|
|
|
|
|
Arthroscopic Reduction and Internal Fixation of Humeral Head Osteo-chondral Fracture
|
|
|
|
Efi Kazum, Ofir Chechik, Noam Rosen, Oleg Dolkart, Yariv Goldstein, Eran Maman Shoulder Surgery Unit, Orthopedic Division, Tel Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel Aviv, Israel. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Efi Kazum Email: efikazum@gmail.com |
|
|
|
|
|
|
|
|
Received:
23-MAY-2017 |
Accepted:
20-SEP-2017 |
Published Online:
05-NOV-2017 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: We present what we believe to be the first description of an arthroscopically assisted approach to treat a patient with an osteo-chondral fracture associated with anterior labral lesion after a traumatic shoulder dislocation from a fall during snow-boarding. Case Report: We used a SmartNail® for the fixation of the osteo-chondral fragment, followed by an arthroscopic anterior labrum repair with Lupine® suture anchors. The procedure is presented in a video. Conclusion: Arthroscopically aided reduction and internal fixation can be considered as a possible treatment of osteo-chondral shoulder fracture. |
|
|
|
|
|
Keywords :
|
Accidental Falls, Arthroscopy, Joint Diseases, Rotation, Shoulder Dislocation.
|
|
|
|
|
|
|
|
|
|
|
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa4291d0000005707000001000200 6go6ckt5b5idvals|801 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Young and active individuals, especially skiers, suffer a variety of upper extremity injuries, among them joint dislocation and bone fractures. A gleno-humeral dislocation is the most common dislocation in skiing as well as in snowboarding [ 1]. The proximal humerus fractures constitute 3.3% and humeral head fractures constituted 1% of shoulder injuries [ 2]. Late complications of proximal humerus fractures, such as mal-union, avascular necrosis, or non-union, are frequent and often lead to articular incongruence that results in considerable pain, stiffness, and functional impairment [ 3, 4].
Fixation of intra-articular osteo-chondral fragments is technically challenging, and few instruments and implants are available for their treatment [ 5]. These types of injuries should be addressed as early as possible with the goal of restoring the anatomy and mobility of the joint. SmartNail ® (Conmed, Utica, NY) is a bio-resorbable nail made of bioglass, which is a biodegradable material that does not require subsequent removal [ 6]. This nail is highly suitable for fixation of osteo-chondral fragments. Case Report
A 26-year-old generally healthy male presented to the emergency department one day after sustaining a direct blow to his left shoulder as a result of a fall while snow-boarding. He reported immediate pain and limitation of movement, and was referred to a local clinic at the ski slope site where he was diagnosed with a proximal humeral head fracture.
Physical examination revealed pain, swelling and hematoma over his left shoulder, as well as severe limitation of shoulder range of motion (ROM) in all directions. No damage to nerves or blood vessels was found. Antero-posterior and lateral images on radiologic examination of the left shoulder demonstrated a bony fragment displaced medially and inferiorly [Fig.1]. Non-contrast computed tomography demonstrated a fracture of the articular posterior part of the proximal humeral head. The fragment measured 2.5 × 2 cm and involved more than 40% of the humeral head [Fig.2-4] which was displaced inferiorly and medially. According to the Flatow and Warner classification system, the related Hill Sachs lesion was classified as “significant” [ 7]. The patient was treated with arthroscopically aided reduction and internal fixation by means of a SmartNail ®, followed by an arthroscopic anterior labrum repair using Lupine ® suture anchors (J&J, Raynham, MA). The procedure is presented in Video 1. This is video of the first diagnostic arthroscopy (fragment reduction and repair, and anterior Bankart repair) and the second arthroscopy (adhesion release demonstrating fragment incorporation).
