Introduction
Asphyxia derives from the Greek words a “without” and sphyxis, “heartbeat” is a condition of deficient tissue oxygenation leading to hypoxia with different etiologies. Traumatic asphyxia is a mechanical cause of hypoxia resulting from external compression and blunt thoracic trauma. It is also called crush asphyxia [
1]. Historically Ollivier, Tardieu and Perthes were the first ones in describing this phenomenon [
2-
4].
Possible causes of traumatic asphyxia include accidents, human stampedes, asthmatic exacerbation, epileptic status and severe emesis, the latter mainly seen in pediatric population [
5-
8]. Both, in the American and in the European literature, the incident of this syndrome has not been yet achieved, especially for underdiagnoses, because even when the patient in many of the descriptions has the typical clinical manifestations, is not labeled as a specific syndrome in the blunt trauma to the chest.
Case Report
A 61 year-old male was brought to the emergency department with a history of crushing thoracic accidental trauma. He is a mechanic, sustained crush injury over his chest and abdomen when supports of bus which he was repairing broke down. 911 was called, he was under the bus for approximately 5 minutes before he was rescued and found non-ambulatory with transient loss of consciousness.
At arrival to the emergency department he was conscious with a cervical collar in place. He was managed as a trauma patient, his airway was described as patent, tachypneic but in no major respiratory distress, breath sounds were clear bilaterally with equal intensity in both hemithoraces, no pathologic sounds were auscultated. Cardiovascular examination showed normal blood pressure, heart rate of 76 beats per minute, pulse oximetry of 97% on 2 liters of oxygen nasal cannula. There were no penetrating thoracic injuries, no paradoxical movement of the chest, and heart sounds were regular without murmurs, rubs or gallops. Abdomen without any signs of peritonism, an extended focused assessment with sonography was reported as normal. No gross neurologic deficit was found, 15 points on Glasgow coma scale, pupils equal, round, reactive to light. His appearance was described as cyanotic with edema and petechial lesions localized in his upper thorax, neck and head
[Fig.1a]. Periorbital ecchymosis and bilateral conjunctival hemorrhages were also seen
[Fig.1b]. During workup a comprehensive metabolic panel and a complete blood count were normal. An arterial blood gas showed mild acute respiratory alkalosis. An electrocardiogram showed normal sinus rhythm. Troponin levels were within normal limits.
An antero-posterior chest X-ray documented a left mid-clavicular fracture with diffuse infiltrates in right lower base
[Fig.2a], no mediastinal widening, no pneumothorax or pleural effusion was noticed. Cervical spine X-rays and abdominal radiographs were unremarkable. A left femur fracture was found on pelvis X-ray. The patient was taken to the computed tomography scan, a brain scan ruled out hemorrhage of the brain and skull fractures. The following is the summary of his chest computed tomography scan: unipolar fractures in left posterior first, second and fourth ribs and comminuted fracture of left posterior third rib
[Fig.2b], trachea, major bronchi and major vascular structures all unaffected. The lung fields were remarkable for mild air trapping, mild bilateral pleural effusion
[Fig.3], and bilateral passive segmental postero-basal atelectasis.
During his hospitalization the patient was hemodynamically stable, managed conservatively with supplemental oxygen and analgesics as needed, using incentive spirometry and followed up with daily chest X-rays with expected clinical evolution of a pulmonary contusion. Ophthalmology ruled out underlying retinal hemorrhage or detachment. His femur fracture was managed by orthopedics with a closed reduction. His ecchymotic lesions, petechiae and subconjunctival hemorrhages improved with time.
Discussion
The pathophysiology of traumatic asphyxia describes acute chest compression results in increased intra-thoracic pressure, driving blood from the right atrium into superior vena cava territories which have valves that are unable to prevent backflow when encountering excessive pressure. The backpressure within the venous system at the level of small venules and capillaries of head and neck, results in petechial hemorrhages, blood stasis, which subsequently generates cyanosis [
9]. A critical event in this process is a forced sudden inspiration with closing glottis, which happens as response to fear, and is crucial to increase the intrathoracic pressure into a level that damages the vasculature [
10].
