|
|
|
|
|
Steroid Cell Tumor Without Virilization
|
|
|
Debanti Banerjee, Kazi S. Manir, Rahul Bhowmick, Chhaya Roy
Department of Radiotherapy, R.G. Kar Medical College & Hospital, Kolkata, 700004, India. |
|
|
|
|
|
Corresponding Author:
|
Dr. Kazi S. Manir
Email: kazi.dr@gmail.com
|
|
|
|
|
|
|
|
|
Received:
07-JUN-2016 |
Accepted:
17-AUG-2016 |
Published Online:
15-OCT-2016 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Steroid cell tumors of the ovary are rare type of sex-cord stromal tumor, comprising less than 0.1% of ovarian tumors. Steroid cell tumors produce testosterone causing virilizing symptoms like hirsutism, male pattern of baldness etc. Steroid cell tumor of ovary without any virilizing symptoms is rare. Serum testosterone and dehydroepiandrosterone (DHEA) measurement is essential for evaluation of androgenic excess. Here we present steroid cell tumor ovary with malignant potential without any features of virilization but with some unusual findings like osteopenia and underweight.
|
|
|
|
|
|
Keywords :
|
Dehydroepiandrosterone, Hirsutism, Ovarian Neoplasms, Sex-Cord-Gonadal Stromal Tumors, Testosterone.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff645211000000ab03000001000b00 6go6ckt5b5idvals|673 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Ovarian steroid cell tumor is a rare sex-cord stromal tumor comprising less than 0.1% of all ovarian tumors [1]. Steroid cell tumor was previously designated as lipoid cell tumor, one third of these tumors are considered malignant. Steroid especially testosterone, is produced by these tumors, causing symptoms like hirsutism, male pattern of hair loss, amenorrhea, oligomenorrhea [2,3]. We report a patient of malignant steroid cell tumor without any symptom of virilization.
Case Report
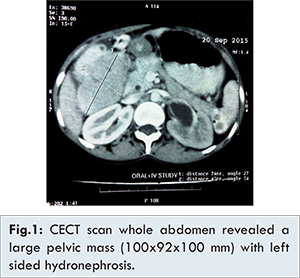
A 22 years old unmarried girl attended our gynaecology outpatient department with complaint of amenorrhea for last 5 months. She had menarche at 13 years of age and since then her menstruation cycles were normal till onset of illness. Her weight was 30 kg and height of 132 cm. No significant past or family was elicited. On physical examination her breast development was normal. There was no male pattern of hair growth, voice change, male pattern of hair loss or cliteromegaly. Sonography of lower abdomen showed bilateral adnexal solid heterogeneous mass (right>left)- likely ovarian along with left sided hydronephrosis. Contrast Enhanced Computer Tomography (CECT) scan whole abdomen revealed a large pelvic mass (100×92×100 mm) with left sided hydronephrosis, peri-portal and peri-pancreatic lymphadenopathy along with metastasis in right lobe of liver [Fig.1]. Laboratory investigation showed normal serum levels of T3, T4, serum estrogen, serum testosterone, 17 alpha hydroxy progesterone and dehydro-epiandrosterone (DHEA-S) and CA-125. Serum TSH level was mildly elevated. Serum LDH level (449 U/L) and serum AFP level (6530.78 U/L) were grossly elevated. Digital X-ray of peripheral limbs showed osteoporosis. She underwent laparotomy and de-bulking surgery. Histopathology report showed presence of solid ovarian tissue composed of lobules, trabeculae and solid areas of polygonal cells having distinct cytoplasmic region, centrally placed nuclei with nuclear pseudo-inclusion and granular eosinophilic cytoplasm. Focal areas of hemorrhage, necrosis and atypical nuclei were noted. The pathological diagnosis was steroid cell tumor with high malignant potential (size >7 cm, necrosis and nuclear atypia). Immunohistochemistry (IHC) report showed that neoplastic cells did not stain with epithelial membrane antigen (EMA) but stained for Inhibin. Post-operative CECT scan of abdomen revealed residual bilateral adnexal lesions with left sided pelvic lymphadenopathy and metastasis in liver. Post-operative serum level of LDH and AFP were still elevated. Adjuvant chemotherapy was started with bleomycin, etoposide and cisplatin, three weekly for four cycles. For evaluation of osteoporosis DEXA scan was done. It showed osteopenia with moderate fracture risk and total body soft tissue quantification showed a low fat percentage value favouring underweight. For osteopenia we have started prophylactic injection zoledronic acid.