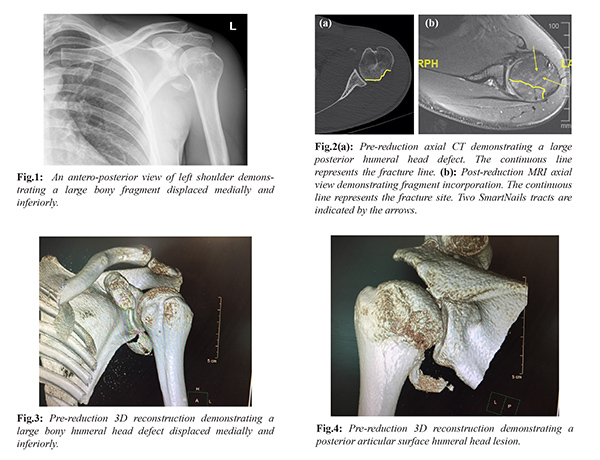
The patient was then immobilized in a sling for 6 weeks, followed by physiotherapy and hydrotherapy. He continued to have persistent joint stiffness despite vigorous physical therapy throughout follow-up. A magnetic resonance imaging study demonstrated incorporation of the fragment and articular surface congruency without step or gap [Fig.2b]. Due to the shoulder joint stiffness and limited ROM, a second arthroscopic procedure was performed one year following the first surgery. Intra-operative findings revealed a stable and fully united osteo-chondral fragment to the humeral head. Debridement and release of adhesions were performed, resulting in partial improvement in shoulder ROM.
At the final follow-up visit, 3 months after the second surgery, active ROM was 120º abduction, forward flexion 110º, external rotation 30º, and internal rotation at the level of L3 vertebrae.
Discussion
We describe a patient with an anterior shoulder dislocation with spontaneous reduction that had resulted in a large displaced osteo-chondral fracture of the posterior articular surface of the humeral head and an anterior labral tear. Surgical treatment was preferred over conservative management due to the large size of the fragment and the extent of the displacement. The specific indications for surgery in this case were damage to articular congruency with the likely development of post-traumatic arthritis [ 3, 4], as well as the high likelihood of recurrent instability [ 7]. While the treatment for gleno-humeral instability is a relatively straightforward labral repair [ 8], the treatment for humeral head defects is more complex and depends upon the size of the lesion.
Humeral head defects that account for 25% or less of the humeral head diameter will be best treated with “Remplissage” [ 9]. Treatment of a humeral defect that exceeds 40% of the humeral head diameter can be provided by the following options: open reduction internal fixation (ORIF) of the fragment, allograft transplantation, mosaicplasty, Latarjet procedure, and our currently presented arthroscopically aided reduction and internal fixation of the fragment.
Fandridis et al. described a shearing-type osteo-chondral humeral head fracture following a traumatic posterior shoulder subluxation in a 26-year-old male [ 10]. Since the osteo-chondral fragment had been sheared off the antero-medial aspect of the humeral head, it was easily approachable by an open delto-pectoral approach. The fragment was reduced and fixed into place with 2 headless screws. At one year post-operatively, there was no difference between the ROMs of the 2 shoulders, and the radiologic workup showed full fragment integration without any absorption or necrosis.
The use of osteo-chondral allografts has been proposed to address moderate-to-large humeral-sided defects (more than 40% of the articular surface). This type of humeral head augmentation aims to restore the native anatomy of the humeral head. Saltzman et al. [ 11] described improved shoulder ROM, improved functional outcome scores, and decreased subsequent dislocation rates when using osteo-chondral allografts for humeral head defects. They used a variety of graft types, including fresh-frozen humeral and femoral head allografts, fresh humeral head allografts, and osteo-articular plugs. The complication rate ranged between 20% to 30%, and the reoperation rate was 26%. At the end of the 5 or more years of follow-up, 50% of the patients required conversion to a total shoulder arthroplasty [ 11].