The extension of the signs and possible sequels, depends on the duration and severity of the thoracic compression at which the patient was exposed [
11]. Among the typical physical examination findings of traumatic asphyxia it is worth mentioning the following: intense vascular congestion in the superior aspect of the thorax, with petechial hemorrhages in face, neck and conjunctiva, this set of clinical manifestations is known also as mask of Morestin [
1,
7,
12]. Other signs may accompany the classic clinical manifestations of this pathology, being the most common mental confusion, amnesia, psychomotor agitation and hyperpyrexia. At ocular level there may be exophthalmos, double vision, loss of visual acuity, and blurry vision, these alterations are explained by retinal hemorrhages [
12]. Additionally, epistaxis due to capillary break and hearing loss due to edema in Eustachian tubes or even hemo-tympanum may be seen [
11-
13]. The natural history of all these injuries is characterized by a progressive resolution, including the neurological symptoms previously mentioned which, in general, revert in 24 hours without sequels. The development of sequels depends on the duration of the thoracic compression. A prolonged compression is associated with increased mortality, mainly secondary to apnea and hypoxemia.
The diagnosis of traumatic asphyxia is made by clinical history and physical examination. The approach of these patients must be integral, initiating for assuring the airway, the patient must place supine with the head tilt to 30 degrees, in order to diminish intracranial pressure [
8-
12]. Oxygen therapy and fluids must begin at once and must consider the need to place mechanical ventilation according to patient requirements and extension of lung injuries [
12-
13]. We must not forget that this pathology is the result of a direct trauma on the thorax, therefore traumatic injuries as pulmonary contusion, hemothorax, pneumothorax, esophageal rupture, laceration of great vessels, myocardial contusion, flail chest, hepatic or splenic lacerations and injuries in pelvis must be rapidly ruled out.
As shown
[Fig.4], several lesions secondary to blunt chest trauma there has been described. Rib fractures constitute a major part of blunt chest trauma and each additional rib fracture is associated with an increasing likelihood of developing complications. Respiratory complications develop in the setting of rib fractures as a consequence of splinting of the thorax from pain and mechanical instability resulting in inadequate ventilation. Even an isolated rib fracture is associated with significant consequences, particularly in the elderly population. This causes decreased lung volumes, atelectasis, and may progress to pneumonia, respiratory failure, need for prolonged ventilation and possible death. The majority of reviewed papers recommended a multi-disciplinary approach including chest physiotherapy, analgesic and surgical intervention; depending upon the number and clinical presentation of the patient [
14].
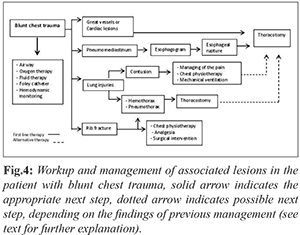
Pulmonary contusion is another consequence commonly observed in these patients. Generally they develop in the first 24 hours and it resolves in approximately 1 week. In one third of the cases there are not evident findings of this pathology in initial radiological studies, so the recommendation is to reassess the patient with serial physical examinations and radiological studies. Managing of the pain and chest physiotherapy are the cornerstones of the treatment. Mechanical ventilation should be considered on basis of patient´s clinical scenario. Another frequently associated complication is pneumothorax, which is a purely clinical diagnosis; the patient may have tachypnea, hypoxia, decrease or absence of breath sound or unilateral lung hyper-resonance. The management include placement of a chest tube. Another possible finding in these patients corresponds to hemothorax, the initial managing of it is also placement of a chest tube, nevertheless an immediate drainage of =1500 mL and state of shock are indications of emergent thoracotomy as the next step [
15]. If pneumo-mediastinum is related, it is necessary to fulfill an esophagogram, in order to detect an esophageal rupture that, in case of being associated, must proceed to prompt surgical treatment. When there are associated injuries of great vessels or structural cardiac injuries, the patient must undergo immediate surgery [
16].
