|
|
|
|
|
Glucocorticoid Induced Knee Osteonecrosis
|
|
|
Tuba Tülay Koca
Physical Medicine and Rehabilitation Clinic, Malatya State Hospital, Malatya, Turkey. |
|
|
|
|
|
Corresponding Author:
|
Dr. Tuba Tülay Koca
Email: tuba_baglan@yahoo.com
|
|
|
|
|
|
|
|
|
Received:
03-AUG-2016 |
Accepted:
09-NOV-2016 |
Published Online:
30-DEC-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Osteonecrosis (ON) is a complex disease, and has been rarely reported. Vascular failure, metabolic changes, and sub-chondral fractures play an important role in the pathogenesis of ON. Case Report: Here, we present a case of 54-year-old male with knee osteonecrosis following a one month course of steroid therapy. Conclusion: Non-traumatic ON is a clinical case that occurs in rheumatologic and hematologic diseases depending on the chronic use of glucocorticoids. Additionally other underlying risk factors should be considered as seen in our case. If it is not diagnosed early, it can cause serious joint deformities and disabilities. |
|
|
|
|
|
Keywords :
|
Arthritis, Glucocorticoids, Knee Joint, Male, Osteonecrosis.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff242114000000f401000001000d00 6go6ckt5b5idvals|703 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Osteonecrosis (ON) is a complex disease,and its etiology has not been defined yet. Vascular failure, metabolic changes, and subchondral fractures play an important role in the pathogenesis of ON [1]. One case of knee osteonecrosis is documented with correlated roentographic and magnetic resonance imaging. ON may lead to serious joint deformities and disabilities if diagnosis is delayed.
Case Report
A 54-year-old male patient visited outpatient clinic because of pain and swelling on his left knee for last 10 days. No history of trauma was present. He was incidentally diagnosed to be suffering from chronic immune thrombocytopenic purpura (ITP) almost 5 years back and treated by splenectomy. He was later noted to be suffering from systemic lupus erythematous (SLE) and received four doses of cyclophophamide. In addition, medical treatment was also given to the patient with azathioprine 50 mg 1x1 oral tablet, hydroxychloroquine (HQ) 200 mg 1x1 oral tablet, metoprolol succinate 50 mg 1x1, and acetylsalicylic acid 100 mg 1x1 oral tablet. A low-dose methyl-prednisolone oral treatment was also given to him from time to time. Since he had frequent inhalation problems, he had a lung computed tomography scan, and the results matched those of infiltrative lung disease.
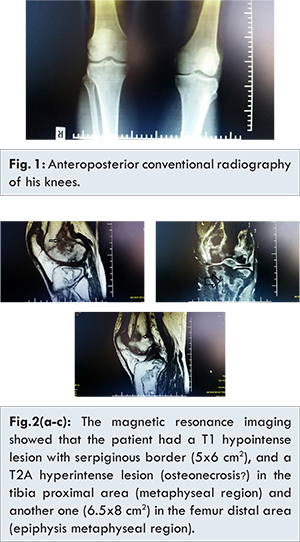
One month ago, the patient visited rheumatology outpatient clinic because of severe widespread knee pain. His sedimentation value was 61 mm/hour (0-20), and C-reactive protein value was 1.53 mg/dL (0-5), cholesterol level was 200 mg/dL (0-200), low density lipoprotein level (LDL) was 132.3 mg/dL (60-129), thrombocyte count was 432x103/µL (142-534). Other test values were within the normal range. The cyclophosphamide dose of the patient was increased to 2x1 per day and the methyl-prednisolone dose was decreased to 1x8 mg after using with a dose of 16 mg per day for 10 days. In his control there was minimal arthritis signs on his left knee with no pathological sign in conventional radiography [Fig.1]. His knee movements were near complete and without pain. Magnetic resonance imaging (MRI) showed that he had a T1 hypointense lesion with a serpiginous border (5x6 cm2), and a T2A hyperintense lesion (osteonecrosis?) in the proximal area of the tibia (metaphyseal region) and another one (6.5x8 cm2) in the distal area of the femur (epiphysis metaphyseal region) [Fig. 2a-c]. The patient was thought to have glucocorticoid-related secondary ON.
