Introduction
Intracranial lipomas are not frequently finding lesions. According to theory presented by Verga [
1] and supported by Truwit and Barkovich [
2], they are congenitally malformed tissue found because of abnormal persistence and mal-differentiation of the meninx premitiva. Intracranial lipomas are mainly found in or near the midline and are usually associated with other brain parenchymal and cerebral vascular malformations. Common locations are interhemispheric region, corpus callosum, superior cerebellar cistern, quadrigeminal cistern, cerebellopontine angle cistern and sylvian cistern. Rarely, they are found over cerebral surfaces. In our case we found an intracranial lipoma located in between two dural leafs over cerebral hemispheric region which is very rare and never mentioned in any literature previously.
Case Report
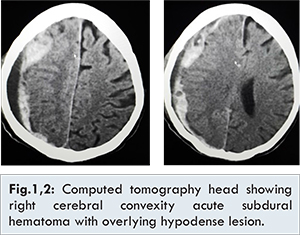
A 48 years old male patient was admitted to trauma centre with history of head injury due to road traffic accident. At the time of admission, patient was unconscious with labored breathing. Patient had a lacerated wound of approximately 2x3 cm in size over right forehead. On examination, patient vitals were normal and no any other external injury was present. His Glasgow Coma Score (GCS) was 6/15 (E1V2M3) and pupils were size of 2-3 mm and bilaterally sluggishly reacting to light. In view of low GCS and respiratory difficulty, he was intubated urgently and put on ventilatory support. NCCT head revealed a high density lesion over right fronto-temporo-parietal region with an overlying low density area making an impression of hyperacute with acute subdural hemorrhage (SDH) associated with significant midline shift towards left side [Fig.1,2]. He was immediately taken for craniotomy and hematoma evacuation.
Patient shifted to Operation Theater where an urgent right side fronto-parieto-occipto-temporal decompressive craniectomy was done. After craniectomy, durotomy was done which showed an yellowish colored tissue resembling lipoma presented just beneath the dura [Fig.3]. During removal of tissue, vascular pedicle was found coming from inner side and supplying the fatty tissue. Vascular pedicle was coagulated and cut. Fatty tissue was removed and sent for histo-pathological examination. After removal of fatty tissue, another layer of dura was seen just beneath the fatty tissue [Fig.4]. Again durotomy of the inner layer was done which showed clotted blood which was removed [Fig.5]. Brain pulsation was seen after removal of acute subdural hematoma. Lax duroplasty was done using galea of the scalp and patient shifted to ICU. Histopathology confirmed the lipomatous origin of specimen.
Discussion
Intracranial lipomas are rare lesions. They accounts for about 0.1-0.34% of all intracranial tumors [
3]. Intracranial lipomas are mainly found in or near the midline and are usually associated with other brain parenchymal and cerebral vascular malformations. Commonly founded locations are interhemispheric region, corpus callosum, superior cerebellar cistern, quadrigeminal cistern, cerebellopontine angle cistern and sylvian cistern. Intracerebral midline locations are most common site including pericallosal cistern accounting for about 45-50% of all cases [
4]. Rest of the locations including quadrigeminal cistern accounts for 25%, cerebellopontine angle cistern accounts for 9%, superior cerebellar cistern and sylvian cistern accounts for 5% of cases respectively. Rarely they may be present over cerebral surfaces [
5-
8].
Intracranial lipomas are usually seen in association with different types of other CNS abnormalities like agenesis of corpus callosum, absence of septum pellucidum, spina bifida, encephalocoel, myelomeningocoel, cortical dysplasia and vermian hypoplasia [
3,
7,
8]. They may also present with vascular anomalies like intracranial aneurysms [
9,
10].
Most of the intracranial lipomas have indolent course. Generally they remain asymptomatic and diagnosed incidentally on autopsy or computed tomography as seen in our case. In our case it was quite interesting that there was partial duplication of dura with lipomatous tissue interposed between them. Symptomatic intracranial lipomas are very rare and symptoms depend upon location of the lipoma and associated abnormalities. Eighty percent of cerebellopontine angle lesions, 50% of callosal, 50% of sylvian fissure and 20% of quadrigeminal-ambient cistern lipoma become symptomatic. They may present with seizure, paralyses, mental retardation, cranial nerve impairment, behavioral abnormalities and headache. Lipomas located in the region of ambient and quadrigeminal cisterns may cause obstructive hydrocephalus and could present with sign of raised intracranial pressure.
Lipomas are seen as a hypodense lesion in nonenhanced computed tomography with attenuation value ranging from -39 HU to -80 HU. On contrast CT, they show no enhancement. Some peripheral calcification may be present. In MRI they present as high signal in T1 sequence, moderate to high signal in T2 sequence, no enhancement in gadolinium sequence and low signal in fat set sequences. Asymptomatic intracranial lipomas are treated conservatively. Lipomas have tendency to engulf vital structures like cranial nerves and vessels which makes surgical treatment technically challenging and hazardous. Patients with seizure disorders are usually managed with antiepileptic drugs. Surgical interventions are usually reserved for intractable seizures and symptomatic lesions not amenable for medical management.
Conclusion
This case report should be taken as a reminder that lipomas are ubiquitous lesion and they could present anywhere even at that sites where they were never expected previously like interdural location.
References
- Verga P. Lipoma ed osteolipomi della pia madre. Tumori. 1929;15:321-357.
- Truwit CL, Barkovich AJ. Pathogenesis of intracranial lipoma: an MR study in 42 patients. AJR Am J Roentgenol. 1990;155:855-865.
- Fitoz S, Atasoy C, Erden I, Akyar S. Intracranial lipoma with extracranial extension through foramen ovale in a patient with encephalocraniocutaneous lipomatosis syndrome. Neuroradiology. 2002;44:175-178.
- Maiuri F, Cirillo S, Simonetti L, De Simone MR, Gangemi M. Intracranial lipomas: diagnostic and therapeutic considerations. J Neurosurg Sci. 1988;32:161-167.
- Britt PM, Bindal AK, Balko MG, Yeh HS. Lipoma of the cerebral cortex: Case Report. Acta Neurochir (Wien). 1993;121:88-92.
- Fujii Y, Konishi Y, Kriyama M, Hori C, Sudo M. Lipoma on surface of centroparietal lobes. Pediatr Neurol. 1993;9:144-146.
- Sasaki H, Yoshida K, Wakamoto H, Otani M, Toya S. Lipomas of the frontal lobe. Clin Neurol Neurosurg. 1996;98:27-31.
- Kakita A, Inenaga C, Kameyama S, Masuda H, Ueno T, Honma J, et al. Cerebral lipoma and underlying cortex of the temporal lobe: pathological features associated with the malformation. Acta Neuropathol. 2005;109:339-345.
- Futami K, Kimura A, Yamashita J. Intracranial lipoma associated with cerebral saccular aneurysm. J Neurosurg. 1992;77(4):640-642.
- Yamamoto M, Kuwabara S, Uozumi T. Lipoma of the corpus callosum associated with distal anterior cerebral artery aneurysm. A case report. Hiroshima J Med Sci. 1989;38(3):157-160.