|
|
|
|
|
Medullary Sponge Kidney with Incomplete Renal Tubular Acidosis: A Poorly Understood Disease
|
|
|
generico cialis italia cialis generico
Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Sandeep Gupta
Email: drsandeepgupta2009@yahoo.in
|
|
|
|
|
|
|
|
|
Received:
18-MAR-2016 |
Accepted:
21-JUN-2016 |
Published Online:
30-SEP-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Medullary sponge kidney (MSK) is usually a benign process which may remain asymptomatic and undetected for life. Incomplete distal renal tubular acidosis (RTA) may be found in as many as 30% to 40% of these patients. Clinical presentation usually occurs after 20 years of age. It may present with renal colic, recurrent urinary tract infection (UTI) and gross hematuria. We are presenting a case of 30 year old female who presented with recurrent urinary tract infection, underwent multiple surgeries for renal stone and due to insufficient follow up developed complications related to forgotten ureteric stent. She finally landed up as poorly functioning symptomatic right kidney and non-functioning left kidney for which nephrectomy was done. This case highlights the importance of earlier diagnosis, proper management and frequent follow up to preserve renal function in a case of MSK.
|
|
|
|
|
|
Keywords :
|
Hematuria, Kidney Calculi, Medullary Sponge Kidney, Renal Colic, Stents.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa4f410000000f404000001000800 6go6ckt5b5idvals|667 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Medullary sponge kidney was recognized by Beitzke in 1908 and radiographic features were described by Lenarduzzi in 1939 [1]. MSK occurring due to disruption at the ureteric bud and metanephric mesenchyme interface supports genetic basis [1,2]. Tubular defects may coexist in this disease due to this disruption; the most important one is distal tubular acidification defect. The frequency of medullary sponge kidney is one case per 5000 general population, and the prevalence may be as much as 1 case per 1000 population in urology clinics. In addition, medullary sponge kidney has been identified in 12-20% of patients who form calcium stones [3]. The first sign of medullary sponge kidney is usually a UTI or a kidney stone. When it presents along with tubular acidification defect, it is diagnosed on the basis of clinical history, biochemical examination of blood and urine and imaging studies. There is no way at present to prevent or reverse MSK, so the management is mainly based on treating UTI and removing kidney stones. In patients with hypo-citraturia and incomplete distal RTA, treatment with potassium citrate helps prevent the formation of new kidney stones. In our case, MSK was associated with tubular acidification defect that lead to recurrent UTI, multiple calculi in bilateral kidneys and ureter leading to chronic kidney disease and renal failure.
Case Report
A 30 years old female presented to us with bilateral flank pain, recurrent UTI, fever and vomiting. She had history of multiple bilateral stone surgeries. Two years back left ureteroscopic stone removal was done and ureteric stent placed. She was lost to follow up and presented to us with above mentioned complaints. General physical examination revealed a malnourished status. Left renal angle was tender without any palpable lump.
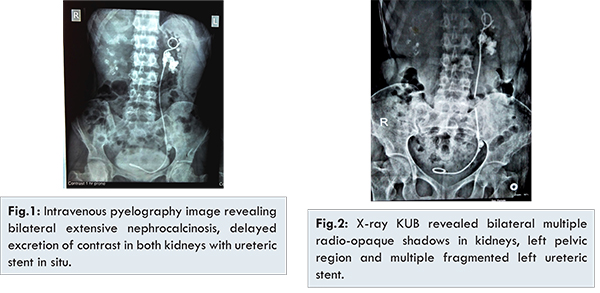
She had IVU (intravenous urogram) films that revealed bilateral extensive nephrocalcinosis, multiple left ureteric calculi, delayed excretion of contrast in both kidneys with ureteric stent in left side [Fig.1]. Screening ultrasonography findings were bilateral medullary nephrocalcinosis with multiple renal calculi in both kidneys along with multiple calculi in left lower ureter and ureteric stent in situ. She was thoroughly investigated. Her creatinine was 2.4 mg/dL at admission. Her serum calcium and parathormone levels were within normal limits. Urinary examination revealed pH: 7.45, proteins ++, plenty of pus cells and red blood cells. Furosemide, fludricortisone test and ammonium chloride loading test revealed inability to decrease urine pH below 5.5 consistent with diagnosis of incomplete RTA. X-ray kidney-ureter-bladder (KUB) showed bilateral multiple radio-opaque shadows in kidneys, left pelvic region and multiple fragmented left ureteric stent [Fig.2]. DTPA (diethylenetriamine pentaacetic acid) renal scan was done which showed poor functioning bilateral kidneys with GFR (glomerular filtration rate) of right kidney 31 ml/min and left kidney 12 ml/min. She was planned for surgery and explained about requirement of nephrectomy in future, if kidney functions fail to improve. With the help of flexible ureteroscope all three fragments of ureteric stent along with the ureteric calculi were removed and repeat ureteric stenting was done. She was followed up regularly, her creatinine level was 1.2 mg/dL post-operatively. A repeat DTPA renal scan was done 6 months post-surgery, which revealed right kidney GFR: 29.10 ml/min and no significant cortical built up of radiotracer in left kidney. She remained symptomatic with no discernible left kidney function so left laparoscopic simple nephrectomy was done. Gross specimen showed multiple, small cysts in medullary pyramids and papillae. Histopathological analysis demonstrated multiple small medullary cysts lined by cuboidal epithelium with concretions adhered to cyst wall consistent with findings in medullary sponge kidney. At discharge she was explained regarding her CKD (chronic kidney disease) status and need for renal transplantation in future.
