6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa441190000004104000001000000
6go6ckt5b5idvals|757
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Triad of gastric leiomyosarcoma, pulmonary chondroma and extra-adrenal paraganglioma in 1977 was described by Carney et al. and this condition has been identified as the Carneys triad (CTr) [
1]. Since 1977, more than 140 cases of the condition with different combinations of the three neoplasms have been described. Carneys triad is a syndrome of neoplasms that affect the stomach, lungs, paraganglionic system, esophagus and adrenal cortex. Multiple tumors develop in affected organs. The disorder affects young women typically and it is not familial.
Case Report
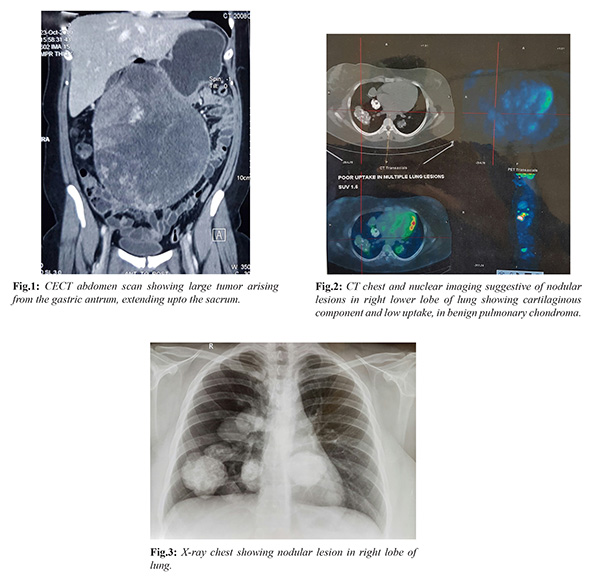
A 18-year-old girl presented with gradually worsening abdominal distension for four months. General examination findings were normal. On per abdominal examination there was hugely distended abdomen and a large intra-abdominal palpable mass with restricted mobility. Rest of the systemic examination was normal. CT scan of the abdomen and pelvis revealed a soft tissue/ mesenteric mass (22×18×12 cm) occupying abdomen and pelvis region, extending from D12 vertebral level to upper sacral vertebrae lesions in gastric fundus, focal lesion in left adrenal 1.2×0.7 cm, and multiple calcified lesions in lower lungs [Fig.1-3]. Upper gastro-intestinal (GI) endoscopic evaluation for gastric mass revealed additional multiple small polyps in stomach and duodenum; biopsy from gastric mass was suggestive of gastrointestinal stromal tumor (GIST) and of gastric polyp was negative for malignancy. Biopsy from one of the lung lesion was suggestive of chondroid hamartoma. After relevant investigations she underwent laparotomy, there were multiple masses, largest was arising from posterior wall of stomach measuring around 20×20 cm and one was at greater curvature measuring 2×1 cm and third mass near lesser curvature of stomach measuring 4×4 cm.
Few small nodules were seen on anterior and posterior wall of stomach. Complete excision of the index mass was done with partial gastrectomy, and other few lesions were removed. Complete R0 resection was not possible. She had an uneventful post-operative recovery.
Histopathology revealed malignant multifocal GISTs of stomach with high malignant potential (high mitotic index) [Fig.4]. Tumor was seen in all excisions and it was seen infiltrating deep into the muscularis propria and adventitia reaching up to the circumferential margins. The staining reactions for CD 34 and C kit (CD 117) were strongly positive while negative for CK and SMA. Gastric revised margins were free. She was discharged on oral imatinib 400 mg twice a day. On last evaluation 6 years after surgery, patient was asymptomatic; however, PET CT whole body revealed relapse of disease in the gastric remnant and metabolically active peritoneal nodules. In view of slow progression, she is being treated with imatinib.
Discussion
An association between gastric leiomyosarcoma, extra-adrenal paraganglioma and pulmonary chondroma may be associated synchronously or metachronously and are referred to as Carneys’ triad [
1,
2]. As associated tumors are rare, presence of at least two of these three tumors was considered sufficient for diagnosing the triad. Very few patients exhibit all three components of the Carney triad, and its clinical presentation is typically chronic, persistent and indolent. Our patient had pulmonary chondroma, gastric GIST and benign appearing adrenal adenoma.
