|
|
|
|
|
Multiple Abscesses in Thigh due to Klebsiella in a Diabetic Patient with Rheumatoid Arthritis
|
|
|
Robin George Manappallil1, Suhaib Rehaman2, Subhash KR3
Department of Medicine1, Surgery2 and Orthopaedics3; National Hospital, Calicut, Kerala 673001, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Robin George Manappallil
Email: drrobingeorgempl@gmail.com
|
|
|
|
|
|
|
|
|
Received:
04-MAR-2016 |
Accepted:
28-JUN-2016 |
Published Online:
30-AUG-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Klebsiella, a gram negative bacteria, can cause a variety of clinical syndromes in human beings. These include pneumonia, urinary tract infection, abdominal infection, surgical site infection, soft tissue infection and infections of intravascular devices. Middle-aged and elderly individuals with chronic debilitating diseases like diabetes, alcoholism, and immunocompromised persons are more susceptible to Klebsiella infections. This case report is regarding a diabetic patient, on treatment for rheumatoid arthritis, who developed cellulitis of leg with multiple thigh abscesses due to Klebsiella, which happens to be a rare presentation. |
|
|
|
|
|
Keywords :
|
Cellulitis, Diabetes Mellitus, Klebsiella, Rheumatoid Arthritis, Thigh.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa8fa0f000000f204000001000f00 6go6ckt5b5idvals|655 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Klebsiella organisms cause a wide range of clinical syndromes, which can lead to bacteremia. Diabetic and immunocompromised persons are more prone to these infections. Pneumonia, urinary tract infection and hepatic abscess account for 15-30% of Klebsiella bacteremia. 5-10% are due to infections of intravascular devices, while the remaining is seen as surgical site infections or as miscellaneous infections [1]. Cellulitis, an acute inflammation of the skin, is commonly caused by Staphylococcus aureus, Streptococcus pyogenes and Pseudomonas aeruginosa. Bacteria gain access to the epidermal layers via cracks in the skin, burns, insect bites, surgical incisions and catheter lines. Clinically, the patients can present with localized pain, erythema, swelling, hot skin and fever. These organisms can also cause pyomyositis and myonecrosis [2].
This case report highlights the presentation of a diabetic patient, who is also on treatment for rheumatoid arthritis, with multiple abscesses in thigh. Moreover, Klebsiella being the causative organism of the abscess is a rare scenario.
Case Report
Our patient is a 45 year old male, farmer by occupation, married and has 2 children, who presented to the Emergency department with complaints of high grade fever and right lower limb swelling and tenderness. He is a diabetic, on glimepiride and metformin, for past 3 years. About 1 year ago, he was diagnosed to have rheumatoid arthritis and is on leflunomide and hydroxychloroquine, as advised by his rheumatologist. He has also been taking short courses of deflazacort during arthritic pain exacerbations.
Detailed history revealed that the patient has been symptomatic for the past 7 days. His initial symptom was mild pain in the right thigh, which he noticed after returning from work in the fields. There was no redness or swelling or local rise in temperature, history of trauma or bite marks. He applied diclofenac gel, following which there was relief of pain. The following day, pain started increasing in the right thigh and he took diclofenac tablets, as over the counter medication. However, there was no relief and he developed redness, swelling and severe tenderness of the thigh. He also noticed that the skin over the entire right thigh was hot. During this period, he also developed low grade fever. For the above complaints, he visited a local hospital, where he was diagnosed to have sepsis due to cellulitis. He was started on intravenous antibiotics (cefoperazone + sulbactam). Since there was no improvement in his condition, he was referred to higher centre for further management.
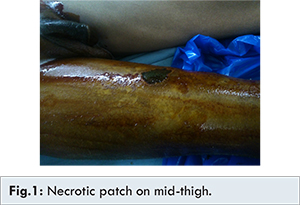
On examination, he was conscious and oriented. He was febrile with temperature of 1010F. His heart rate was 100 beats/ minute which was regular, blood pressure of 100/70 mmHg with no postural drop, respiratory rate of 20/minute with 96% oxygen saturation in room air. Local examination revealed swelling of the entire right lower limb with swelling of the right knee joint. The skin over the right lower limb was red, tender and hot. A 3x4 cm necrotic patch was present on mid-thigh which was formed after a blister rupture [Fig.1]. He had bilateral fine basal crepitations on respiratory system examination. Other systemic examinations were normal.
