|
|
|
|
|
Birt- Hogg- Dube Syndrome: Difficulties in Diagnosis and Management in Developing Countries
|
|
|
Dilip Nikam, Mahesh Rewadkar, Irfanulla Khan
Department of Radiotherapy & Oncology, Cama & Albless Hospitals, Grant Government Medical College & Sir J. J. Group of Hospitals, Mumbai, Maharashtra, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Dilip Nikam
Email: docnik128@yahoo.com
|
|
|
|
|
|
|
|
|
Received:
13-MAY-2016 |
Accepted:
28-JUL-2016 |
Published Online:
10-OCT-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Birt-Hogg-Dube syndrome (BHD) is a rare autosomal dominant inherited cancer syndrome characterized by benign tumors of the hair follicle (fibrofolliculoma), pulmonary cysts, spontaneous pneumothorax and increased risk for renal carcinoma. In developing countries like India where affordability and facility for FLCN BHD gene study are not available, presence of skin lesions, pulmonary cyst and renal hybrid tumor comprising of both oncocytoma and chromophobe renal cell carcinoma can contribute for diagnosis. |
|
|
|
|
|
Keywords :
|
Birt-Hogg-Dube syndrome, Cysts, Genes, Hair Follicle, Kidney Neoplasms.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff3033110000002005000001000500 6go6ckt5b5idvals|672 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Birt-Hogg-Dube syndrome (BHD) is rare inherited syndrome characterised by multiple fibrofolliculomas, pulmonary cysts, pneumothorax and renal tumors. Fibrofolliculomas and lung cysts are most common manifestation. Renal tumors with variable histologies develop in about 30% of BHD affected individual, most frequently chromophobe renal carcinoma and hybrid onocytic tumors. Metastasis is uncommon but may develop. A genetic linkage analysis identified BHD gene, FLCN on short arm of chromosome 17 [1,2].
Case Report
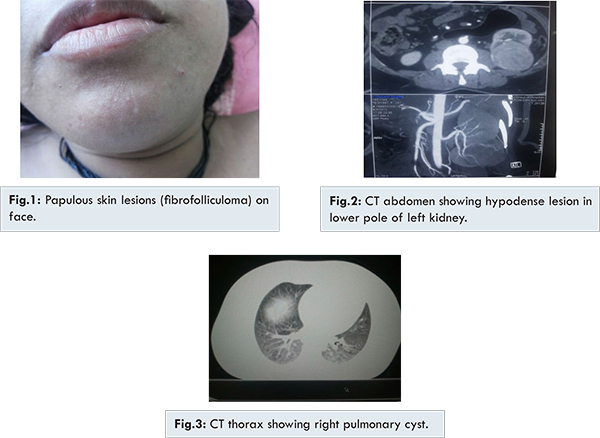
A 28 year old, premenopausal, nulliparous, female consulted for gradually progressive, dull abdominal pain and hematuria since 1 month. In general, the examination was within normal limits except few papulous skin lesions (fibrofolliculoma) on face, and back [Fig.1]. No organomegaly was noticed on abdominal examination. The patient’s haematological and biochemical workup was within normal limits. Urine routine and microscopic examination was within normal limits. CT abdomen and pelvis revealed left kidney measuring 11.7x4.8 cm with well-defined hypodense lesion measuring 5x5x4.7 cm seen arising from lower moiety of left kidney [Fig.2]. This lesion showed early enhancement on arterial phase and wash out on delayed phase. Bilateral renal veins and inferior vena cava showed normal contrast opacification and no evidence of thrombosis within. Right kidney was within normal limits. There were multiple enlarged non-necrotic lymph nodes along lesser curvature, peripancratic and paraaortic region largest measuring 1.9x1.3 cm in perigastric region. Liver appears normal in attenuation and enhancement pattern except simple cyst in IVa segment and calcified granuloma in VI segment. A small enhancing nodule was seen in medial segment of right middle lobe of lung with multiple enlarged lymph-nodes in pretracheal, para-tracheal, bilateral hilar and sub-carinal region largest measuring 1.2x1.0 cm in pretracheal region. Abdominal aortogram and left renal angiogram showed relatively avascular mass in lower pole of left kidney. CT thorax showed small cyst in right lung [Fig.3]. Ultrasound guided biopsy from left kidney mass reported renal cell neoplasm showing oncocytic change with differential diagnosis of renal cell carcinoma and oncocytoma favouring more on later. Pulmonary function test showed restrictive ventilator defect with MVV more than 50%.