Spontaneous ON is usually seen in people who are in their 60s, whereas unilateral and secondary ON is usually seen in young people with bilateral and multifocal involvement [1]. The most frequent cause of non-traumatic ON is the use of glucocorticoids (GCs). The risk of developing ON due to the long-term use of GCs is between 9% and 40%. ON is a serious condition that involves bone disruption and is treated with surgical reconstruction. Other causes of ON can be alcoholism, infections, hyperbaric cases, storage diseases, coagulation defects, bone infiltration, and autoimmune diseases. Additionally, many idiopathic cases can also cause ON. Besides discouraging excessive use of GCs, other risk factors also need to be eliminated by knowing detailed medical history of patients [2,3].
The pathogenesis of the disease involves vascular pressure, bone and cell death, or defective bone repair. An early diagnosis of ON is possible using MRI and bone scintigraphy. Early detection depends on prognostic stage and localization [1]. A number of modalities are used in the treatment, such as conservative treatment, arthroscopic debridement, core decompression, microfracture, autologous osteochondral transplantation, chondrocyte culture, high tibial osteotomy, and arthroplasties [1]. Zhao et al. studied the risk factors in patients with SLE suffering from symptomatic knee ON. They found that cutaneous vasculitis, hyperfibrinogenemia, and increased immunoglobulin G levels might be possible risk factors. They also found that HQ might act as a protector against ON. Lupus activity and hyper-coagulation state are also found to play a role in knee development [4]. Another study by Kuroda found high triglyceride levels to be a risk factor for ON development in patients with SLE [5].
The patient in this study, who was diagnosed with ITP and SLE, showed a difference in non-traumatic avascular necrosis development in both femoral and tibial metaphyseal regions after short-term, low-dose usage methyl-prednisolone (16 mg for 10 days/8 mg for 10 days). In addition, since the patient also had chronic ITP, he carried a pro-coagulation risk factor for ON development. Unlike osteonecrosis of the femoral head, osteonecrosis of the knee is considered to be related to sub-chondral fragility fractures but not glucocorticoid itself. Septic arthritis was not predicted in this patient (leukocyte was normal, no acute arthritis). Recent studies have suggested hyperlipidemia as a risk factor for ON development. The lipid profile of the patient was not considered and no anti-hyperlipidemic medication was given to him. He was referred to orthopedics clinic after including an anti-hyperlipidemic medication in his treatment.
Conclusion
Non-traumatic ON is a clinical case that occurs in rheumatologic and hematologic diseases depending on the chronic use of glucocorticoids. Additionally other underlying risk factors should be considered as seen in our case. If it is not diagnosed early, it can cause serious joint deformities and disabilities.
References
- Akgün I, Unlü MC. Osteonecrosis of the knee. Acta Orthop Traumatol Turc. 2007;41 Suppl. 2:123-137.
- Pape D, Seil R, Fritsch E, Rupp S, Kohn D. Prevalence of spontaneous osteonecrosis of the medial femoral condyle in elderly patients. Knee Surg Sports Traumatol Arthrosc. 2002;10:233-240.
- Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32(2):94-124.
- Zhao L, Wu X, Wu H, Su J, Zhang W, Zhao Y, Zhang X, Zheng W. Symptomatic knee osteonecrosis in patients with systemic lupus erythematosus: a case-control study. Rheumatol Int. 2016;36:1105-1111.
- Kuroda T, Tanabe N, Wakamatsu A, Takai C, Sato H, Nakatsue T, et al. High triglyceride is a risk factor for silent osteonecrosis of the femoral head in systemic lupus erythematosus. Clin Rheumatol. 2015;34(12):2071-2077.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Tülay Koca TGlucocorticoid Induced Knee Osteonecrosis.JCR 2016;6:598-600 |
|
Tülay Koca TGlucocorticoid Induced Knee Osteonecrosis.JCR [serial online] 2016[cited 2024 Apr 27];6:598-600. Available from: http://www.casereports.in/articles/6/4/Glucocorticoid-Induced-Knee-Osteonecrosis.html |

|
|
|
|
|