Introduction
Postoperative pneumothorax (PNX) is a rare, but a life-threatening complication. It requires prompt diagnosis, and should be immediately treated. The most common causes of iatrogenic PNX are chest trauma, upper extremity blocks, subclavian or internal jugular vein catheterization, and barotrauma during mechanical ventilation [1]. An elevated peak inspiratory pressure (PIP), high positive end-expiratory pressure (PEEP), and high transalveolar pressure may lead to alveolar over-distention, alveolar rupture and pulmonary barotraumas [2,3].
The manual bag and mask ventilation is commonly used in intubated patients, especially during transport, and cardiopulmonary resuscitation efforts. The risk of barotrauma is greater during manual ventilation of an intubated patient, since air cannot leak out [4,5]. We report a case of PNX and pneumo-mediastinum after manual ventilation with a bag valve device in an intubated patient during transport.
Case Report
A 65-year-old woman, ASA status class II, was scheduled for a lumbar disc stabilization surgery under general anesthesia. Clinical examination at pre-anaesthesia clinic was within normal limits. Her past history was suggestive of hypertension. Laboratory investigations, chest X-ray and electrocardiograph (ECG) were normal.
In operating room, the patient was monitored with ECG, non-invasive blood pressure, and pulse oximetry (SpO2) till completion of surgery. After pre-oxygenation with 100% oxygen, general anesthesia was induced with 100 µg of fentanyl, 150 mg of propofol, and 40 mg of rocuronium bromide intravenously. After mask ventilation for 3 min, the tracheal intubation was performed with 7.0 sized endotracheal tube (ETT) without complications. After the location of the ETT was confirmed, it was fixed. The volume controlled mechanical ventilation was commenced (tidal volume of 8 ml/kg, and a respiratory rate of 12 breaths/min). The anesthesia was maintained with oxygen (2 L/min), nitrous oxide (2 L/min), and sevoflurane (1.5-2.0%, end-tidal concentration). The patient was hemodynamically stable during the operation. The surgery was completed in 210 minutes.
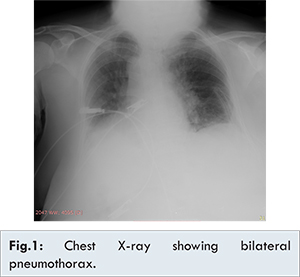
On completion of surgery, the intubated patient was transported to the imaging center. During transport, the patient received manual ventilation with a bag valve device, and was monitored with pulse oximetry. After she was brought back to the operating room, the neuromuscular block was reversed with atropine and neostigmine. The patient was extubated, when the respiration seemed adequate, and the conscious was recovered. Her vital signs were stable (blood pressure: 135/75 mmHg, heart rate: 82 beats/min, and SpO2: 98%), so she was transferred to the postoperative recovery unit (PACU). Approximately five minutes after arrival, she developed dyspnea, chest pain, cyanosis, and severe agitation. During this period, the patient’s vital signs were: a SpO2 of 72%, a heart rate of 125 beats/min, and a blood pressure of 70/45 mmHg. The patient was oxygenated with a face mask (5 L/min), and was immediately transferred to the ICU for respiratory support. A portable chest X-ray, and CT were taken. The radiological examinations revealed a bilateral pneumothorax which was more prominent on the left side, and pneumo-mediastinum [Fig.1]. The left chest tube was placed, and the patient made a rapid recovery. On the third postoperative day, chest X-ray showed complete expansion of the lung, and the chest drain was removed. She was shifted to the ward, and was uneventfully discharged from the hospital on the sixth postoperative day.
Bag valve ventilation devices are commonly used in intubated patient especially during transportation. The devices are generally safe, but they may lead to many complications as a result of manufacturing defects or improper applications. The clinicians may generate very high airway pressure during manual ventilation. High positive pressures might lead to alveolar damage and pulmonary barotrauma, and this can result in pneumo-mediastinum, pneumothorax, pneumo-peritoneum, or tension pneumothorax. Barotrauma after positive pressure ventilation has been reported in numerous studies, but there are few reports of barotrauma after manual ventilation of intubated patients during transport [2,3]. Moreover, the displacement of the ETT, and the patient’s movements may also increase the risk of barotrauma.
In the postoperative period, PNX needs to be differentiated from bronchospasm, pulmonary embolism, pulmonary edema, and pulmonary aspiration. The most common presentations of PNX include tachycardia, chest pain, dyspnea, anxiety, decreased breath sounds, hypoxemia, and hypotension. In our case, she developed hypoxemia, dyspnea, tachypnea, chest pain, and tachycardia. During this period, the patient was oxygenated with face mask, and was immediately transferred to the ICU. A chest-X ray and CT scan thorax confirmed the presence of a bilateral pneumothorax and pneumo-mediastinum. The left chest drain was placed, and the patient made a good recovery rapidly. The patient was discharged uneventfully at the sixth postoperative day.
Conclusion
The manual ventilation with bag valve devices should be done with lower tidal volumes and increased time for full exhalation between breaths. It should be noted that high pressure ventilation carries the risk of PNX. Anesthesiologist should pay careful attention to avoid airway pressure elevation, when applying manual ventilation with bag-valve devices in intubated patients during transport.
References
- Choi WI. Pneumothorax. Tuberc Respir Dis. 2014;76(3):99-104.
- Erden IA, Onal O, Pamuk AG, Akinci SB, Aypar U. Sudden pneumothorax develeoped during ventilation with a bag valve device while transportation. Duzce Med Journal. 2012;14(3):94-96.
- Kim JB, Jung HJ, Lee JM, Im KS, Kim DJ. Barotrauma developed during intra-hospital transfer: A case report. Korean J Anesthesiol. 2010;59(Suppl): 218-221.
- Ricard JD. Manual ventilation and risk of barotrauma: primum nonnocere. Respir Care. 2005;50:338-339.
- Turki M, Young MP, Wagers SS, Bates JH. Peak pressures duringmanual ventilation. Respir Care. 2005;50:340-344.