Introduction
Sclerosing angiomatoid nodular transformation (SANT) is a benign non-neoplastic vascular splenic lesion. Consisting of multiple angiomatoid nodules surrounded by dense fibrous tissue, it was initially described by Martel et al. in 2004 [
1]. Several authors have shown characteristic imaging features of SANT: a T2-shortening mass on MRI [
2] and peripheral enhancing radiating lines and progressive enhancement in the arterial or portal venous phase [
3]. Calcification is rarely seen radiologically [
2] and is rarely mentioned as a characteristic image finding of SANT [
4]. Splenic hemangiomas, one of the most common vascular splenic lesions, sometimes show calcifications within the lesion [
5], whereas in SANT, there have been only a small number of such cases reported [
6]. Herein we report a case of SANT that showed scattered punctate foci of calcification on imaging and describe their significance.
Case Report
A 50-year-old woman was admitted to our hospital for investigation of a splenic mass incidentally detected on CT while investigating a large ovarian tumor. The ovarian lesion was diagnosed as a mucinous cystadenoma by bilateral salpingo-oophorectomy. She had neither abdominal symptoms nor signs on physical examination. She had no history of malignancy. Laboratory tests showed no inflammatory reaction, and tumor markers of CEA and CA 19-9 were within normal limits.
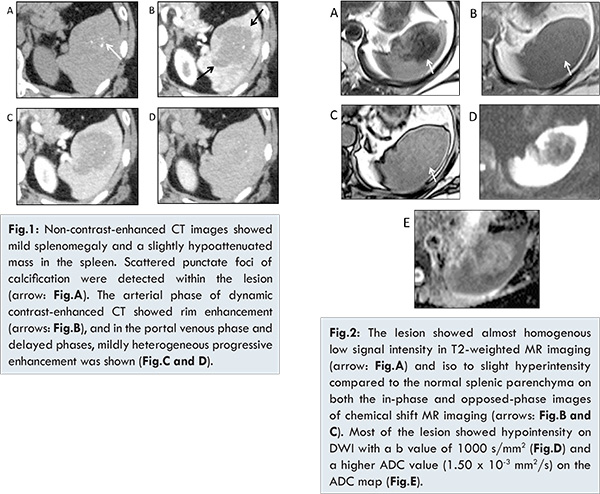
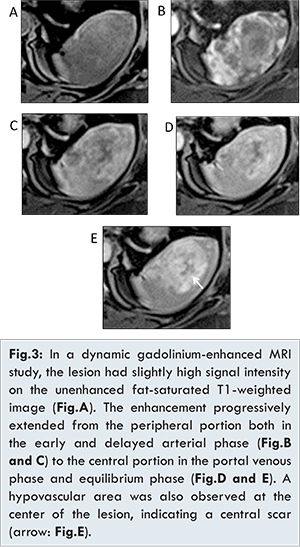
Non-contrast-enhanced CT revealed moderate splenomegaly and asplenic mass approximately 60 mm in diameter [Fig.1A]. The lesion was irregular and ill-defined, showing iso to mild hypoattenuation in relation to the normal splenic parenchyma. Scattered punctate foci of calcification were illustrated within the lesion, although there was no calcification in the surrounding splenic parenchyma. No lymphadenopathy was detected. The arterial phase of dynamic contrast-enhanced CT showed rim enhancement [Fig.1B]. In the portal and delayed phases, mildly heterogeneous progressive enhancement was observed [Figs.1C,1D]. On T2-weighted MR imaging, the lesion showed diffuse low signal intensity [Fig.2A]. Chemical shift imaging showed almost homogenous iso to slightly high signal intensity in relation to the normal splenic parenchyma both on in-phase and opposed-phase MR images [Figs.2B,2C]. Diffusion-weighted MR imaging with a b value of 1000 s/mm2 showed hypointensity throughout most of the mass with high apparent diffusion coefficient (ADC) values [Figs.2D,2E]. On dynamic gadolinium-enhanced MRI, the mass appeared slightly hyperintense on an unenhanced fat-saturated T1-weighted image [Fig.3A], and in the dynamic study the lesion showed peripheral enhancement in the early and delayed arterial phase [Figs.3B,3C] with the enhancement extending centrally in the portal and delayed phase [Figs.3D,3E]. There was a poorly enhanced area at the center of the lesion.
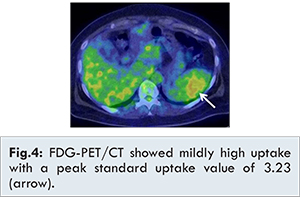
18F-FDG-PET/CT additionally performed showed mildly increased uptake of FDG with a peak standard uptake value of 3.23 at the lesion [Fig.4]. Multimodal imaging demonstrated that the lesion was probably benign, mainly according to the characteristic MR findings observed in the dynamic enhancement pattern and T2WI and DWI. Finally, hand-assisted laparoscopic splenectomy was performed, because the splenic malignancy could not be excluded.
