6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff2c741b000000ad03000001001200
6go6ckt5b5idvals|783
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Mesenteric panniculitis (MP) is an acute and chronic fibrosing inflammatory disease that affects the adipose tissue of the mesentery of the small intestine [
1]. The specific etiology of the disease is yet unclear. Mesenteric panniculitis has been connected to a variety of conditions like vasculitis, granulomatous disease, malignancies and pancreatitis [
2]. Most of the time disease is asymptomatic but when symptomatic, presentations include abdominal pain, vomiting, diarrhea, constipation and palpable abdominal mass or intestinal obstruction. The outcome of the disease is usually benign and prognosis is good in most cases.
Abdominal CT is the most sensitive imaging modality for detecting mesenteric panniculitis, but the definite diagnosis is established by biopsy [
3,
4]. Hereby we report a case of mesenteric panniculitis mimicking non-Hodgkin lymphoma.
Case Report
A 45 year male presented to Radiotherapy outpatient department with complains of abdominal lump since one year, which spontaneously regressed within 10-15 days of appearance after taking some treatment and reappeared after 10 months. The lump was associated with off and on abdominal pain but not with vomiting and fever. The patient was chronic tobacco chewer and smoker since 20 years. He was not suffering from any other chronic illness. Patient gave history of receiving one cycle of anthracyclin based chemotherapy 1 year back.
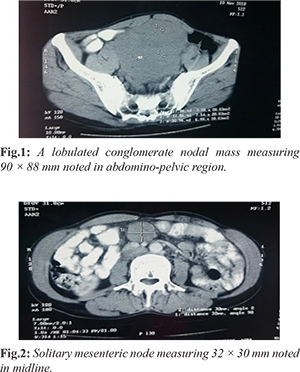
Per abdomen examination revealed a non-tender lump approximately of size 8 × 9 cm in hypogastrium which was extending to umbilical region. It was firm to hard on palpation. Blood investigations and chest X-ray were within normal limits. CECT abdomen showed extensive nodal masses in peri-portal, peri-pancreatic, paracaval, celiac, aorto-caval and para-aortic region measuring 20-60 mm. Extensive peritoneal deposits/nodal masses were noted in sub-hepatic region and pelvis on right side measuring 40-80 mm. Repeat CECT abdomen after one month revealed a lobulated conglomerate nodal mass measuring 90 × 88 mm in abdomino-pelvic region showing mild to moderate degree of heterogeneous contrast enhancement. Another solitary mesenteric node measuring 32 × 30 mm was noted in midline [Fig.1,2]. Ultrasound (USG) guided fine needle aspiration cytology (FNAC) of peri-pancreatic lymph node shows cytological overlap between reactive hyperplasia and non-Hodgkin lymphoma.
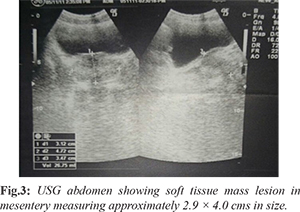
Patient was advised for biopsy, but he refused, so in view of clinical and radio-pathological correlation and patients previous history of response with chemotherapy, patient was treated with CHOP regimen. After 4 cycles of CHOP, USG revealed enlarged lymph node mass of 4.9 × 5.1 cm and another hypoechoiec lymph node in left lumbar region of size 4.8 × 5.1 cm. Patient received 4 more cycles. On clinical examination no abdominal lump was palpable but on USG abdomen mass lesion and node were persisting [Fig.3]. In view of persisting lesion and after convincing the patient, he underwent exploratory laparotomy with resection of mesenteric mass with ileal segment with anastomosis.
Histopathology from mesenteric mass shows extensively hyalinised areas with hemorrhage and cholesterol cleft, few hyalinised trabeculae with cellular lymphoid area. Section examined from the intestine were histologically unremarkable expect for mild non-specific inflammation. Lesion doesn't appear to be hemato-lymphoid neoplasm. Possibility of mesenteric panniculitis/ sclerosing mesentritis should be considered [Fig.4,5]. On one year follow-up, his ultrasound whole abdomen done was within normal limit. Presently patient is totally asymptomatic and is on three monthly follow up.
Discussion
Very few cases of mesenteric panniculitis have been reported in the English literature under several names: retractile mesenteritis, sclerosing mesenteritis, liposclerotic mesenteritis etc [
5]. Incidence increases with age and pediatric cases are less, probably because of less mesenteric fat in children [
6]. This case is reported in view of its rarity in Indian scenario and because of chances of misdiagnosis.
