|
|
|
|
|
Combination Therapy: Promising Rationale for Alzheimer’s Disease
|
|
|
Xuekai Zhang1, Jing Shi1, Ting Li1, Mingqing Wei1, Jingnian Ni1, Yongyan Wang2, Jinzhou Tian1
1BUCM Neurology Centre, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing 100700, China; 2Institute of Clinical Medicine, China Academy of Chinese Medical Sciences, Beijing 100700, China. |
|
|
|
|
|
Corresponding Author:
|
Dr. Jinzhou Tian
Email: jztian@hotmail.com
|
|
|
|
|
|
|
|
|
Received:
30-MAY-2016 |
Accepted:
23-AUG-2016 |
Published Online:
25-SEP-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
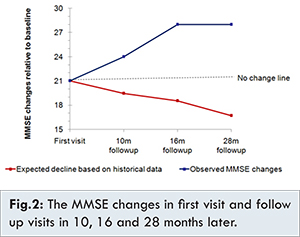
Donepezil treatment may associated with slow cognitive decline effects for a limited period of time in Alzheimer’s disease (AD). We report a 78 year old highly educated man of mild to moderate probable AD treated by a combination therapy of donepezil, nicergoline, nimodipine and TCM herbal therapy. His cognitive function and global status improved slowly over 2.5 years, from 21 scores on MMSE at first visit to 28 scores on MMSE at final visit. The diagnosis of AD was made mainly based on his complaint of memory loss, hidden onset, and gradually increased medical history, objective evidence of neuropsychological tests demonstrating cognitive impairment and hippocampal atrophy on MRI. His mild dementia slowly showed improvement to normal cognition over a period of 2.5 years. Further studies are needed to define the role of combination therapy in treating Alzheimer’s disease. |
|
|
|
|
|
Keywords :
|
Alzheimer Disease, Atrophy, Memory Disorders, Nicergoline, Nimodipine.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64d5100000000205000001001400 6go6ckt5b5idvals|666 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Alzheimer’s disease (AD), the most common cause of dementia in the elderly, currently affects about 8.2/1000 person-years in China [1]. Although AD has been intensively researched for many years, there are still limited treatments for it. Currently approved pharmacotherapy includes three cholinesterase inhibitors and one N-methyl D-aspartate receptor (NMDAR) antagonist. Although there are evidences prove that one of the cholinesterase inhibitor, donepezil, might slow down the hippocampus atrophy [ 2], those treatments are generally considered as symptom stabilizer [ 3- 5]. Previous studies showed that donepezil decreased an annualized rate of cognitive decline on MMSE in AD [ 6]. Here is a report of a 78-year-old and highly educated man with mild to moderate probable AD. He has been improved slowly by a combined therapy at cognitive function and global status over 2.5 years, from 21 scores on MMSE at his first visit to 28 scores on MMSE at final visit.
Case Report
The patient is an 77 year old mathematics teacher who was brought to our memory clinic in 2012 for consideration of gradual cognitive decline in two years’ time, especially short-term memory impairment (failing to remember foods eaten for breakfast), and difficulties with mathematical calculation (86 - 7=99), reading clock and judgment, slurred reaction, unstable mood, (impatience and irritability), language repetition, low comprehension and judgment, slowness of reaction, inability to use household appliances, significantly impaired shopping and money-management, slight difficulties in dressing, and needing instructions in eating and grooming.
His past medical history was suggestive of lower extremity weakness since developing acute cerebral hemorrhage prior to presentation. His past history was also suggestive of prostatectomy for benign hypertrophy of prostate. He had no history of drinking alcohol and smoking, and no obvious family history related to dementia. Upon general examination, no relevant sign was evident. Head turning sign was the only specific sign of neurologic examination with no evidence of extrapyramidal signs, involuntary movements or ataxia. Laboratory tests, like erythrocyte sedimentation rate, full blood count, electrolytes, calcium, renal and liver function tests; antinuclear factor, glucose, thyroid function, vitamin B12, folate, homocysteine, serology for syphilis, HIV, and hepatitis virus were all unremarkable. There was no abnormality in ECG or chest X-ray. Axial FLAIR showed multiple ischemic infarcts beside the lateral ventricles, frontal and parietal lobes, and mild white matter demyelination. Axial FLAIR showed the malacia on the right temporal lobe. Coronal FLAIR showed atrophy of the bilateral hippocampal volume, medial temporal lobe atrophy (MTA) scale=3, and global cortical atrophy (GCA) scale=2 [Fig.1].

His neuropsychological assessment at presentation revealed significant decrease in global cognition, delayed episodic memory, and calculation/attention; mild decrease of daily living activities, without obvious depression, anxiety, psychiatric and behavior symptoms. In detail, his Mini-Mental State Examination (MMSE) score was 21/30, Delayed Story Recall (DSR) was 4/56, Clock Drawing Test (CDT) was 4/4, Activity of Daily Living (ADL) was 17/56, Hamilton Depression Scale (HAMD) was 3/56, Hamilton Anxiety Scale (HAMA) was 1/56, Hachinski Inchemic Score (HIS) was 4/18, Clinical Dementia Rating score (CDR) was 1/3, Neuropsychiatric Inventory(NPI) was 0/144.