In the resected gross specimen, the lesion was a 6-cm whitish mass. Multiple lobular reddish brown nodules were contained within the thick whitish fibrous tissues of the lesion [Fig.5A]. No invasion beyond the splenic capsule was identified. Microscopically, there were nodular proliferations of small vessels with abundant red blood cells and a partial deposit of hemosiderin [Fig.5B]. Immunohistochemical staining demonstrated that the vascular nodules consisted of three types of vessels: capillaries (indicating the expression of CD34+/CD8-/CD31+), small veins (CD34-/CD8-/CD31+) and sinusoids (CD34-/CD8+/CD31+). The angiomatoid nodules were separated by fibrous stroma with hyalinization and proliferation of myofibroblasts. Plasma cells and other inflammatory cells were scattered within the stroma. Some small foci of calcification were identified in the part of the lesion with hyalinization. These pathological findings were compatible with SANT seen in the spleen.
Discussion
SANT is a benign vascular splenic lesion thought to arise from a response of the red pulp to underlying stromal inflammation or vascular injury [4]. It consists of multiple angiomatoid nodules surrounded by dense fibrous tissue. The angiomatoid nodules include three types of vessels: capillaries (CD34+/CD8-/CD31+), small veins (CD34-/CD8-/CD31+), and sinusoids (CD34-/CD8+/CD31+) [1]. It has been reported that SANT is a female-predominant disease, affecting adults in the fourth to seventh decades of life [
8]. SANT is typically asymptomatic [
4], but can in rare cases cause abdominal pain, splenomegaly, or anemia [
3].
As imaging features, SANT shows iso to mild hypoattenuation on non-contrast-enhanced CT. It shows homogenous iso-intensity on T1-weighted MR imaging and heterogeneous hypointensity on T2-weighted MR imaging; the low signal intensity can be explained by the fibrous component and hemosiderin deposition. Low signal intensity is also described on chemical-shift imaging, with the decrease in signal intensity on the in-phase image compared with the opposed-phase image corresponding to the role of hemosiderin [
7]. In our case, the fibrous stroma accounted for a large part of the lesion compared with angiomatoid nodules while a few hemosiderin deposits were detected. In this case, the low signal intensity on T2-weighted image was considered to be mainly due to the fibrous component.
There have been a few reports describing the findings of DWI and the ADC map in SANT. Jang et al. [
9] described a case of SANT which showed low signal intensity on DWI and high ADC values as well as other various benign splenic lesions. On the contrary, Yoshimura et al. [
10] reported two cases of SANT which demonstrated multinodular high-intensity areas on DWI. As for the radiological-pathological correlations, these papers suggest that high-signal-intensity areas corresponded to angiomatoid nodules and peripheral low-signal-intensity areas corresponded to fibrous tissues [
10]. On the other hand, in our case, the detailed radiological-pathological correlation was not defined.
As to the enhancement patterns on dynamic contrast-enhanced study on CT/MRI, SANT usually demonstrates progressive or persistent enhancement; however, several enhancement patterns such as the spoke-and-wheel pattern, rim enhancement, a peripheral enhancing radiating line and central scar have also been reported [
3]. These enhancement patterns are considered to depend on the extent and distribution of angiomatous and fibrous components. In this case, early peripheral and delayed progressive central enhancements were also demonstrated. The hypovascular area in the center of the lesion was suspected to reflect a central scar although the scar was ill-defined in the resected specimen because of the diffusely distributed fibrous parenchyma.
The extent of FDG uptake on 18F-FDG-PET/CT in previous literature has varied, and the avidity of FDG was considered to depend on the number of macrophages, plasma cells, and myofibroblasts [
7]. In our case, there were small numbers of inflammatory cells, but a proliferation of myofibroblasts throughout the stroma, which seemed to account for the abnormal uptake of FDG. The peak value of SUV was almost similar to that in a previous report [
7], suggesting that peak SUV may contribute to differentiating SANT from malignant splenic lesions such as splenic malignant lymphoma and metastatic splenic tumor which have higher SUV peaks [
11].
To the best of our knowledge, there have been no case reports of SANT describing malignant transformation. Falk et al. [
8] reported there was no sensitive and specific way to make a diagnosis of SANT without obtaining a tissue sample, and it was prudent to operate even if SANT was suspected. Meanwhile, with the characteristic imaging findings for SANT as written above and without any suggestive findings for malignancy such as evidence of metastases, the appropriate options for a splenic lesion are either performing image-guided biopsy for a pathological diagnosis or watchful waiting. Gutzeit A et al. [
12] showed a case of SANT diagnosed by means of ultrasound-guided core needle biopsy without complications. Recent studies demonstrated lower complication rates in image-guided splenic biopsy [
13]. On the other hand, it should be noted that some cases of SANT can gradually increase in size during the follow-up period, despite its benign etiology [
10].
In general, as the differential diagnoses of splenic lesions that can contain calcifications, the standard nominees are hemangioma, malignant lymphoma, metastasis from mucinous adenocarcinoma, lymphangioma, inflammatory pseudotumor pseudocyst, and hamartoma [
14,
15]. Many authors have demonstrated that splenic hemangiomas, the most common vascular splenic lesion, sometimes show calcification. Calcifications can be present in firm fibrotic areas of the hemangioma or in the surrounding intratumoral cystic area in splenic hemangioma. On imaging, curvilinear or eggshell calcification is most often seen in cystic hemangioma while mottled central calcification is often seen in solid splenic hemangioma. Coarse calcification tends to occur in areas of necrosis or long-standing thrombosis [
5].