Although various causal factors have been identified, the precise etiology remains unknown. More recent studies have shown a strong relationship between tobacco consumption and panniculitis [7]. In this case the patient was a chronic tobacco chewer and bidi smoker. Histologically, the disease progresses in three stages: mesenteric lipodystrophy, mesenteric panniculitis and finally retractile mesenteritis [6]. Here histopathology was of mesenteric panniculitis. Retractile mesenteritis has been associated with a number of malignant diseases such as lymphoma, melanoma, colon cancer, renal cell cancer, myeloma, and gastric carcinoma etc and may mimic these malignancies [
4,
6,
7].
The disease is often asymptomatic. When present, clinical symptoms may include anorexia, abdominal pain, abdominal fullness, nausea, pyrexia and weight loss [
8]. On occasions, the disease may also present with merely a single or multiple palpable masses. Here patient presented with a single large lump. Some reports even go as far as stating that few or none of the patients with mesenteric panniculitis can be diagnosed correctly before operation [
5]. However, with the advent of imaging technology like high-resolution CT or magnetic resonance imaging, distinguishing mesenteric panniculitis from other mesenteric diseases with similar imaging features such as carcinomatosis, carcinoid tumor, lymphoma, desmoids tumor seems possible and feasible [
9].
In this case CECT scan was not very conclusive and clinical presentation was in favor of non-Hodgkin lymphoma, though FNAC revealed features overlapping between reactive hyperplasia and NHL. Biopsy from the mass was advised but patient was very reluctant to any invasive procedure. As cases of abdominal lymphoma presenting in our out-patient department are not uncommon so this patient was considered a case of NHL.
Mesenteric panniculitis resolves spontaneously in most cases. In non-resolving lesions and symptomatic patients several types of treatment have been proposed. Therapy is individualized and may be attempted with a variety of drugs including steroids, thalidomide, cyclophosphamide, progesterone, colchicine, azathioprine, tamoxifen, antibiotics and emetine or radiotherapy with different degrees of success [
10]. Surgery may be attempted if medical therapy fails or in the presence of complications such as bowel obstruction or perforation. Patient showed good response with CHOP regimen, this may be due to response with prednisolone and cyclophosphamide as panniculitis also responds to these agents. Mesenteric panniculitis is a rare clinical entity that occurs independently or in association with other disorders including malignancy. In most of the cases high resolution CT scan is diagnostic. Open biopsy is required in those cases where CT scan is not conclusive.
Conclusion
We recommend that when a patient of mesenteric mass presents to oncology OPD and CT scan is not very decisive then open biopsy is mandatory. If biopsy is not feasible and such a patient did not get complete response with chemotherapy then possibility of mesenteric panniculitis should be kept in mind.
Contributors: SG: manuscript writing, literature search, patient management; PA: manuscript editing, literature search, histopathology; SP, AS: manuscript editing, patient management. SG will act as guarantor. All authors approved the final version of the manuscript.
Funding: None; Competing interests: None stated.
References
- Issa I, Baydoun H. Mesenteric panniculitis: various presentations and treatment regimens. World J Gastroenterol. 2009;15:3827-3830.
- Kipfer RE, Moertel CG, Dahlin DC. Mesenteric lipodystrophy. Ann Intern Med. 1974; 80:583-588.
- Emory TS, Monihan JM, Carr NJ, Sobin LH. Sclerosing mesenteritis, mesenteric panniculitis and mesenteric lipodystrophy: a single entity? Am J Surg Pathol. 1997;21:392-398.
- Akram S, Pardi DS, Schaffner JA, Smyrk TC. Sclerosing mesenteritis: clinical features, treatment, and outcome in ninety-two patients. Clin Gastroenterol Hepatol. 2007;5:589-596.
- Grieser C, Denecke T, Langrehr J, Hamm B, Hanninen EL. Sclerosing mesenteritis as a rare cause of upper abdominal pain and digestive disorders. Acta Radiol. 2008;13:1-3.
- Delgado Plasencia L, Rodríguez Ballester L, Lopez-Tomassetti Fernández EM, et al. Mesenteric panniculitis: experience in our center. Rev Esp Enferm Dig. 2007;99:291-297.
- Daskalogiannaki M, Voloudaki A, Prassopoulos P, Magkanas E, Stefanaki K, Apostolaki E, et al. CT evaluation of mesenteric panniculitis: prevalence and associated diseases. Am J Roentgenol. 2000;174:427-431.
- Shah AN, You CH. Mesenteric lipodystrophy presenting as an acute abdomen. South Med J. 1982;75:1025-1026.
- Pickhardt PJ, Bhalla S. Unusual nonneoplastic peritoneal and sub-peritoneal conditions: CT findings. Radiographics. 2005;25:719-730.
- Mazure R, Fernandez Marty P, Niveloni S, Pedreira S, Vazquez H, Smecuol E, et al. Successful treatment of retractile mesenteritis with oral progesterone. Gastroenterology. 1998;114:1313-1317.