Medullary sponge kidney is characterized by tubular dilatation of the distal collecting ducts with numerous associated cysts and diverticula which are confined to the medullary pyramids. It is usually a benign process that may remain asymptomatic and undetected for life. Clinical presentation usually occurs after age of 20 years, with the most common presentation being renal colic (50% to 60%), urinary tract infection (20% to 33%) and gross haematuria (10% to 18%) [4]. Among people who are more likely to develop calcium-based kidney stones, women are more likely than men to have medullary sponge kidney [5]. The incidence of MSK in stone-formers differs widely in the reported series. Stagnant flow as a result of the dilated collecting duct, and particularly the static conditions in the fluid filled blind ended cysts, are the reason those innumerable tiny stones form which end up packing the ‘sponges’ with masses of crystals. This stagnant flow in dilated intramedullary collecting duct and particularly in cysts, predisposes to infection. In addition to such anatomic abnormalities, low levels of urinary inhibitors of stones seem to contribute to the pathogenesis of nephrolithiasis in patients with MSK [3]. MSK patients have defects in urinary acidification and concentration mechanism which may, in part, be the result of functional abnormality of the terminal collecting ducts [6]. Incomplete distal renal tubular acidosis may be found in as many as 30% to 40% of these patients [5]. Incomplete RTA represents less serious clinical pattern. Up to 70% of adults with distal RTA have kidney stones. Incomplete variant of the disease shows less marked hypocitraturia and normal urine acidity. Diagnosis of incomplete variant was made with the use of an ammonium chloride loading challenge [7,8].
The significance of nephrolithiasis and the mechanisms by which it occurs are not properly understood. Many patients with MSK have no evidence of nephrolithiasis. Among those who do, recurrence is common, and metabolic profile and composition are varied as in the general stone forming population [9]. IVU is the gold standard for the diagnosis of MSK, but as the technique is used less and less, there is a concrete possibility of this renal condition being forgotten in the future. In general, intravenous urography is more sensitive than computed tomography in detecting mild cases of medullary sponge kidney. Although the pathogenesis of MSK has yet to be elucidated, its association with different malformations which supports the idea that it is a developmental disorder. Recent findings suggest that MSK may be the consequence of a disruption of the ureteral-bud and metanephric blastema interface [1,2]. MSK is a disease that deserves more attention and research efforts to help clarify its etiology and optimize treatment strategies. Metabolic evaluations and attempts at stone prevention are most critical in patients suffering from MSK. In such patients the clinical history is especially important as visualizing new stones in the setting of extensive nephrocalcinosis can be quite challenging. That being said, realistic surgical goals should be established. Clearing all stones from such kidneys is rarely feasible, though unroofing the pockets that are closest to the collecting system or large on CT imaging offers a good place to start. Treatment with potassium citrate is effective in preventing renal stones in the typical patient with MSK [10].
Conclusion
MSK is a rare, complex and poorly understood disease that can manifest uniquely from patient to patient. When it is associated with renal tubular acidosis, patient presents with recurrent UTI and renal stones. Early diagnosis, proper management and frequent follow up are very important to preserve kidney functions.
References
- Gambaro G, Feltrin GP, Lupo A. Medullary sponge kidney (Lenarduzzi-Cacchi-Ricci disease): a Padua Medical School discovery in the 1930s. Kidney Int. 2006;69(4):663-665.
- Gedroyk WM, Saxton HM. More medullary sponge variants. Clin Radiol.1988;39(4):423-425.
- Yagisawa T, Kobayashi C, Hayashi T. Contributory metabolic factors in the development of nephrolithiasis in patients with medullary sponge kidney. Am J Kidney Dis. 2001;37(6):1140-1143.
- Kuiper JJ. Medullary sponge kidney. Perspect Nephrol Hypertens. 1976;4:151-71.
- Torres VE, Grantham JJ. Cystic diseases of the kidney. In: Brenner BM, editor. Brenner and Rector’s the kidney. 8th ed. Philadelphia: Saunders; 2008. p. 1428-1462.
- Higashihara E, Nutahara K, Tago K. Medullary sponge kidney and renal acidification defect. Kidney Int. 1984;25(2):453-459.
- Arampatzis S, Röpke-Rieben B, Lippuner K, Hess B. Prevalence and densitometric characteristics of incomplete distal renal tubular acidosis in men with recurrent calcium nephrolithiasis. Urol Res. 2012;40(1):53-59.
- Tannen RL, Falls WF Jr, Brackett NC Jr. Incomplete renal tubular acidosis: some clinical and physiological features. Nephron. 1975;15:111-123.
- McPhail EF, Gettman MT, Patterson DE, Rangel LJ, Krambeck AE. Nephrolithiasis in Medullary Sponge Kidney: Evaluation of Clinical and Metabolic Features. Urology. 2012;79(2):277-281.
- Fabris A, Lupo A, Bernich P. Long-term treatment with potassium citrate and renal stones in medullary sponge kidney. Clin J Am Soc Nephrol. 2010;5(9):1663-1668.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Gupta S, Jain P, Chandra V, Pal DKMedullary Sponge Kidney with Incomplete Renal Tubular Acidosis: A Poorly Understood Disease.JCR 2016;6:459-462 |
|
Gupta S, Jain P, Chandra V, Pal DKMedullary Sponge Kidney with Incomplete Renal Tubular Acidosis: A Poorly Understood Disease.JCR [serial online] 2016[cited 2025 Dec 25];6:459-462. Available from: http://www.casereports.in/articles/6/3/Medullary-Sponge-Kidney-with-Incomplete-Renal-Tubular-Acidosis.html |

|
|
|
|
|