Introduction
Systemic lupus erythematosus (SLE) is more prevalent in western countries but with increasing awareness and availability of modern diagnostic facilities it is not uncommon in India. This autoimmune disease has a capability of involving almost every organ in the body [
1]. Mitral valve prolapse (MVP) syndrome is a commonly overlooked association of SLE. MVP is thought to be the most common form of valvular heart disease in SLE patients (25% of lupus patients vs 9% of controls) [
2]. It may present as an early indicator before other symptoms of SLE floridly develop.
Case Report
A 17-year young unmarried Indian lady presented with history of fever for three months. It was initially of low grade but suddenly changed to high grade for last 7 days along with anorexia and significant weight loss (she lost 7 kg in last 4 months). She was on penicillin prophylaxis for seven months because of suspected rheumatic mitral valve disease. She had never suffered from palpitation or shortness of breath or any joint pain. There were no other important past, personal or family history or any history of unprotected sex. Her immunization was completed as per national schedule. There was no history of travel in the recent past.
General examination revealed pallor with tachycardia (112/min) and trachypnea (30/min). Her blood pressure was 108/70 mmHg. Bodyweight was 36 kg with a body mass index (BMI) of 19.18 kg/m2. There was no icterus, edema, lymphadenopathy or bony tenderness. Her cardiovascular system examination revealed mid systolic murmur (grade 2/5) with radiation towards left second intercostal space. Important findings from other systemic examination were bilateral basal crepitations and mild hepatosplenomegaly. Information from neurological examination was generalized weakness and wasting with a power of 4/5 in all four limbs. Reflexes were normal.
Initial investigations showed hemoglobin of 10.9 gm/dL (normocytic normochromic), with a raised ESR 110 (1st hour) and an elevated CRP (85 mg/L) with a normal white cell but low to normal platelet (150,000/dL) counts. Her capillary blood glucose was normal. Screening results for malaria, enteric fever, dengue fever, leishmaniasis, HIV and viral hepatitis were negative. ABG showed hyperlactatemia, otherwise normal (pH: 7.44, PO2: 84 mmHg, pCO2 35 mmHg, HCO3 18 mEq/L, sodium 135 mEq/L, potassium 4.8 mEq/L, lactate of 2.2 mmol/L). Routine examination of urine revealed pus cells of 6-7/HPF, without any RBC, crystal, cast or organism. Chest X-ray was normal. Blood cultures (c/s) for anaerobic and aerobic organisms were sent.
She was empirically started on anti-tubercular drugs keeping disseminated TB in mind along with treatment for infective endocarditis (ceftiaxone and gentamycin). Her blood culture sensivity showed Klebsiella pneumoniae, and ceftrioxane was continued as the organism was sensitive according to antibiogram. There was hepatosplenomegaly from contrast enhance CT thorax and abdomen. Sputum ZN stain, Gram stain and culture sensivity did not reveal any organism. Anti-tubercular drugs were immediately stopped. Echocardiography (TTE & TEE) showed presence of MVP (mitral valve prolapse) with ejection fraction of 65% and mild MR without any features of endocarditis. Over the next couple of days her well-being and appetite improved. High rise of temperature subsided but the pattern changed toa continuous fever of about 37.8ºC.
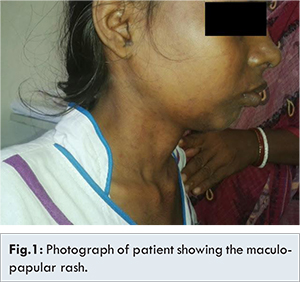
On 5th day of her admission there were generalized tonic clonic convulsions (GTCS) which improved with antiepileptic drugs. CECT brain and cerebrospinal fluid reports were normal (Glucose: 69 gm/dL, protein: 0.7 gm/dL, cells count 20, all lymphocytes). EEG showed generalized dysrhythmia. Thyroid functions, serum calcium, renal functions and electrolytes were normal. On 6th day, maculo-papular rash was seen over both extremities, trunk and neck [Fig.1]. Dermatologist consultation was taken. Drug lists were rechecked. She received penicillin as RHD prophylaxis on every third week of the month for last 7 months and occasional acetaminophen for fever. There was also history of azithromycin intake for 5 days in two separate occasions and the latest event was 20 days before admission. The possibility of drug rash was excluded. Skin biopsy was taken from back of the chest (from the fresh lesion) and her skin biopsy revealed damaged vessel wall with infiltration of inflammatory cells, mostly lymphocytes along with few neutrophils.
Hematological tests were repeated and now the platelet count was low (90,000/dL), procalcitonin (0.17 ng/mL, < 0.5 normal) and normal CRP but ESR was 69 in 1st hour. ANA (by immunoflurosence method) was positive in 1/360 and homogenous in pattern. Anti-ds DNA and anti-phospholipid antibody were also positive but anti-Sm was negative.
At this moment our diagnosis was SLE with MVP complicated by gram negative septicemia. On 8th day we started IV methyl prednisolone 1 gm for three days. That time she was not under any antibiotic coverage. We started oral prednisolone from 11th day with a plan to tapper it gradually as per guidelines. First dose of cyclophosphamide was given on fourteen day of admission. Now she is doing well. She has already completed 5th cycle of cyclophosphamide pulse therapy and remains afebrile for last five follow up.
