-Cell-Carcinoma-to-the-Jejunum.html |

|
|
|
|
|