Osteo-chondral transplant techniques require the transfer of small bone plugs covered with normal hyaline articular cartilage to the location of chondral defects, which then heal to the surrounding recipient tissue [ 12]. Nam et al. described two cases of chondral defects of the femoral head resulting from traumatic hip dislocation that were treated with osteochondral autografts from the ipsilateral knee and the inferior femoral head. At one and 5-year follow-ups, the magnetic resonance imaging studies showed good autograft incorporation and maintenance of articular surface congruity. Both patients were pain-free, they had full ROM of their hips, and they were able to ambulate without assistance [ 13]. Given the similarities between the humeral and hip joints, mosaicplasty could be considered as an option in cases of large humeral defects.
Snir et al. [ 14] (described an arthroscopic approach using cylindrical osteo-chondral allograft plug transplantation without fixation for the treatment of large Hill-Sachs defects. That technique is free of the drawbacks encountered when performing the open approach, including soft-tissue trauma, neurovascular injury, avascular necrosis and hardware complications [ 15]. It is a minimally invasive approach that allows close approximation of the plugs and restorations of the humeral head contour. However, potential complications, such as graft reabsorption, graft failure, and cyst development, were described, as was the risk of disease transmission [ 16].
The Remplissage procedure consists of infraspinatus tenodesis and posterior capsulodesis to fill the humeral head lesion in addition to Bankart repair. The Latarjet operation employs a triple blocking mechanism, including lengthening the glenoid arc by adding a coracoid graft to the anterior glenoid rim. In 2000, Burkhart and De Beer reported a recurrence rate of 4% after arthroscopic Bankart repair for patients with anterior instability and no significant bone deficiency. However, the recurrence rate in the presence of a gleno-humeral bony deficiency was 67% [ 17]. Cho et al. [ 18] reported the clinical outcomes and post-operative complications of 37 patients that were treated arthroscopically with Remplissage and Bankart repair to 35 Latarjet procedures indicated for anterior shoulder instability with a large engaging Hill–Sachs lesion and without significant glenoid bone loss (glenoid deficit less than 25%). The total recurrence rate was 5.4% in the Remplissage group and 5.7% in the Latarjet group. 14.3 % of the patients in the Latarjet group suffered from complications, while no complications were reported in the Remplissage group. Motion was limited in approximately 10° in external rotation in both the Remplissage and Latarjet groups and internal rotation was at the 1.9 level in the Latarjet group. An increase in muscle strength was seen in both groups. Those authors noted that resection of the fragment would have left a large defect in the humeral head, and that the defect would have most likely ended in chronic instability.
The present report describes a case of a non-bony labral lesion with a significant humeral head defect. After reviewing the existing literature, the treatment goals were set to reconstruct the articular surface as anatomically as possible and to provide an effective solution for the shoulder instability. We decided to carry out arthroscopically assisted reduction and internal fixation of the osteo-chondral lesion together with Bankart lesion over the presented alternatives. Shoulder arthroscopy, as a minimal invasive procedure, has the advantages of minimal soft tissue morbidity, no need for joint dislocation and minimal blood loss. Furthermore, early joint mobilization and rehabilitation are carried out post-operatively.
The late complications that could be expected over time are reduced ROM and pain, back-out and breakage of the smart nail, nonunion of the reduced fragment, synovitis and osteolytic lesions as a result of inflammatory response to the implant [ 9, 19]. One year of follow-up of our patient is too short to conclude that the he was spared from experiencing the mentioned complications.
Conclusion
To our knowledge, this is the first description of an arthroscopically assisted treatment for an osteo-chondral fracture associated with anterior labral lesion after a traumatic shoulder dislocation.
Acknowledgment: Esther Eshkol is thanked for editorial assistance. Contributors: EK, OC: manuscript writing, patient management; NR, OD, YG, EM: manuscript editing, critical inputs into the manuscript, patient management. KL will act as guarantor. All authors approved the final version of the manuscript. Funding: None; Competing interests: None stated.
References - Johnson RJ, Pope MH. Epidemiology and prevention of skiing injuries. Ann Chir Gynaecol. 1991;80:110-115.
- Kocher MS, Feagin JA, Jr. Shoulder injuries during alpine skiing. Am J Sports Med. 1996;24:665-669.
