Introduction
Caudal anesthesia is epidural anesthesia of the cauda equina roots in the sacral canal, approached through the sacral hiatus. This technique is a common pediatric regional procedure which is quick to learn and easy to perform, with high success and low complication rates. But no procedure is risk free, it may cause delayed respiratory depression and failed or incomplete block may need more medications causing over-sedation, hypoventilation and respiratory acidosis [
1]. Respiratory acidosis may be brought about by complications either involving the lungs and respiratory system or signals from the respiratory center that controls breathing [
2].
Maximum respiratory stimulant effects are attained by a PaCO2 around 100 mm Hg. The PCO2- ventilation response curve is generally displaced to the right, and its slope is reduced by anesthetics and other depressant drugs. With deep anesthesia, the response curve gradually slopes downward, and CO2 then acts as a respiratory depressant. In patients with ventilatory failure, CO2 narcosis occurs when the PaCO2 rises to more than 90 to 120 mm Hg [
3].
Case Report
A eight months old child weight 7.3 kg presented with missing left testis and ballooning of penile foreskin, diagnosed as undescended testis (left) with phimosis. The patient was scheduled for left orchidopexy and circumcision under caudal anesthesia. Pre-anaesthesia checkup was done 24 hours prior to surgery and written informed consent was obtained from parents. Preoperative fasting guidelines were followed and baby kept nil per oral for six hours. After evaluating history, physical examination and investigations, baby was accepted in American Society of Anesthesiologists (ASA) grade I, attending nurse accompanied the baby inside theater. On arrival at operation theatre, baby induced with halothane, intravenous line established and analgesic dose of ketamine @ 1mg/kg given before caudal block. The patient was connected with baseline monitors. Caudal block was performed in lateral decubitus position with back flexed and head extended to avoid airway occlusion; three ml 0.5% plain bupivacaine, 1.5 ml 2% lidocaine and one ml distilled water were administered as local anesthetics. Pin-prick test was elicited before proceeding towards surgery. Baby was kept sedated in supine position by intravenous diazepam, intermittent ketamine and fentanyl in incremental doses when required; oxygenation maintained with face mask. At certain stage of operation baby started moving and straining, precaution calls of surgeon about straining were managed by intermittent dose of ketamine and fentanyl; at one stage baby started desaturating and became brady-arrythymic. Right at that moment, ‘call for help’ warning came. Fellow anesthesiologists rushed towards that theater, ACLS instituted firstly with bag-mask ventilation then airway secured with endotracheal intubation and medications like atropine, hydrocortisone was administered as per body weight.
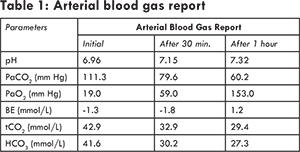
Examination revealed brady-arrythymia, no effective respiration and pulse oximetry reading was erroneous, to be more accurate pulse oximeter failed to read arterial pulse and oxygen saturation, baby was cyanosed. Arterial blood gas revealed severe respiratory acidosis where pH=6.96, PaCO2=111.3 mm Hg, PaO2=19 mm Hg, BE= -1.3, tCO2= 42.9 mmol/L, HCO3= 41.6 mmol/L. Evaluating physical findings and arterial blood gas report baby was diagnosed as a case of severe respiratory acidosis. Based on ABG reports baby was then given sodium-bicarbonate as per formula [0.3 x weights (kg) x base deficit (mEq/L)]. Deliberate manual hyperventilation by Ayre’s T piece continued about an hour. At certain stage, baby started taking spontaneous respiration then artificial ventilation synchronized with spontaneous respiration for couple of minutes. Again blood sample was taken for ABG reports 30 minutes apart of first sample to see level of PaCO2 and effectiveness of deliberate manual ventilation. One hour period of close monitoring and constant diligence could correct blood chemistry to almost normal.
As PaCO2 washed away due to hyperventilation; baby woke up and started taking spontaneous respiration, patient was extubated and kept in recovery position inside theater to see how baby maintained airway and oxygenation. After ensuring patency of airway and oxygenation baby was shifted to post-operative ward in recovery position. Baby was then discharged on 3rd post-operative day.
Discussion
Regional anesthesia has wide-ranging benefits but requires technical expertise. Its use in neonates, infants, and children continue to escalate, either as a sole anesthetic or in combination with general anesthesia, to provide both intraoperative and initial postoperative analgesia [4]. In all areas of anesthesia, safety and efficiency have valued goals, and in developing countries additional challenges are due to shortages of anesthetic drugs, supplies and monitoring equipments. In developing countries, caudal block with general anesthesia or caudal anesthesia alone can provide safe, reliable and efficient analgesia and/ or anesthesia for both high risk and general pediatric surgical patients [
5].
This technical skill can be easily learnt and may be modified to extend analgesia in the postoperative period (with the addition of opioids or continuous techniques) or replace into general anesthesia in circumstances where either the equipments or drugs are not available [5]. Nevertheless, the risk-benefit analysis must take into account failure rate and the incidence of complications. Between 5%-25% of caudal epidural blocks can be considered “failed or incomplete”. The anesthesiologist may not be able to identify the anatomic landmarks and are therefore unable to insert the caudal needle into the epidural space [
5]. At any cost, patient safety should remain the focus while performing regional anesthesia. The preferred regional technique should be considered within the context of risk versus benefit, based on age of the child, nature of the surgery, available facilities and skill of the practitioner [
6,
7].
In our case, caudal anesthesia was provided under general anesthesia and patient was kept sedated by intermittent dose of ketamine and fentanyl. During operation baby was straining which might be due to inadequate or failed block remain unnoticed as a result oversedation ensued hypoventilation and accumulation of CO2 upto 111 mm of Hg. Eventually baby developed severe respiratory acidosis, became brady-arrhythmics and went into cardiac arrest.
Conclusion
To perform caudal block safely in pediatrics, it is mandatory to know the anatomical and physiological differences, the correct technical procedures, the safety measures before LA injections. Beside those close monitoring of ventilation, oxygenation, and circulation during and after blockade are required to minimize risk.
In our case, baby was straining and hypoventilating during operation contributed to accumulation of PCO2 upto 111.3 mm of Hg which could be minimized by close monitoring of respiratory pattern and cardiac arrest could have been avoided.
References
- Raux O, Dadure C, Carr J, Rochette A, Capdevila X. Paediatric caudal anaesthesia. Update in Anaesthesia. 2015;30(1):32-36.
-
Fluid Electrolyte and Acid-Base Disorders. In: Family Medicine Principles and Practices. 5th New York; Springer-Verlag, 1998.
-
Churchill Livingstone. Part-D. Respiratory Physiology and Respiratory Function during Anesthesia, Chapter-15, Section 2; Physiology and Anesthesia.
-
Bosenberg A. Benefits of regional anesthesia in children. Pediatric Anesthesia. 2012; 22:10-18.
-
Edler A, Wellis VG. Caudal Epidural Anesthesia for Pediatric Patients: a safe reliable and effective method in developing countries. Update in Anaesthesia. 1998 No. 8.
-
Bosenberg AT. Regional anaesthesia in children: an update. South Afr J Anaesth Analg. 2013;19(6):282-288.
-
Gregory GA, Andropoulos DB. Gregory’s Pediatric Anesthesia, 5th UK; Blackwell Publishing Ltd. 2012: 441.