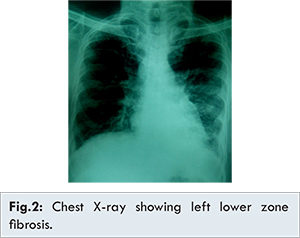
On the basis of his history and examination, a provisional diagnosis of sepsis due to right lower limb cellulitis, diabetes, rheumatoid arthritis and interstitial lung disease (as a part of rheumatoid arthritis) was made. Initial laboratory investigations showed anaemia (Hb 7.6 g/dL) with elevated leucocyte count (18,000 cells/cmm) and mild thrombocytopenia (1,20,000 cells/cmm). Peripheral smear showed microcytic hypochromic red cells. His renal function tests, electrolytes, calcium, liver function tests, aPTT and prothrombin time were normal. His total cholesterol was 227 mg/dL and random blood glucose was 250 mg/dL. Urinary ketones were negative and urine microscopy was normal. Chest X-ray showed lower zone fibrosis mainly on the left side [Fig.2] and computed tomography of chest was suggestive of interstitial lung disease (usual interstitial pneumonia pattern). ECG and ultrasound abdomen were normal. Blood culture was sterile. Serology for melioidosis was negative. Mantoux test also turned out to be negative.
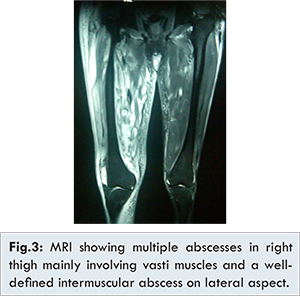
He was started on intravenous piperacillin + tazobactam and linezolid. Sugar levels were controlled with regular and NPH insulin. He was asymptomatic with regard to his interstitial lung disease. X-ray of right knee (anteroposterior and lateral views) were normal. Right knee joint aspiration was done and synovial fluid report was suggestive of septic arthritis, with Klebsiella organism on culture. By day 3 of admission, his total counts and platelets started normalizing, and lower limb oedema below the knee almost completely resolved. Even after 5 days of antibiotic treatment, his right thigh failed to show any improvement with regard to oedema. Ultrasound of right thigh showed large localized collection in the lateral compartment of proximal and mid-thigh. Magnetic resonance imaging of bilateral lower limbs showed multiple abscesses in the right thigh mainly involving the vasti muscles [Fig.3].
Surgical and orthopaedic consultations were taken and incision and drainage with extensive wound debridement of anterior compartment was done, with incision extending from the right inguinal region up to right knee joint. The necrotic patches of muscle were excised [Fig.4]. Two units of packed cell transfusions were given. Pus culture grew Klebsiella and Candida, and was negative for acid fast bacilli. As per pus culture and sensitivity reports, linezolid was stopped, and piperacillin + tazobactam was continued with addition of amikacin and fluconazole. Muscle biopsy was consistent with myonecrosis. Vacuum dressing was done for a few days. Following the formation of granulation tissue, the wound was closed with nylon suture and drain was placed. Three days later, the drain was removed, after complete cessation of discharge, and on day 15, he was discharged. Alternate day dressing was advised, with review of wound after 8 days and suture removal after 12 days.
Discussion
Klebsiella pneumonia, a gram negative bacilli, is one of the most important organism causing community acquired and nosocomial infections. These include pneumonia, urinary tract infection, abdominal infection, soft tissue infection and infection of surgical sites and intravascular devices [1]. The incidence of Klebsiella infections is higher in diabetic patients [2-4]. The commonly reported infections in patients with rheumatoid arthritis are abscess (limb, perinephric, subdural, ovarian, cerebral, lung), pneumonia, empyema and pyelonephritis [5]. Increased incidence of faecal Klebsiella pneumonia has been reported in patients with rheumatoid arthritis [6].
An abscess can occur anywhere in the body and presents with clinical features of acute inflammation. The abscess formation is usually preceded by a puncture wound or a surgery or can even be metastatic following bacteremia [7]. Klebsiella organisms cause soft tissue infection by gaining access either directly from trauma of the affected site or, by hematogenous spread from other septic foci. Abscess formation is an uncommon presentation of Klebsiella. However, it has been an emerging pathogen in pyogenic liver abscess [8]. There have also been reports of spinal epidural, brain and renal abscess due to Klebsiella [9-11]. Psoas abscess have been reported in diabetic patients [12]. Septic arthritis has also been observed with Klebsiella [13]. A few cases of necrotizing fasciitis have been reported with Klebsiella. They were associated with other septic foci, commonly liver abscesses, urinary tract infections and endogenous endophthalmitis. Therefore, it is always essential to look for other foci of infection in case of Klebsiella associated soft tissue infections [14-16]. Due to increasing emergence of resistance, treatment of these infections have become challenging, often requiring a combination therapy [1].
Ultrasonography, computerised tomography and magnetic resonance imaging are useful in the diagnosis; and can also aid in guided aspiration of the pus. Surgical decompression and curettage of the abscess remains as the main stay of treatment. The role of antibiotics is controversial, unless there is evidence of spreading infection in the form of cellulitis or sepsis. Delayed primary or secondary suturing following the formation of mature granulation tissue is the safest method of wound closure [7].
