|
|
|
|
|
Hereditary Trichilemmal Cyst
|
|
|
Sandip Kumar Rahul1, Ghanshyam Sahu2, Susama Behera1, Satyabir Mohapatra3, Pallavi Suman4
Departments of 1Surgery, 2Pathology, 3Pediatrics, Nehru Shatabdi Central Hospital, Talcher, Angul, Odisha 759103; 4Central Hospital, Barajamda, West Singhbum, Jharkhand, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Sandip Kumar Rahul
Email: sandeep.rahul65@gmail.com
|
|
|
|
|
|
|
|
|
Received:
15-MAY-2016 |
Accepted:
14-JUL-2016 |
Published Online:
20-SEP-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Trichilemmal cysts over scalp commonly occur in sporadic form. Hereditary form is rare. A case of hereditary trichilemmal cyst with multiple cysts on scalp and calcification in the histopathological examination of the lesion is described. Importance of identifying the hereditary variety, its criteria and the need for histopathology are stressed upon. |
|
|
|
|
|
Keywords :
|
Calcification, Calcinosis, Epidermal Cyst, Scalp.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa47710000000ff04000001000700 6go6ckt5b5idvals|663 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Trichilemmal cysts (TC) affect 5% to 10% of the population with a female predominance and an autosomal dominant inheritance, if hereditary [ 1]. Its natural course is usually benign but occasionally there may be recurrences, excessive increase in the size and number of lesions and even malignant transformation. There are a few subtle points in the patient’s history and a few unique histopathological characteristics which can point towards a complicated course. A case is discussed to emphasize upon these salient features and their implication.
Case Report
A 47-year-old female presented to the outpatient’s clinic with complaints of multiple painless, progressively enlarging swellings over her scalp since last 4 years. No other symptoms were present. Patient’s mother had a history of similar scalp lesions before 45 years of age and later developed breast cancer. On examination, three non-tender, mobile, cystic lesions without any punctum and with well-defined margins were found over the scalp. These lesions measured 6x3 cm, 2x2 cm and 3x2 cm over the left parietal, right parietal and occipital scalp respectively [Fig.1]. Lymph nodes of the neck were not enlarged. Another cystic lesion with punctum was seen over back. Routine blood and urine examination were normal. Lesions over the scalp were excised under local lignocaine anesthesia. They had well defined capsules and could be easily separated from the surrounding structures. Histopathological examination (HPE) of the lesion revealed features consistent with TC with central calcification [Fig.2,3].
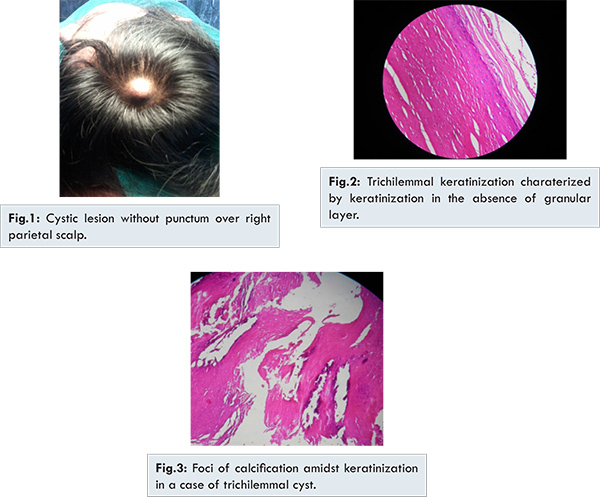
TC has been reported to be an important cause of cystic scalp lesion in middle aged and elderly females [ 2, 3]. It has been described as keratin filled cyst originating from the outer hair root sheath. It usually manifests as a benign, slowly growing, painless lesion, single or multiple in number, mostly located in regions having high hair density. Scalp is the affected site in more than 90% cases [ 2]. In a study of sebaceous cysts under electron microscope, McGavran and Binnington used the term ‘pilar cysts’ for cysts wherein keratinization occurred without keratohyaline granules, as in the cases of the cortex of hair and nail [ 4]. Pinkus used the term TC for these lesions [ 5]. Trichilemmal keratinization without granular layer is pathognomonic of TC and important in differentiating it from epidermoid cyst [ 6, 7].
Several investigators have reported the natural course of TC [ 8, 9]. Proliferating and malignant proliferating variety of TC, although rare, need to be diagnosed on histopathology as they attain large sizes, recur and metastasize when malignant [ 10]. This signifies the importance of HPE in every case of TC. TC cases are commonly sporadic and hereditary TC is rare. However, due to chances of multiple lesions, recurrences and risks of occurrence in other family members, it is important to identify hereditary TC.
