|
|
|
|
|
Bilateral Cataract: Unusual Manifestation of Type 1 Diabetes Mellitus
|
|
|
mixing lexapro and weed mixing lexapro and weed link
Department of Medicine and 1Radiodiagnosis, King George’s Medical College, Lucknow, Uttar Pradesh, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Manish Gutch
Email: manish07gutch@gmail.com
|
|
|
|
|
|
|
|
|
Received:
13-JAN-2016 |
Accepted:
26-MAY-2016 |
Published Online:
05-AUG-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Diabetes is a well-known causative factor for cataract in both developing and developed countries. Diabetic patients also have higher risk of both operative and post-operative complications. However early detection of diabetes in young patients along with strict diabetic control can minimise the risk of development of cataract. Though drugs like aldose reductase inhibitors and other antioxidants have been found to be beneficial, their clinical efficacy is still uncertain. We hereby describe a rare case of bilateral cataract in a patient of type 1 diabetes mellitus in a young female. |
|
|
|
|
|
Keywords :
|
Aldehyde Reductase, Antioxidants, Cataract, Type 1 Diabetes Mellitus, Diabetic Ketoacidosis.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe81f0f000000cc04000001000700 6go6ckt5b5idvals|644 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Type 1 diabetes is a common disease usually diagnosed in young. The prevalence of type 1 diabetes mellitus (T1DM) is also on increase like type 2 diabetes with a trend of 3%-5% increase/year [1]. India has three new cases of T1DM/100,000 in children aged 0-14 years [1-3]. T1DM may be autoimmune or idiopathic in nature and is present in 9% cases of insulin deficiency [1-3]. T1DM is primarily caused by genetic factors, environmental factors, and disorders of the immune regulatory mechanism. A combination of all these factors causes autoimmune destruction of pancreatic beta cells and insulin deficiency leading to hyperglycemia, ketoacidosis and potentially death, if not treated with insulin. The pathogenesis of development of cataract in diabetic patients primarily involves the polyol pathway. Intracellular accumulation of glucose in conditions of uncontrolled blood sugar levels leads to conversion of glucose to sorbitol catalysed by the enzyme aldose reductase. Accumulation of sorbitol increases osmotic content in lens causing increased fluid accumulation and hydropic lens fibres. Also the polar nature of the sorbitol prevents diffusion of sorbitol out of the lens further enhancing the effect [4-6]. Here we describe a rare case of a young girl suffering from T1DM with development of bilateral cataract without any underlying retinopathy.
Case Report
A 13 year old girl weighing 30 kg presented to the emergency department in altered sensorium following decreased appetite and vomiting since 15 days. Besides this, her vision had gradually deteriorated over the previous 6 months. There was no history of fever, headache, trauma, convulsions or any focal neurological deficit. On examination, her vitals were stable. Glasgow Coma Scale (GCS) score was 7 (E2V2M3), pupils were bilaterally normally reactive to light. Plantar response was normal (bilaterally flexor) and meningeal signs were absent. She exhibited Kussmaul’s pattern of breathing. Rest of the systemic examination was within normal limits.
Investigations revealed high blood glucose levels (430 mg/dL), acidosis (pH = 6.9), low serum bicarbonate levels (3.2 mmol/L) with ketones detectable in urine by dipstick method (3+). Glycosylated haemoglobin (HbA1c) was 11.5%. Other routine investigations including hemogram, electrolytes, liver and renal functions were within normal limits. A provisional diagnosis of diabetic ketoacidosis was made and she was immediately treated with intravenous fluids, insulin infusion and other supportive measures. Her vitals, electrolytes and urine output were timely monitored. She regained full consciousness within the next 24 hours and was subsequently shifted to subcutaneous insulin regimen when she resumed oral feeding. On further screening, glutamic acid decarboxylase (GAD-65) antibodies were detected. Thus we labelled her as a case of newly detected type 1 diabetes mellitus presenting for the first time with diabetic ketoacidosis [14].
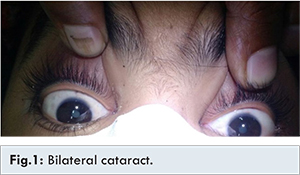
Even after achieving euglycemia and resolution of acidosis, her complain of decreased visual acuity persisted. We subsequently discovered that she had developed bilateral cataract [Fig.1]. Visual acuity was 6/24 in both eyes. Pupillary reaction to light was normal bilaterally. On slit-lamp examination, posterior subcapsular opacity was present suggestive of presence of posterior subcapsular cataract bilaterally. On fundus examination after attaining full mydriasis, the optic disc was normal in shape and size, pink, vertically oval with C:D ratio (cup: disc) of 0.3 and clear margins. The A:V ratio (artery:vein) was normal (2:3). Macula was within normal limits and there was no evidence of diabetic retinopathy (haemorrhage, exudation, etc.). No abnormality was found on fundus fluorescein angiography.
After rendering her euglycemic with regular Insulin therapy, we referred her to the ophthalmology department for surgical intervention. After cataract surgery, her vision normalised to 6/6 in both eyes. Presently she is maintaining good glycaemic control by being compliant to her prescribed insulin regimen.
Discussion
Diabetes is an emerging epidemic in India with an estimated 62 million people affected. The conventional risk factors of urbanisation, unhealthy eating habits, physical inactivity and inherent genetic attributes all contribute to increasing prevalence of diabetes [7-10]. Subsequently the prevalence of microvascular and macrovascular complications of diabetes is also on the rise. The prevalence of diabetes in India is reported to range from 5.3% to 13.6% [7-10]. Cataract development is an early complication of diabetes mellitus. Klein et al. [11] showed that diabetic patients are 2-3 times more likely to develop cataract than their normal counterparts. The risk is more (about 15-25 times) in young diabetics aged less than 40 years [7-10].