The prognosis of these patients generally is favorable, however the morbidity and mortality depends on several factors including the age of the patient, duration of compression, severity of pulmonary injuries and existence of associated injuries specifically those that involve the cardiovascular system or central nervous system [
5,
8,
11].
Conclusion
The diagnosis of traumatic asphyxia is made by the clinical manifestations of increased craniocervical pressure associated with blunt chest trauma. The approach of the patients should be multidisciplinary. We must recognize and treat potential life threating associated lesions. The prognosis is usually favorable and depends on several factors such as age, time of compression and associated injuries.
Contributors: ROJ: patient management, literature review, KVB: literature review, writing manuscript. EMAA: patient management, manuscript review. KVB will act as guarantor. All authors approved the final version of the manuscript.
Funding: None;
Competing interests: None stated.
References
- Lateef H. Traumatic Asphyxia with Diaphragmatic Injury: A Case Report. Oman Med J. 2015;30:142-145.
- Burrell H, Crandon L. Traumatic Apnea or Asphyxia. Boston Med Surg J. 1902;146:13-15.
- Byard R, Wick R, Simpson E, Gilbert J. The pathological features and circumstances of death of lethal crush/traumatic asphyxia in adults-A 25-year study. Forensic Sci Int. 2006;159:200-205.
- Salazar Vargas C, Alvarado Arce M, Araya Gutierrez H, Soto Pacheco L. Pneumotorax catamenial. Rev Méd Costa Rica y Centroamérica. 1997;54:141-144
- Luviano García J, Cataneo Cerna A. Asfixia traumática: Reporte de un caso. Rev Asoc Mex Med Crit Ter Int. 2011;25:157-159.
- El Koraichi A, Benafitou R, Tadili J, Rafii M, El Kharaz H, Al Haddoury M, et al. Syndrome d’asphyxie traumatique ou syndrome de Perthes : à propos de deux observations pédiatriques. Ann Fr Anesth Reanim. 2012;31:259-261.
- Vargas Alvarado, E. Medicina Forense y Deontología Médica. Ciencias Forenses para Médicos y Abogados. 2da ed. Costa Rica. Editorial Trillas. 1991, pp. 370-371.
- Kamali S, Kesici S, Gunduz I, Kesici U. A Case of Traumatic Asphyxia due to Motorcycle Accident. Case Rep Emerg Med. 2013;2013:857131.
- Amit S, Anju R, Jyoti B.Traumatic Asphyxial Deaths Due to an Uncontrolled Crowd at Railway station: Two case reports. J Indian Forensic Sci. 2010;32:254-256.
- Montes Tapia F, Barreto Arroyo I, Cura Esquivel I, Rodríguez Taméz A, de la O Cavazos M. Traumatic Asphyxia. Pediatr Emerg Care. 2014;30:114-116.
- Sertariou E, Papaioannou V, Koulatsis G, Theodorou V, Pneumatikos I. Traumatic asphyxia due to blunt chest trauma: a case report and literature review. J Case Rep Med. 2012;6:257.
- Karamustafaoglu Y, Yavasman I, Tiryaki S, Yoruk Y. Traumatic asphyxia. Int J Emerg Med. 2010;3:379-380.
- Eken C, Yigit O. Traumatic asphyxia: a rare syndrome in trauma patients. Int J Emerg Med. 2009;2:255-256.
- Unsworth A, Curtis K, Asha, S. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resusc Emerg Med. 2015;23(1):17.
- Mowery N, Gunter O, Collier B, Diaz J, Haut E, Hildreth A, et al. Practice Management Guidelines for Management of Hemothorax and Occult Pneumothorax. The Journal of Trauma: Injury, Infection, and Critical Care. 2011;70(2):510-518.
- Navid F, Gleason T. Great Vessel and Cardiac Trauma: Diagnostic and Management Strategies. Seminars in Thoracic and Cardiovascular Surgery. 2008;20(1):31-38.