|
|
|
|
|
Placenta Percreta with Occult Uterine Rupture in the First Trimester
|
|
|
Tabitha L. Schrufer-Poland, Paul Singh, Cristiano Jodicke, Ryan Reynolds, Sara Reynolds, Dev Maulik
Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, University of Missouri Kansas City School of Medicine, Kansas City, Missouri 64108. |
|
|
|
|
|
Corresponding Author:
|
Dr. Tabitha L. Schrufer-Poland
Email: schruferpolandt@umkc.edu
|
|
|
|
|
|
|
|
|
Received:
09-FEB-2016 |
Accepted:
06-DEC-2016 |
Published Online:
25-NOV-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Placenta percreta is a rare finding in the first trimester and is often associated with severe maternal morbidity. Herein we describe a case of placenta percreta with occult uterine rupture in the first trimester in a patient with a history of two previous cesarean deliveries. Imaging was concerning for placenta accreta. Following onset of acute abdominal pain, she underwent exploratory laparoscopy, which was negative for overt uterine scar dehiscence. She ultimately underwent total abdominal hysterectomy at 14 weeks following severe bleeding, with intraoperative and histologic findings consistent with placenta percreta with dehiscence of the anterior lower uterine segment below the level of, and obscured by the vesicouterine peritoneum.
Bleeding and severe abdominal pain in the first trimester in the context of prior uterine instrumentation should always prompt evaluation of the scar, by imaging in a stable patient, and by direct visualization if necessitated. However, maintenance of clinical suspicion for uterine scar dehiscence is warranted in patients at high risk even in the absence of direct visualization intra-operatively.
|
|
|
|
|
|
Keywords :
|
Abdominal Pain, Hystrectomy, Placenta Accreta, Pregnancy, Uterine Rupture.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa4e812000000a201000001001000 6go6ckt5b5idvals|689 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Placenta percreta is a potentially catastrophic complication of pregnancy and may be associated with uterine rupture, life-threatening hemorrhage, and major surgical morbidity. Due to a combination of the increasing incidence of cesarean delivery as well as improving diagnostic modalities, the incidence and recognition of placenta accreta has increased. Herein we describe a case of placenta percreta with occult uterine rupture during the first trimester in a patient with a history of two prior cesarean deliveries.
Case Report
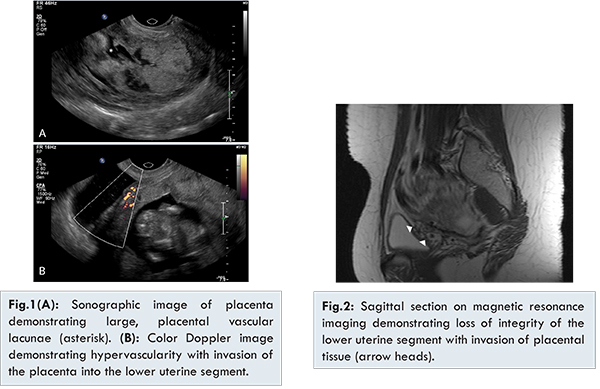
A 21-year old gravida 3, para 2, with a history of two prior cesarean deliveries underwent an initial fetal ultrasound at 12 weeks demonstrating an enlarged placenta filled with lacunar lakes completely overlying the internal os. A pelvic MRI was obtained which was concerning for invasion of the placenta into the lower uterine segment. She was counseled regarding management options and at that time, desired expectant management. At 13 weeks gestation the patient was admitted for severe abdominal pain with vaginal bleeding. Ultrasound identified possible small defect in the anterior uterine wall with a small volume of free fluid in the cul-de-sac. An exploratory laparoscopy performed revealed a thin, but normal appearing lower uterine segment along with a small volume of blood-tinged peritoneal fluid with no obvious uterine scar dehiscence. A cystoscopy was negative for overt placental invasion. Since the patient at that time still desired to continue the pregnancy and no obvious maternal or fetal contraindications to pregnancy were identified intra-operatively, conservative management was undertaken. After one week, the patient developed heavy vaginal bleeding and elected for termination of pregnancy.
The patient underwent a total abdominal hysterectomy with intraoperative findings of placental tissue protruding through a 4 cm defect within the lower uterine segment below the level of the vesicouterine peritoneum. During her procedure, she had a sizeable hemorrhage requiring transfusion. Postoperatively, her hospital course was unremarkable; she was discharged home on postoperative day four. Pathologic examination of the uterus demonstrated a 3.6x2.9 cm defect in the anterior lower uterine segment with adherent placenta penetrating the full thickness of the uterine wall.
Discussion
Placenta accreta is characterized by a deficiency or complete absence of the normally intervening Nitabuch’s layer which separates placental villous tissue from myometrium. The uterine decidua is often replaced only by loose connective tissue, allowing for essentially unrestricted access of trophoblasts to myometrial fibers. Previously an exceedingly rare occurrence, the incidence of placenta accreta has seen a 10-fold increase, and currently approximates 3 per 1000 pregnancies [ 1, 3]. A potentially catastrophic condition, the morbidity associated with abnormal placentation is profound and may include uterine rupture, life-threatening hemorrhage and shock, injury to surrounding structures, thromboembolism, consumptive coagulopathy, and death.