The three main mechanisms involved in the development of cataract are the activated polyol pathway, oxidative stress and accumulation of non-enzymatic glycation end products (AGES). The basement membrane of the lens is thickened and friable in diabetics. Many studies have compared the incidence of cataract in both diabetics and non-diabetics. Saxena et al. [12] observed two fold higher incidence of cortical cataract in patients whose blood glucose levels were uncontrolled for more than 5 years. Posterior sub-capsular cataracts were found to be more common in these patients. Snowflake cataract, also called as true diabetic cataract, is less common and consists of widespread bilateral subcapsular opacities. It usually presents as rapidly progressive visual loss in young diabetics with uncontrolled blood glucose levels. Bilateral cataract can also be the initial presentation in many young diabetics. There is an increased risk of development of macular edema and progression of diabetic retinopathy in these patients [7,13].
According to the Wisconsin epidemiologic study of diabetic retinopathy, the incidence of cataract surgery after 10 years of follow up was 8.3% in type 1 diabetes and 24.9% in type 2 diabetes patients [7,9]. Ketoacidosis is an independent risk factor for cataract formation as it decreases the availability of antioxidants. A few studies have observed an increased risk of cataract in females, reasons yet unknown. The risk is amplified in patients who have deranged HbA1c levels and prolonged symptoms of diabetes [13].
Our patient, a young teenage girl, presented with diabetic ketoacidosis as the first presenting feature of T1DM. Subsequently we discovered she had developed bilateral cataract, signifying uncontrolled blood glucose levels over the past many years. Hence the development of cataract in a young individual must prompt the treating physician to rule out underlying metabolic abnormalities, diabetes mellitus being the commonest of them all.
Conclusion
Development of cataract is one among the many complications associated with uncontrolled diabetes. It may be the initial presenting feature of diabetes, especially in children presenting with gradually progressive decline of vision. Strict blood glucose control can prevent the development of cataract and other ophthalmological complications of diabetes mellitus.
References
- Das AK. Type 1 diabetes in India: Overall insights. Indian J Endocr Metab. 2015;19:Suppl S1:31-33.
- Gutch M, Razi SM, Kumar S, Gupta KK. Diabetes mellitus: Trends in northern India. Indian J Endocrinol Metab. 2014;18:731-734.
- Gutch M, Kumar S, Saran S, Gupta KK, Mohd Razi S, Philip R. Prevalence of autoimmune disorders in pediatrics type-1 diabetes mellitus in Western Uttar Pradesh, India. Int J Med Public Health. 2015;5(1):29-31.
- Agroiya P, Philip R, Saran S, Gutch M, Tyagi R, et al. Association of serum lipids with diabetic retinopathy in type 2 diabetes. Indian J Endocrinol Metab. 2013;17: S335-S337.
- Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001;44:156-163.
- Harding JJ, Egerton M, van Heyningen R, Harding RS. Diabetes, glaucoma, sex, and cataract: analysis of combined data from two case control studies. Br J Ophthalmol. 1993;77:2-6.
- Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022-3027.
- Huffman MD, Prabhakaran D, Osmond C, Fall CH, Tandon N, Lakshmy R, et al. Incidence of cardiovascular risk factors in an Indian urban cohort results from the New Delhi birth cohort. J Am Coll Cardiol. 2011;57:1765-1774.
- Mohan V, Deepa M, Anjana RM, Lanthorn H, Deepa R. Incidence of diabetes and pre-diabetes in a selected urban south Indian population (CUPS-19). J Assoc Physicians India. 2008;56:152-157.
- Mohan V, Deepa M, Deepa R, Shanthirani CS, Farooq S, Ganesan A, et al. Secular trends in the prevalence of diabetes and impaired glucose tolerance in urban South India--the Chennai Urban Rural Epidemiology Study (CURES-17). Diabetologia. 2006;49:1175-1178.
- Wang JJ, Klein R, Smith W, Klein BE, Tomany S, Mitchell P. Cataract surgery and 5 year incidence of late stage age related maculopathy. Pooled findings from Beaver Dams and Blue Mountains eye studies. Ophthalmology. 2003;110:1960-1967
- Saxena S, Mitchell P, Rochtchina E. Five-year incidence of cataract in older persons with diabetes and pre-diabetes. Ophthalmic Epidemiol. 2004;11:271-277.
- Kumar P, Krishna P, Reddy SC, Gurappa M, Aravind SR, Munichoodappa C. Incidence of type 1 diabetes mellitus and associated complications among children and young adults: Results from Karnataka Diabetes Registry 1995-2008. J Indian Med Assoc. 2008;106:708-711.
- Pihoker C, Gilliam l, Hampe C, Lernmark A. Autoantibodies in diabetes. Diabetes. 2005;54:S52-61.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Gutch M, Kumar S, Bhattacharjee A, Chawla H, Singh HBilateral Cataract: Unusual Manifestation of Type 1 Diabetes Mellitus.JCR 2016;6:366-369 |
|
Gutch M, Kumar S, Bhattacharjee A, Chawla H, Singh HBilateral Cataract: Unusual Manifestation of Type 1 Diabetes Mellitus.JCR [serial online] 2016[cited 2025 Jun 21];6:366-369. Available from: http://www.casereports.in/articles/6/3/Bilateral-Cataract.html |

|
|
|
|
|