- Boileau P, Trojani C, Walch G, Krishnan SG, Romeo A, Sinnerton R. Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elbow Surg. 2001;10:299-308.
- Mansat P, Bonnevialle N. Treatment of fracture sequelae of the proximal humerus: anatomical vs reverse shoulder prosthesis. Int Orthop. 2015;39:349-354.
- Gupta AK, McCormick FM, Abrams GD, Harris JD, Bach BR, Jr., Romeo AA, et al. Arthroscopic bony bankart fixation using a modified sugaya technique. Arthrosc Tech. 2013;2:e251-255.
- Weckstrom M, Parviainen M, Kiuru MJ, Mattila VM, Pihlajamaki HK. Comparison of bioabsorbable pins and nails in the fixation of adult osteochondritis dissecans fragments of the knee: an outcome of 30 knees. Am J Sports Med. 2007;35:1467-476.
- Flatow EL, Warner JI. Instability of the shoulder: complex problems and failed repairs: Part I. Relevant biomechanics, multidirectional instability, and severe glenoid loss. Instructional Course Lectures. 1998;47:97-112.
- Levy DM, Cole BJ, Bach BR, Jr. History of surgical intervention of anterior shoulder instability. J Shoulder Elbow Surg. 2016;25:e139-50.
- Longo UG, Loppini M, Rizzello G, Ciuffreda M, Berton A, Maffulli N, et al. Remplissage, humeral osteochondral grafts, weber osteotomy, and shoulder arthroplasty for the management of humeral bone defects in shoulder instability: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30:1650-1666.
- Fandridis E, Stavropoulos S, Dimou L, Spyridonos S. Osteochondral humeral head fracture after posterior shoulder subluxation: A case report. Int J Shoulder Surg. 2014;8:55-57.
- Saltzman BM, Riboh JC, Cole BJ, Yanke AB. Humeral head reconstruction with osteochondral allograft transplantation. Arthroscopy. 2015;31:1827-1834.
- Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, et al. Autologous osteochondral grafting-technique and long-term results. Injury. 2008;39 Suppl 1:S32-39.
- Banz VM, Jakob SM, Inderbitzin D. Review article: improving outcome after major surgery: pathophysiological considerations. Anesth Analg. 2011;112:1147-1155.
- Roghani R, Snir N, Wolfson TS, Rokito AJ. The Importance of tear edge fixation in modified transosseous-equivalent rotator cuff repair A biomechanical study. Bull Hosp Jt Dis. 2013;73:10-17.
- Snir N, Hamula M, Wolfson T, Meislin R, Strauss EJ, Jazrawi LM. Clinical outcomes after chronic distal biceps reconstruction with allografts. Am J Sports Med. 2013;41:2288-2295.
- Lynch JR, Clinton JM, Dewing CB, Warme WJ, Matsen FA, 3rd. Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elbow Surg. 2009;18:317-328.
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677-694.
- Cho NS, Yoo JH, Rhee YG. Management of an engaging Hill-Sachs lesion: arthroscopic remplissage with Bankart repair versus Latarjet procedure. Knee Surg Sports Traumatol Arthrosc. 2016;24:3793-3800.
- Dines JS, Fealy S, Potter HG, Warren RF. Outcomes of osteochondral lesions of the knee repaired with a bioabsorbable device. Arthroscopy. 2008;24:62-68.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Kazum E, Chechik O, Rosen N, Dolkart O, Goldstein Y, Maman EArthroscopic Reduction and Internal Fixation of Humeral Head Osteo-chondral Fracture.JCR 2017;7:355-359 |
|
Kazum E, Chechik O, Rosen N, Dolkart O, Goldstein Y, Maman EArthroscopic Reduction and Internal Fixation of Humeral Head Osteo-chondral Fracture.JCR [serial online] 2017[cited 2025 Sep 8];7:355-359. Available from: http://www.casereports.in/articles/7/4/Arthroscopic-Reduction-and-Internal-Fixation-of-Humeral-Head-Osteo-chondral-Fracture.html |

|
|
|
|
|