Early identification of abnormal placentation allows for close follow-up, arrangement for transfer to tertiary care center, and early multidisciplinary planning and has been shown to lead to improved outcomes [ 4, 5]. With increasing utilization of first trimester screening ultrasonography, detection of abnormal placentation early in pregnancy has increased. Ultrasonic markers identified early in gestation include low implantation [ 6, 7], hypoechoic defects, subjective interpretation of thinning, and invasion into adjacent structures [ 7, 8]. Other first trimester sonographic observations seen with abnormal placentation include those which are more commonly seen at more advanced gestational ages such as an irregular myometrial-placental interface, vascular lacunae, and persistent previa [ 9, 10]. Unfortunately, the sensitivity and specificity of these markers in the first trimester is low, 41% and 88%, respectively [ 10]. Adaptation of uniform criteria has yet to be established for early detection of abnormal placentation [ 5, 11, 12], and unfortunately, despite advances in ultrasound imaging, many cases of abnormal placentation are diagnosed with massive bleeding at the time of placental separation during delivery or with dilation and curettage.
While the management of placenta percreta in a setting of acute hemorrhage or an unstable patient is relatively straightforward, the management in a stable patient in the first trimester represents a challenge. Management options abound in the literature, ranging from expectant to surgical. Few cases in the literature describe pregnancies that reach viability, fewer yet approaching term with favorable outcomes, and patients remain at risk throughout the duration of pregnancy for sudden, life-threatening complications [ 13, 14]. Therefore patients must be very carefully selected, be highly motivated, and exceptionally compliant if expectant management is to be undertaken.
Conclusion
This case emphasizes the need for maintenance of high clinical suspicion for uterine scar dehiscence in patients at high risk even in the absence of direct visualization on exploratory laparoscopy and underscores the need for early ultrasonic evaluation of a previous cesarean scar.
References
- Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. American Journal of Obstetrics and Gynecology. 2012;207(1):14-29.
- Jauniaux E, Jurkovic D. Placenta accreta: pathogenesis of a 20th century iatrogenic uterine disease. Placenta. 2012;33(4):244-251.
- Publications Committee SfM-FM, Belfort MA. Placenta accreta. American journal of obstetrics and Gynecology. 2010;203(5):430-439.
- Perez-Delboy A, Wright JD. Surgical management of placenta accreta: to leave or remove the placenta? BJOG: an international journal of obstetrics and gynaecology. 2014;121(2):163-169; discussion 9-70.
- Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. American Journal of Obstetrics and Gynecology. 2012;207(1):44 e1-13.
- Stirnemann JJ, Mousty E, Chalouhi G, Salomon LJ, Bernard JP, Ville Y. Screening for placenta accreta at 11-14 weeks of gestation. American Journal of Obstetrics and Gynecology. 2011;205(6):547 e1-6.
- Comstock CH, Lee W, Vettraino IM, Bronsteen RA. The early sonographic appearance of placenta accreta. Journal of ultrasound in medicine: official journal of the American Institute of Ultrasound in Medicine. 2003;22(1):19-23; quiz 4-6.
- Buetow MP. Sonography of placenta percreta during the first trimester. AJR American journal of Roentgenology. 2002;179(2):535.
- Abuhamad A. Morbidly adherent placenta. Seminars in perinatology. 2013;37(5):359-364.
- Rahimi-Sharbaf F, Jamal A, Mesdaghinia E, Abedzadeh-Kalahroudi M, Niroomanesh S, Atoof F. Ultrasound detection of placenta accreta in the first trimester of pregnancy. Iranian journal of Reproductive Medicine. 2014;12(6):421-426.
- Vial Y, Petignat P, Hohlfeld P. Pregnancy in a cesarean scar. Ultrasound in Obstetrics & Gynecology. 2000;16(6):592-593.
- Seow KM, Hwang JL, Tsai YL. Ultrasound diagnosis of a pregnancy in a Cesarean section scar. Ultrasound in Obstetrics & Gynecology. 2001;18(5):547-549.
- Roeters AE, Oudijk MA, Heydanus R, Bruinse HW. Pregnancy outcome after intra-abdominal bleeding due to placenta percreta at 14 weeks of gestation. Obstetrics and Gynecology. 2007;109(2 Pt2):574-576.
- El-Matary A, Akinlade R, Jolaoso A. Caesarean scar pregnancy with expectant management to full term. Journal of Obstetrics and Gynaecology. 2007;27(6):624-625.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
L. Schrufer-Poland T, Singh P, Jodicke C, Reynolds R, Reynolds S, Maulik DPlacenta Percreta with Occult Uterine Rupture in the First Trimester.JCR 2016;6:545-548 |
|
L. Schrufer-Poland T, Singh P, Jodicke C, Reynolds R, Reynolds S, Maulik DPlacenta Percreta with Occult Uterine Rupture in the First Trimester.JCR [serial online] 2016[cited 2025 Oct 16];6:545-548. Available from: http://www.casereports.in/articles/6/4/Placenta-Percreta-with-Occult-Uterine-Rupture-in-the-First-Trimester.html |

|
|
|
|
|