Discussion
Systemic lupus erythematosus (SLE) is an immune-mediated disease. It can affect almost every organ of the human body. Females are commonly affected in their reproductive age group [
1]. SLE is diagnosed based on the presence of auto-antibodies and clinical manifestation [
1,
3]. Only presence of antibodies does not confirm SLE. Organs are involved in variable frequencies. Commonest form of skin involvement is the photosensitive rash, but vasculitis can be seen upto 20% cases [
1]. Pericarditis is the commonest form of cardiac involvement which is seen in 30%-50% cases, but mitral valves prolapsed (MVP) is not an uncommon finding. MVP is more commonly found in patients positive for anti-cardiolipin antibody [
3,
4]. Cognitive dysfunction and seizure are seen in 60% and 20% of the patients respectively [
1]. Among the other organs, renal involvement is more common in Asians [
1]. Immunosuppressant is the main stay of treatment. Though there is no clear guidelines regarding use of cyclophosphamide in central nervous system involvement in lupus, still there are several small studies to support its use [
5,
6].
The lymphatic and hematogenous spread of TB is known as miliary TB [
7]. It is a severe form of extrapulmonary TB. Early diagnosis and treatment are needed to stop fatal outcome. CT scan of chest and tissue biopsy from affected organs has an important role in diagnosis [
8]. Rheumatic heart disease is common in tropical countries and low socioeconomic groups. Several studies in recent past show that RHD is still a major health problem in Southeast Asia [
9]. Mitral valve prolapse syndrome is the most common form of valvular heart disease and usually a benign condition [
10]. It may present with varied symptoms like chest pain, palpitation, life threatening arrhythmias, mitral regurgitation etc. [
10]. Echocardiography diagnostic criteria for MVP [10] are well established and MVP can be diagnosed firmly with these criteria. Secondary mitral valve prolapsed is seen in hereditary and other type of connective tissue diseases [
10]. Two important studies have concluded with inference that MVP is more commonly found in SLE patients than general population, and MVP might be an early indication of connective tissue disease [
5,
6]. They also showed positive correlation between anti-cardiolipin antibody and MVP.
Our patient presented with fever and weight loss which subsequently reveled a Gram negative septicemia. She did not fulfill the Duke’s criteria for infective endocarditis. There was no evidence of TB and anti-tubercular drugs started empirically were immediately stopped. We also excluded lymphoma and Brucellosis with adequate investigations. Diagnosis of SLE was done from low platelet counts, CNS involvement, positive ANA, positive anti-ds DNA and positive anti phospholipids antibody (4 points among 11, according to ACR guideline anti-ds DNA and anti-phospholipid come under single heading immunological disordered and carry only one point). Our patient also suffered from MVP which is a clue of her autoimmune disease.
Conclusion
This young lady has been suffering from PUO. Various treatment modalities were applied empirically, however a careful cardiological examination and relevant investigations subsequently revealed the cause as lupus. Though Klebsiella infection may have aggravated her clinical features but only lupus can explain whole spectrum on its own. A more careful investigation for the cause of her MVP might reveal the SLE in an early stage and prevent the flare.
References
- Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison’s Principles of Internal Medicine, 18th Ed. New York: McGraw-Hill Medical.Volume-1(319):2724.
- Evangelopoulos M, Alevizaki M, Toumanidis S, Sotou D, Evangelopoulos C, Koutras D, et al. Mitral valve prolapse in systemic lupus erythematosus patients: clinical and immunological aspects. Lupus. 2003;12(4):308-311.
- Hochberg M. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis & Rheumatism. 1997;40(9):1725-1725.
- Evangelopoulos M, Toumanidis S, Sotou D, Evangelopoulos C, Mavrikakis M, Alevizaki M, et al. Mitral valve prolapse in young healthy individuals. An early index of autoimmunity? Lupus. 2009;18(5):436-440.
- Petri M. Cyclophosphamide: new approaches for systemic lupus erythematosus. Lupus. 2004;13(5):366-371.
- Tanaka Y. Recent progress in neuropsychiatric systemic lupus erythematosus; Brain Nerve. 2013;65(11):1255-1267.
- Sharma SK, Mohan A, Sharma A. Challenges in the diagnosis & treatment of miliary tuberculosis. Indian J Med Res. 2012;135(5):703-730.
- Sia I, Wieland M. Current Concepts in the Management of Tuberculosis. Mayo Clinic Proceedings. 2011;86(4):348-361.
- Saxena A, Ramakrishnan S, Roy A, Seth S, Krishnan A, Misra P, et al. Prevalence and outcome of subclinical rheumatic heart disease in India: The RHEUMATIC (Rheumatic Heart Echo Utilisation and Monitoring Actuarial Trends in Indian Children) study. Heart. 2011;97(24):2018-2022.
- Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald’s Heart Disease, 9th edition. Elsevier Health Sciences. pp. 1669-1674.