Pathologically, foci of calcification can sometimes be accompanied by large nodular or diffuse areas of hyalinization in SANT [
1]. In our case, the foci of calcification corresponded with the parts histologically identified with hyalinization. Yet most of imaging case reports have not described calcification as a characteristic image finding for SANT [2,4]. Radiologically, there have been only a small number of reported cases [
3,
6], and all of these cases showed punctate foci of calcification. In our case punctate calcifications scattered diffusely within the lesion were detected by CT, suggesting that this finding is unusual for SANT but not inconsiderable. Like splenic hemangioma, old hemorrhage and thrombosis can be also considered as causes of calcifications in SANT. SANT shows a punctate or mottled pattern of calcification, which may be defined as characteristic, as these patterns was seen in both previously reported cases and our case. When we see a case of SANT that shows diffuse, low signal intensity on T2-weighted MR imaging as in our case, intralesional calcifications within the prominent fibrous components may be detected on imaging.
In summary, SANT should be added to the lists of differential diagnoses of splenic tumors that show intralesional calcifications. It should be kept in mind that a punctate or mottled pattern of calcification within the prominent fibrous components, regions of hyalinization, or old hemorrhage may suggest a diagnosis of SANT.
References
- Martel M, Cheuk W, Lombardi L, Lifschitz-Mercer B, Chan JK, Rosai J. Sclerosing angiomatoid nodular transformation of the spleen (SANT): report of 25 cases of a distinctive splenic lesion. Am J Surg Pathol. 2004;28:1268-1279.
- Raman SP, Singhi A, Horton KM, Hruban RH, Fishman EK. Sclerosing angiomatoid nodular transformation of the spleen (SANT): multimodality imaging appearance of five cases with radiology-pathology correlation. Abdom Imaging. 2013;38:827-834.
- Lewis RB, Lattin GE, Nandedkar M, Aguilera NS. Sclerosingangiomatoid nodular transformation of the spleen: CT and MRI features with pathologic correlation. Am J Roentgenol. 2013;200:W353-360.
- Thipphavong S, Duigenan S, Schindera ST, Gee MS, Philips S. Nonneoplastic, benign, and malignant splenic diseases: cross-sectional imaging findings and rare disease entities. Am J Roentgenol. 2014;203:315-322.
- Abbott RM, Levy AD, Aguilera NS, Gorospe L, Thompson WM. From the archives of the AFIP primary vascular neoplasms of the spleen: radiologic-pathologic correlation. Radiographics. 2004;24:1137-1163.
- Li L, Fisher DA, Stanek AE. Sclerosing angiomatoid nodular transformation (SANT) of the spleen: addition of a case with focal CD68 staining and distinctive CT features. Am J Surg Pathol. 2005;29:839-841.
- Thacker C, Korn R, Millstine J, Harvin H, Van LierRibbink JA, et al. Sclerosing angiomatoid nodular transformation of the spleen: CT, MR, PET, and 99mTc-sulfur colloid SPECT CT findings with gross and histopathological correlation. Abdom Imaging. 2010;35:683-689.
- Falk GA, Nooli NP, Morris-Stiff G, Plesec TP, Rosenblatt S. Sclerosing angiomatoid nodular transformation (SANT) of the spleen: case report and review of the literature. Int J Surg Case Rep. 2012;3:492-500.
- Jang KM, Kim SH, Hwang J, Lee SJ, Kang TW, Lee MW, et al. Differentiation of malignant from benign focal splenic lesions: added value of diffusion-weighted MRI. Am J Roentgenol. 2014;203:803-812.
- Yoshimura N, Saito K, Shirota N, et al. Two cases of sclerosing angiomatoid nodular transformation of the spleen with gradual growth: usefulness of diffusion-weighted imaging. Clin Radiol. 2015;39:315-317.
- Metser U, Miller E, Kessler A, Lerman H, Lievshitz G, Oren R, et al. Solid splenic masses: evaluation with 18F-FDG PET/CT. J Nucl Med. 2005;46(1):52-59.
- Gutzeit A, Stuckmann G, Dommann-Scherrer C. Sclerosing angiomatoid nodular transformation (SANT) of the spleen: sonographic finding. J Clin Ultrasound. 2009;37:308-311.
- Gaetke-Udager K, Wasnik AP, Kaza RK, Al-Hawary MM, Maturen KE, et al. Multimodality imaging of splenic lesions and the role of non-vascular, image-guided intervention. Abdom Imaging. 2014;95:570-587.
- Kaza RK, Azar S, Al-Hawary MM, Francis IR. Primary and secondary neoplasms of the spleen. Cancer Imaging. 2010;10:173-182.
- Wang JH, Ma XL, Ren FY, Zuo CJ, Tian JM, Wang ZF, et al. Multi-modality imaging findings of splenic hamartoma: a report of nine cases and review of the literature. Abdom Imaging. 2013;38(1):154-162.