Seidenari et al. proposed the clinical criteria for the identification of hereditary cases. This includes: (i) Diagnosis of TC in at least 2 first degree relative, or in 3 ‘first’ or ‘second’ degree relatives in 2 consecutive generations, (ii) TC diagnosed at less than 45 years of age in at least 1 family member, (iii) diagnosis of multiple cysts, giant cysts (greater than 5 cm), or cysts with rare HPE features, such as proliferation or ossification [ 9]. Eiberg et al. reported a Danish family in which 11 members had TC inherited in an autosomal dominant pattern [ 11]. The involved locus was suggested to be 3p24-p21.2 [ 11].
Identifying the hereditary variety of TC has important implications. A patient who has multiple lesions, giant lesions, a positive family history and lesions occurring at a younger age should be thought to have hereditary variant. Our patient had multiple lesions over scalp, largest among them exceeded 5 cm, and one first degree relative (mother) had a positive history before 45 years of age. All these features pointed towards hereditary form of TC in our patient. Calcification was found in HPE [Fig.3]. This has been reported to be seen in approximately 25% of the lesions [ 12]. Proliferating TC characterized by lobulation of the cyst wall with piling up of squamous epithelium have a tendency to transform into large lobulated scalp masses, occasionally with malignant degeneration. However, in our patient non-proliferating histology was reported.
Conclusion
Hereditary TC should be considered, keeping the family history, nature of the lesion and its clinical features in mind. Histopathology is indispensable in diagnosing proliferating, malignant proliferating and lesions with calcification. HPE should therefore be done in all cystic lesions of the scalp.
References
- Thomas VD, Snavely NR, Lee KK, Swanson NA. Benign epithelial tumors, hamartomas, and hyperplasias. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick’s Dermatology in General Medicine. 8th ed. McGraw-Hill: New York; 2012. pp. 1334.
- Al-Khateeb TH, Al-Masri NM, Al-Zoubi F. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg. 2009;67:52-57.
- Leung LK. Differential diagnosis of soft scalp lumps. BMJ Case Rep. 2011;2011.
- McGavran MH, Binnington B. Keratinous cysts of the skin. Identification and differentiation of pilar cysts from epidermal cysts. Arch Dermatol. 1966;94:499-508.
- Pinkus H. Sebaceous cysts are trichilemmal cysts. Arch Dermatol. 1969;99:544-555.
- Wick MR, Glembocki DJ, Teague MW, Patterson JW. Cutaneous tumors and tumor like conditions. In: Silverberg SG, editor. Silverberg’s Principles and Practice of Surgical Pathology and Cytopathology. 4th ed. Churchill Livingstone, Elsevier: Philadelphia; 2006: pp. 254-5.
- Tamer SS, Joesph DP, Seycora JT. Tumors of the epidermal appendages. In: Elder DE, editor. Lever’s Histopathology of the Skin, 10th ed. Lippincott Williams & Wikins: Philadelphia; 2009. pp. 866-67.
- Leppard BJ, Sanderson KV. The natural history of trichilemmal cysts. Br J Dermatol. 1976; 94:379-390.
- Seidenari S, Pellacani G, Nasti S, Tomasi A, Pastorino L, Ghiorzo P, et al. Hereditary trichilemmal cysts: a proposal for the assessment of diagnostic clinical criteria. Clin Genet. 2013;84:65-69.
- Ye J, Nappi O, Swanson PE, Patterson JW, Wick MR. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol. 2004;122:566-574.
- Eiberg H, Hansen L, Hansen C, Mohr J, Teglbjaerg PS, Kjaer KW. Mapping of hereditary trichilemmal cyst (TRICY1) to chromosome 3p24-p21.2 and exclusion of beta-CATENIN and MLH1. Am J Med Genet A. 2005;133:44-47.
- Elder D, Elenitsas R, Ragsdale B. Tumors of the epidermal appendages. In: Elder D, Elenitsas R, Jaworsky C, et al. eds. Lever’s histopathology of the skin. 8th ed. Lippincott-Raven: Philadelphia; 1997:749-99.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Rahul SK, Sahu G, Behera S, Mohapatra S, Suman PHereditary Trichilemmal Cyst.JCR 2016;6:441-443 |
|
Rahul SK, Sahu G, Behera S, Mohapatra S, Suman PHereditary Trichilemmal Cyst.JCR [serial online] 2016[cited 2026 Mar 5];6:441-443. Available from: http://www.casereports.in/articles/6/3/Hereditary-Trichilemmal-Cyst.html |

|
|
|
|
|