Introduction
Over 500 years, many syndromes and diseases have been examined for HLA markers; HLA-related diseases are mostly observed in the HLA-DR and DQ genes. Idiopathic hemochromatosis, C2-C4A-C4B deficiencies, spinocerebellar ataxia, insulin-dependent diabetes mellitus, and celiac disease are just some of those diseases [
1-
3]. In this study, we illustrate a 30-year-old female Friedrich’s ataxia (FA) patient who came to our clinic with chronic inflammatory backache who was eventually diagnosed with Ankylosing Spondylitis (AS) and celiac disease (CD).
Case Report
The 30-year-old female presented to the Physical Medicine and Rehabilitation clinic due to chronic backache. She had backache for several years along with morning stiffness that lasted all day with pain in bilateral hip joints. The patient did not have any history of joint swelling, skin lesions, oral ulcers, dysphagia, abdominal pain, Raynaud phenomenon and gastrointestinal symptoms.
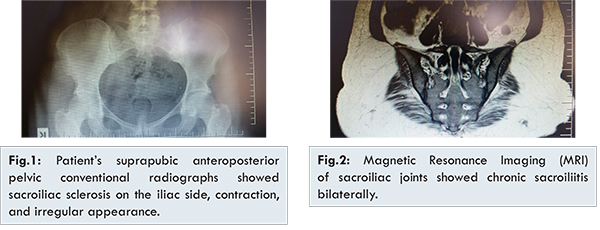
The patient was known case of FA and had physiotherapy 4 years ago to treat imbalance and loss of strength in the legs. Physical examination revealed an ataxic gait pattern and thoracic spinal, particularly lumbar spinal motion restriction (lumbar Schober: 2 cm). Both hip movements, especially rotational movements were limited, and hamstring shortness was apparent. Both lower extremities showed 1 to 2/5 weakness and hyporeflexia (++). Dysesthesia was observed, but the level couldn’t be recorded. C-reactive protein in the patient’s laboratory test was 9 mg/L (0-5). Vitamin B12 level was normal. Blood antigliadin antibodies were highly positive. HLA-B27 gene analysis was positive. Bulging that did not compress the dural sac on L4-5 was also observed via lumbar magnetic resonance imaging (MRI). In the patient’s suprapubic anteroposterior pelvic conventional radiographs, sacroiliac sclerosis on the iliac side, contraction, and irregular appearance were present; in the sacroiliac joint MRI, chronic sacroiliac joint sacroiliitis in both sacroiliac joints was observed [Fig.1,2]. There were no pathological findings in the patient’s echocardiogram or in whole-abdomen ultrasonography. Duodenal endoscopic biopsy confirmed as CD. The patient was treated with oral diclofenac sodium 500 mg, 2x1 (2 times in day, with 12- hour intervals and 1 pill each time). She was advised gluten free diet and pulsed steroid infusions for nonresponsive backache.
Spinocerebellar ataxia is a hereditary neurological disorder with heterogeneous features. Indications of cerebellar ataxia are frequently seen together with cerebellar and non-cerebellar symptoms [
4]. CD long has been associated with neurologic and psychiatric disorders including cerebellar ataxia, peripheral neuropathy, epilepsy, dementia, and depression. The association between most neurologic syndromes described and gluten sensitivity remains to be confirmed by larger epidemiologic studies. It further has been suggested that gluten sensitivity (as evidenced by high antigliadin antibodies) is a common cause of neurologic syndromes (notably cerebellar ataxia) of otherwise unknown cause. Additional studies showed high prevalence of gluten sensitivity in genetic neurodegenerative disorders such as hereditary spinocerebellar ataxia and Huntington’s disease [
5]. Neurological symptoms as a presenting of CD has become increasingly related associations [
6]. Ataxia is one of the neurological syndromes more frequently associated with CD. It is often not suspected because of a lack of symptoms or signs of malabsorption. Biopsy-confirmed CD in patients with ataxia of unknown origin is about 12%. Celiac disease-associated ataxia often lacks particular features that would distinguish it from cerebellar ataxia [
5,
6]. AS is the prototype of group of diseases which are also known as spondyloarthropathy (SpA). SpA is characterized by abnormal osteoproliferation in enthesis regions and regions that are affected by subchondral bone marrow inflammation [
1,
7].
Her disease (FA) started after age 20. There were no skeletal deformities (scoliosis or per cavus) resulting from the disease, and her reflexes were hypoactive. The patient was diagnosed with atypical, late-onset, and clinical-type FA without any systemic involvement. We could not completely distinguish whether the ataxia was celiac-related ataxia or a hereditary ataxia? She had no gastrointestinal symptoms. Additionally although the patient had backache for many years, she was told that backaches resulted from FA. When the anamnesis of patient deepened, inflammatory back pain, hip pain, morning stiffness lasting all day were the symptoms; axial AS diagnosis was finalized using radiological imaging.
Many studies showed high prevalence of gluten sensitivity in genetic neurodegenerative disorders such as hereditary spinocerebellar ataxia. It remains unclear whether gluten sensitivity contributes to the pathogenesis of these disorders or whether it represents an epiphenomenon. Diagnosis of ataxia, AS and CD diseases oinciding in a patient will be clarified by the unanswered questions of immunopathogenesis of these diseases.
References
- Kolostová K, Cerná M, Andel M. Association of HLA molecules with autoimmune diseases. Cas Lek Cesk. 2002;141(24):755-762.
- Hors J, Gony J. HL-A and disease. Adv Nephrol Necker Hosp. 1986;15:329-351.
- Caillat-Zucman S. Molecular mechanisms of HLA association with autoimmune diseases. Tissue Antigens. 2009;73(1):1-8.
- Matilla-Dueñas A, Corral-Juan M, Volpini V, Sanchez I. The spinocerebellar ataxias: clinical aspects and molecular genetics. Adv Exp Med Biol. 2012;724:351-374.
- Muthuswamy S, Agarwal S. Friedreich Ataxia: From the Eye of a Molecular Biologist. Neurologist. 2015;20(3):51-55.
- Parkinson MH, Boesch S, Nachbauer W, Mariotti C, Giunti P. Clinical features of Friedreich’s ataxia: classical and atypical phenotypes. J Neurochem. 2013;126 Suppl. 1:103-117.
- Collins A. Clinical neurogenetics: Friedreich ataxia. Neurol Clin. 2013;31(4):1095-1120.