In this case, the patient is a diabetic and has rheumatoid arthritis, and has been on intermittent course of steroids. However, during this episode he was off steroids. The initial event would have been cellulitis, followed by septic arthritis. Due to the emergence of resistant strains of Klebsiella, the use of cephalosporins was insufficient to tackle the infection, leading to the formation of abscess. Such an event of multiple thigh abscesses by Klebsiella, starting from cellulitis has not been reported yet.
Conclusion
Though Klebsiella is one of the etiological agents of soft tissue and muscle infections, especially in diabetics and immunocompromised patients, its presentation as multiple abscesses has rarely been reported. This case report also emphasises the need for combination therapy as well as the use of broad spectrum antibiotics for Klebsiella infections, due to emergence of resistant strains.
References
- Thomas AR, James RJ. Diseases caused by gram-negative enteric bacilli. In: Kasper, Fauci, Hauser, Longo, Jameson, Loscalzo (ed). Harrison’s Principles of Internal Medicine. 19th ed. Mc Graw Hill education. pp. 1031-1033.
- Chang CM, Lee HC, Lee NY, Lee IW, Wu CJ, Chen PL, et al. Community-acquired Klebsiella pneumoniae complicated skin and soft-tissue infections of extremities: emphasis on cirrhotic patients and gas formation. Infection. 2008; 36:328-334.
- Chou H, Teo HE, Dubey N, Peh WC. Tropical pyomyositis and necrotizing fasciitis. Semin Musculoskelet Radiol. 2011;15:489-505.
- Lye WC, Chan RK, Lee EJ, Kumarasinghe G. Urinary tract infections in patients with diabetes mellitus. J Infect. 1992;24(2):169-174.
- Huskisson EC, Hart DF. Severe, unusual, and recurrent infections in rheumatoid arthritis. Ann Rheum Dis. 1972;31:118.
- Ebringer R, Colthorpe D, Young A, Corbett M. Increased incidence of faecal Klebsiella pneumoniae in patients with HLA B7, CREG antigen and men with rheumatoid arthritis. Br Med J. 1980;281(6240):583-585.
- William NS, Bulstrode CJK, O’Connell PR, editors. In: Williams NS, Bulstrode CJK, O’Connell PR, editors. Bailey and Love’s Short Practice of Surgery. 25th ed. London (UK): Hodder Arnold; 2008.
- Basu S. Klebsiella pneumoniae: An Emerging Pathogen of Pyogenic Liver Abscess. Oman Medical Journal. 2009;24(2):131-133.
- Kangwanprasert M, Young RS. Case report: spinal epidural abscess from Klebsiella pneumoniae. Hawaii Med J. 2005;64(8):216-217.
- Cho KT, Park BJ. Gas-Forming Brain Abscess Caused by Klebsiella Pneumoniae. Journal of Korean Neurosurgical Society. 2008;44(6):382-384.
- Chang SW, Yen DH, Fung CP, Liu CY, Chen KK, Tiu CM, et al. Klebsiella pneumoniae renal abscess. Zhonghua Yi Xue Za Zhi (Taipei). 2000;63(10):721-728.
- Chang CM, Ko WC, Lee HC, Chen YM, Chuang YC. Klebsiella pneumoniae psoas abscess: predominance in diabetic patients and grave prognosis in gas-forming cases. J Microbiol Immunol Infect. 2001;34(3):201-206.
- Pop C, Calagiu D, Jantea P, Nemes R. Septic knee arthritis in Crohn’s disease biological therapy-free patient: Case report. J Med Life. 2015;8(4):492-495.
- Hu BS, Lau YJ, Shi ZY, Lin YH. Necrotizing fasciitis associated with Klebsiella pneumoniae liver abscess. Clin Infect Dis. 1999;29:1360-1361.
- Dylewski JS, Dylewski I. Necrotizing fasciitis with Klebsiella liver abscess. Clin Infect Dis. 1998;27:1561-1562.
- Ho PL, Tang WM, Yuen KY. Klebsiella pneumonia necrotizing fasciitis associated with diabetes and liver cirrhosis. Clin Infect Dis. 2000;30:989-990.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Manappallil RG, Rehaman S, KR SubhashMultiple Abscesses in Thigh due to Klebsiella in a Diabetic Patient with Rheumatoid Arthritis.JCR 2016;6:406-410 |
|
Manappallil RG, Rehaman S, KR SubhashMultiple Abscesses in Thigh due to Klebsiella in a Diabetic Patient with Rheumatoid Arthritis.JCR [serial online] 2016[cited 2026 Jan 17];6:406-410. Available from: http://www.casereports.in/articles/6/3/Multiple-Abscesses-in-Thigh-due-to-Klebsiella-in-a-Diabetic-Patient-with-Rheumatoid-Arthritis.html |

|
|
|
|
|