Ovarian steroid cell are grouped under sex cord tumor and they are usually benign, unilateral and formed by steroid cell proliferation. Sex cord stromal tumors of ovary are developed from sex cord and stromal component of ovary [4,5]. Steroid cell tumors generally show androgenic symptoms like amenorrhea, male pattern of hair growth, hair loss, cliteromegaly, regression of breast development [6]. In our patient the tumor was bilateral and had high malignant potential and caused liver metastasis. Steroid cell tumors usually show androgenic symptoms like amenorrhea and abnormal hair growth and hair loss. Our patient presented only with amenorrhea. There were no features of virilization like hirsutism, abnormal hair loss, clitoromegaly, which is rare.
For the evaluation of androgen excess, testosterone and DHEA-S are the first laboratory tests to be measured [7]. In our patient, testosterone and serum DHEA-S levels were normal. Ultrasound and CECT scan showed bilateral mass in both ovaries, normal adrenal gland and no ascites. Steroid cell tumors are generally unilateral and benign. Malignancy is generally associated with identification of the histo-pathological findings of two or more mitotic figures per 10 high power fields (92% malignant), necrosis (86% malignant), size of 7 cm or more (78% malignant), hemorrhage (77% malignant), grade 2/3 nuclear atypia (64% malignant) [8]. In our patient pathology report showed large tumor of 15×12×10 cm (size > 7 cm, necrosis, hemorrhage and nuclear atypia) indicating steroid cell tumor with high malignant potential. In addition to these microscopic findings steroid cell tumor can be differentiated from other tumors with help of IHC. Sex cord stromal tumor usually stains positive for Inhibin and negative for EMA [9]. In our patient the tumor also stained positive for Inhibin and negative for EMA. Surgery is the most important and hallmark treatment. But complete de-bulking was not possible in our case. Due to high malignant potential and post-operative increased serum markers adjuvant chemotherapy was started.
Conclusion
Steroid cell tumors are rare and androgenic symptoms with increased testosterone levels are important suspicious signs of a functional ovarian tumor. It rarely presents as non-functional malignant tumor. Complete hormonal evaluation is essential. For diagnosis of malignancy, pathological evaluation and IHC is very necessary. Features of amenorrhea and elevated markers level do not normalize following surgery if there is residual or metastatic disease. Postoperative chemotherapy is essential in malignant cases.
References
- Young RH, Scully RE. Steroid cell tumours of the ovary. In: Fox H., Wells M. (eds.). Obstetric & Gynaecological Pathology. Churchill Livingstone Edinburgh, U.K. 2003: pp. 845-56.
- Powell JL, Dulaney DP, Shiro BC. Androgen - secreting steroid cell tumor of the ovary. South Med J. 2000;93(7):1201-1204.
- Young RH, Clement PB, Scully RE. Sex cord stromal, steroid cell and germ cell tumours of ovary. In: Mills S E, Carter D, Greenson DK, Reuter VE, Stoler MH (eds.) Sternberg’s Diagnostic Surgical Pathology Volume 2, Lippincott Williams and Wiilkins, Philadelphia, PA, U.S.A., 5th edition; 2009: pp. 2592-2595.
- Boyraz G, Selcuk I, Yusifli Z, Usubutun A, Gunalp S. Steroid Cell Tumor of the ovary in an Adolescent: A Rare Case Report. Case Rep M. 2013;2013:527698.
- Scully RE, Young RH, Clement PB. Steroid cell tumours. In: Tumours of the Ovary, Mal- Developed Gonads, Fallopian tube and Broad Ligament, Armed Forces Institute of Pathology, Washington DC, USA, 1996: pp. 227-238.
- Aimakhu VE, Adeleye JE, Hendrickse M. Masculinizing tumours of the ovary. J Natl Med Assoc. 1976;68(1):34-38.
- Martin KA, Chang RJ, Ehrmann DA, Ibanez L, Lobo RA, Shapiro J, et al. Evaluation and Treatment of hirsutism in premenopausal women: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93(4):1105-1120.
- Hayes MC, Scully RE. Ovarian steroid cell tumour (not otherwise specified) A clinicopathogical analysis of 63 cases. Am J Surg Pathol. 1987;11(11):835-845.
- Zhao C, Vinh TN, McManus K, Dabbs D, Barner R, Vang R. Identification of the most sensitive and robust immunohistochemical markers in different categories of ovarian sex cord stromal tumours. Am J Surg Pathol. 2009;33(3):354-366.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Banerjee D, S. Manir K, Bhowmick R, Roy CSteroid Cell Tumor Without Virilization.JCR 2016;6:485-487 |
|
Banerjee D, S. Manir K, Bhowmick R, Roy CSteroid Cell Tumor Without Virilization.JCR [serial online] 2016[cited 2024 Apr 27];6:485-487. Available from: http://www.casereports.in/articles/6/4/Steroid-Cell-Tumor-Without-Virilization.html |

|
|
|
|
|