The most commonly observed component of Carney triad is GIST (99%) and it is also the most common initial clinical manifestation, presenting with bleeding and associated symptoms and signs (e.g. anaemia, hematemesis, and melena). Gastric GISTs in Carney’s triad occur at an early age, have few local symptoms, have intramural origin with eventual mucosal ulceration, they present typically in the antrum and the lesser curvature, and have very slow progression of disease [
3,
4]. All these characteristics were observed in our case.
Alternative therapies for metastases from GISTs like chemotherapy, radiation, thermo-ablation or cryo-ablation are usually ineffective for treating metastatic lesions. Although the role of imatinib mesylate as a tyrosine kinase inhibitor in metastatic GISTs is well known, but till now its use in gastric GISTs as a part of Carney’s triad is rarely reported. First molecular analysis of gastric GISTs in Carney triad was performed by Diment et al. [
5], which revealed the absence of mutations in c-kit and platelet-derived growth factor receptor-A, and same findings were reported by Knop et al. [
6] and Stratakis et al. [
7]. Both Diment et al. [
5] and Stratakis and Carney [
7] concluded that, the poor treatment response of gastric GISTs in the Carney triad to imatinib mesylate might be due to the absence of c-kit and platelet-derived growth factor receptor mutations, either of which occur in most sporadic GISTs. In contrast to this, our case had strongly positive CD 34 and C kit (CD117) and the disease has been stabilized on daily oral imatinib mesylate till date. Patients who are diagnosed even with one component of the Carney’s triad should be assessed for the other components, as the triad component occurring individually is rare. Due to the extreme rarity of the triad components occurring individually Margulies and Sheps presented an algorithm for the initial assessment and continued follow-up of patients with one component of the Carney triad [
8].
Vogl et al. reported the clinical use of 18-fluoro-2-desoxyglucose PET (FDG-PET) as an imaging tool in patient follow-up programs [
9]. Metabolically active lesions seen on FDG-PET CT scans may represent paragangliomas and GIST metastases or other primary tumors. In a patient reported here PET/CT scan revealed increased standardized uptake value (SUVmax) in the gastric GIST, but minimal uptake in pulmonary chordoma. Also, it revealed recurrent lesions during follow up, two years after surgery with increased FDG-PET avidity involving fundus, pylorus, peritoneal nodules as well as liver segments VII and part of V. Thus, PET CT scans also provide a guide for follow-up during adjuvant targeted therapy.
Conclusion
This report will sensitize the physicians about the possibility of Carneys triad, especially in young females presenting with one of the three components at unusual locations. Further diagnostic testing is needed to identify early-stage tumors while curative surgery is still possible. Few patients may require long-term follow-up for detection of other components of the Carney triad.
Contributors: NVG: manuscript writing, literature search; ASP: critical inputs into the manuscript; KCP, RCM: manuscript editing, literature search. NVG will act as guarantor. All authors approved the final version of the manuscript.
Funding: None; Competing interests: None stated.
References
- Carney JA, Sheps SG, Go VL. The triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma. N Engl J Med. 1977;296:1517-1518.
- Carney JA. The triad of gastric epithelioid leiomyosarcoma, pulmonary chondroma and functioning extra-adrenal paraganglioma: a five-year review. Medicine (Baltimore). 1983;62:159-169.
- Carney JA. Gastric sarcoma, pulmonary chondroma and extra-adrenal paraganglioma (Carney’s triad): natural history, adrenocortical component and possible familial occurrence. Mayo Clin Proc. 1999;74:543-552.
- Byrne CM, Daneshjoo R, Wyatt JM. Gastrointestinal haemorrhage as a presentation of Carney’s triad. ANZ J Surg. 2007;77:88-90.
- Diment J, Tamborini E, Casali P. Carney triad: case report and molecular analysis of gastric tumor. Hum Pathol. 2005;36:112-116.
- Knop S, Schupp M, Wardelmann E. A new case of Carney triad: gastrointestinal stromal tumours and leiomyoma of the oesophagus do not show activating mutations of KIT and platelet-derived growth factor receptor alpha. J Clin Pathol. 2006;59:1097-1099.
- Stratakis CA, Carney JA. The triad of paragangliomas, gastric stromal tumours and pulmonary chondromas (Carney triad), and the dyad of paragangliomas and gastric stromal sarcomas (Carney–Stratakis syndrome): molecular genetics and clinical implications. J Intern Med. 2009;266:43-52.
- Margulies KB, Sheps SG. Carney’s triad: guidelines for management. Mayo Clin Proc. 1988;63:496-502.
- Vogl TJ, Lehnert T, Wetter A. Interventional radiology in Carney triad. Eur Radiol. 2005;15:833-837.