According to history, physical examination, neurological examination and investigations, especially neuropsychological assessment results and cranial MRI imaging (MTA 3/3, Fazekas scale 1.5/3), the case was diagnosed as moderate dementia, probable Alzheimer disease with mild cerebral vascular risk factor according to NINCDS-ADRDA criteria proposed in 1984 [ 7]. He was started on combined therapy of Donepezil tablets 5 mg once a day; Nicergoline tablets 10 mg thrice a day; and Nimodipine tablets 30 mg thrice a day) and TCM herbal therapy (prescribed herbal decoction covering herbs with functions of boosting kidney, and clearing phlegm every day). He got a continues improvement in cognition, especially episodic memory and an improvement in daily activities after two and half years’ combined therapy [Table 1].
His ISR increased from 14 to 19, DSR increased from 4 to 15, MMSE increased from 21 to 28, ADL deceased from 17 to 15, and CDR reduced from 1 to 0.5. CDT remained nearly the same.
Discussion
Although the patient had been in hospital for acute cerebral hemorrhage for three weeks prior to presentation and there are several small ischemic infarcts beside the lateral ventricles, frontal and parietal lobes, and mild white matter demyelination in his brain MRI, he was diagnosed as probable AD with mild vascular factor. There are several reasons. First, the patient was brought to our memory clinic for his insidious and progressive cognitive decline in two year time without fluctuating character. Second, he has more than two domains of cognitive impairment (memory loss and decreased calculation, comprehension, judgment and clumsy response). His CDR was more than 0.5 and ADL score is more than 16 (he cannot use household appliances and has slight difficulties in dressing, and need instructions in eating and grooming). Third, his brain MRI showed severe atrophy of the bilateral hippocampal volume, MTA scale=3, GCA=2 in coronal FLAIR image, and very mild white matter demyelination and small multiple ischemic infarct beside the lateral ventricles, frontal and parietal lobes. Thus, he was finally diagnosed as probable AD. Other diseases that cause cognitive impairment were excluded by the patient’s negative results of laboratory tests.
The good outcomes of receiving 2.5 year’s combined therapy after diagnosis was quite beyond the expected decline of MMSE changes according to historical data [ 8], which may partially explained by evidences from clinical trials or animal experiments of Donepezil [ 6] and our herbal formula, GAPT, a combination of eight herbal extracts with functions of boosting kidney, and clearing phlegm [ 9- 11]. It might also indicate the complex pathogenic process of AD should be treated with multiple targets medicine or combination of multiple therapies. Well-designed preclinical and clinical study are required to investigate the effects of combination therapy in treating Alzheimer’s disease.
Acknowledgments
Project on Absorption of Intellects by Institutions of Higher Education for Academic Disciplinary Innovations (the “111 Project”) (No.B08006), and The Technological Platform of Clinical Evaluation and Research for New Herbal Medicinal Products (2011ZX09302-006-01), and National Natural Science Foundation of China (No. 81473518, 81573824 and 81503625).
References
- Yuan J, Zhang Z, Wen H, Hong X, Hong Z, Qu Q, et al. Incidence of dementia and subtypes: A cohort study in four regions in China. Alzheimers Dement. 2016;12(3):262-271.
- Dubois B, Chupin M, Hampel H, Lista S, Cavedo E, Croisile B, et al. Donepezil decreases annual rate of hippocampal atrophy in suspected prodromal Alzheimer’s disease. Alzheimers Dement. 2015;11(9):1041-1049.
- Wilcock GK. Disease-modifying treatments for Alzheimer’s disease: A perspective based on experience with r-flurbiprofen. Alzheimer’s Dement. 2006;2(3):150-152.
- Gill SS, Anderson GM, Fischer HD, Bell CM, Li P, Normand SL, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med. 2009;169(9):867-873.
- Chalmers KA, Wilcock GK, Vinters HV. Cholinesterase inhibitors may increase phosphorylated tau in Alzheimer’s disease. Journal of Neurology. 2009;256(5):717-720.
- Winblad B1, Engedal K, Soininen H, et al. A 1-year, randomized, placebo-controlled study of donepezil in patients with mild to moderate AD. Neurology. 2001;57(3):489-495.
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939-944.
- Mendiondo MS, Ashford JW, Kryscio RJ, Schmitt FA. Modelling mini mental state examination changes in Alzheimer’s disease. Stat Med. 2000 Jun 15-30;19(11-12):1607-1616.
- Tian J, Shi J, Zhang X, Wang Y. Herbal therapy: a new pathway for the treatment of Alzheimer’s disease. Alzheimers Res Ther. 2010;2(5):30.
- Tian J, Shi J, Zhang L, Yin J, Hu Q, Xu Y, et al. GEPT extract reduces Abeta deposition by regulating the balance between production and degradation of Abeta in APPV717I transgenic mice. J. Curr Alzheimer Res. 2009;6(2): 118-131.
- Shi J, Tian J, Zhang X, Wei M, Yin L, Wang P, et al. A combination extract of ginseng, epimedium, polygala, and tuber curcumae increases synaptophysin expression in APPV717I transgenic mice. J. Chinese Medicine. 2012;7(1):13.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Zhang X, Shi J, Li T, Wei M, Ni J, Wang Y, Tian JCombination Therapy: Promising Rationale for Alzheimer’s Disease.JCR 2016;6:455-458 |
|
Zhang X, Shi J, Li T, Wei M, Ni J, Wang Y, Tian JCombination Therapy: Promising Rationale for Alzheimer’s Disease.JCR [serial online] 2016[cited 2025 Dec 14];6:455-458. Available from: http://www.casereports.in/articles/6/3/Combination-Therapy.html |

|
|
|
|
|