The patient was operated for left radical nephrectomy with retroperitoneal lymph-nodes dissection. The patient tolerated the procedure well and post-operative period was uneventful. Drain was removed on fifth day and staple sutures were removed on tenth day. Histopathology showed oncocytoma, pericapsular fat showed presence of tumor. There was neither lymphovascular invasion, nor renal veins invasion. The dissected lymph-nodes were negative for malignancy. The slides and paraffin blocks were reviewed at Tata Memorial Centre which confirmed the diagnosis of renal hybrid tumor comprising of both oncocytoma and chromophobe renal cell carcinoma. Tumor cells show diffuse and strong cytoplasmic positivity for CD10, focally positive for CK7 and weak diffuse positive for C-kit favouring oncocytoma while negative for vimentin, AMACR.
In view of clinical and pathological findings, we advised a genetic linkage analysis of the BHD gene, FLCN located on short arm of chromosome 17, but she has refused to do so for socioeconomically reasons.
Discussion
Birt-Hogg-Dube syndrome (BHD) is uncommon and associated with mutations in the FLCN gene, which encodes folliculin, which is preferentially expressed in the skin, kidney, and lung. The syndrome was characterized by the presence of fibrofolliculomas and/or trichodiscomas (skin), pulmonary cysts, spontaneous pneumothorax (lung), and renal tumors (kidney) [4]. The European Birt-Hogg-Dube Consortium has proposed a series of major and minor criteria for establishing the diagnosis. At least five fibrofolliculomas or trichodiscomas, at least 1 confirmed histologically, of adult onset and pathogenic germline mutation in FLCN are major criteria. The minor criteria are multiple lung cysts: basally located with or without spontaneous pneumothorax; renal cancer: early onset (<50 years), multifocal or bilateral renal cancer, or renal cancer of characteristic histologic forms (oncocytic-chromophobe hybrid histology) and first-degree relative with Birt-Hogg-Dube syndrome (BHD). Patients should fulfil one major or two minor criterion for diagnosis of Birt-Hogg-Dube syndrome (BHD) [3]. Pneumothorax and chest pain are clinically important signs and symptoms and warrant a thorough medical examination [4], and it is important to keep in mind that the onset of repeated pneumothorax generally starts at an earlier age than RCC in patients with BHD [5].
Staging and management of renal cancer is no different to renal cancer in patients without the syndrome. Once diagnosed, treatment is usually surgical, leaving as much renal parenchyma as possible with nephron sparing techniques instead of radical nephrectomy [6]. In the event of metastases, rapamycin analogs may be considered, given the implication of the FLCN gene in regulating the mTOR pathway, although more studies are needed to demonstrate benefit [1]. In our case, the patient was presented with renal symptoms and underwent for left radical nephrectomy with retroperitoneal lymph-nodes dissection. As the disease was limited no further adjuvant therapy was advised. She was referred to dermatologist for evaluation. In view of small pulmonary cysts of lung, she was evaluated by respiratory medicine consultant.
Conclusion
In developing countries like India, affordability and facility for FLCN BHD gene study are not available. The European Birt-Hogg-Dube Consortium proposed major and minor criteria for establishing the diagnosis seems reasonable.
References
- Menko FH, Van steensel MA, Giraud S, Friis-Hansen L, Richard S, Ungari S, et al. European BHD Consortium. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol. 2009;10(12):1199-1206.
- Nickerson ML, Warren MB, Toro JR, Matrosova V, Glenn G, Turner ML, et al. Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with the Birt-Hogg-Dubé syndrome. Cancer Cell. 2002;2(2):157-164.
- López V, Jordá E, Monteagudo C. Birt-Hogg-Dubé syndrome: an update. Actas Dermosifiliogr. 2012;103(3):198-206.
- Toro JR, Wei MH, Glenn GM, Weinreich M, O Toure, Vocke C, et al. BHD mutations, clinical and molecular genetic investigations of Birt-Hogg-Dube syndrome: a new series of 50 families and a review of published reports. J Med Genet. 2008;45:321-331.
- Zbar B, Alvord WG, Glenn G, Turner M, Pavlovich CP, Schmidt, et al. Risk of renal and colonic neoplasms and spontaneous pneumothorax in the Birt-Hogg-Dube syndrome. Cancer Epidemiol Biomarkers Prev. 2002;11:393-400.
- Herring JC, Enquist EG, Chernoff A, Linehan WM, Choyke PL, Walther MM. Parenchymal sparing surgery in patients with hereditary renal cell carcinoma: a 10-year experience. J Urol. 2001;165:777-781.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Nikam D, Rewadkar M, Khan IBirt- Hogg- Dube Syndrome: Difficulties in Diagnosis and Management in Developing Countries.JCR 2016;6:482-484 |
|
Nikam D, Rewadkar M, Khan IBirt- Hogg- Dube Syndrome: Difficulties in Diagnosis and Management in Developing Countries.JCR [serial online] 2016[cited 2025 Jul 25];6:482-484. Available from: http://www.casereports.in/articles/6/4/Birt-Hogg-Dube-Syndrome.html |

|
|
|
|
|