6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe4421e0000000c02000001000200
6go6ckt5b5idvals|810
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Asystole is a state of no cardiac activity and is eventually recorded in all dying patients. The immediate diagnosis of asystole requires the recognition of cardiac arrest and a confirmed flat line rhythm, in two perpendicular leads. Patient may complain of lightheadedness or syncope if asystole is preceded by brady-asystolic rhythm. Asystole is associated with a poor outcome, regardless of its initial cause. Resuscitation is likely to be successful only if it is secondary to a correctable event, such as a cardiac arrest due to a cafe coronary (fatal food asphyxia). The incidence of asystole is reported to be similar in males and females; however, the frequency of cardiac arrest is proportional to the underlying incidence of heart disease, which is more common in males until age 75. The prevalence of asystole as the presenting cardiac rhythm is lower in adults (25%-56%) than children (90%-95) [
1-
3]. Pulseless electrical activity (PEA) is the term applied to a heterogeneous group of dysrhythmias accompanied by an undetectable pulse.
Herein we present a case of cardiac arrest (primary asystole) who recovered after prolonged cardio-pulmonary resuscitation and was successfully discharged after permanent pacemaker implantation.
Case Report
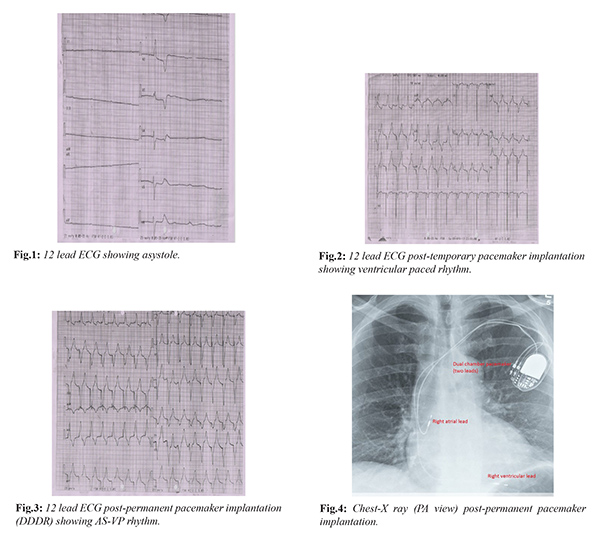
A 55 years old female presented to casualty with an episode of seizure (lasted ~5 min) followed by unconsciousness. On initial examination pulse and BP was not recordable and outside electrocardiogram (ECG) (done 15 min prior to arriving in accident and emergency) showed asystole [Fig.1]. Hence, cardio-pulmonary resuscitation (CPR) was started immediately as per advanced cardiac life support (ACLS) guidelines and endo-tracheal intubation was done. Old records of patient revealed dilated cardiomyopathy with reduced ejection fraction (38%) and documented complete heart block (CHB). Inspite of prolonged CPR and repeated injections of atropine and adrenaline rhythm could not be restored. Patient was shifted to cathlab with continued CPR and temporary pacemaker implantation was done [Fig.2]. Patient was shifted to coronary care unit (CCU) with inotropes, temporary pacemaker implantation and was placed on ventilator. Poor neurologic and cardiac recovery was explained to relatives accordingly. But, to our surprise patient became responsive after 12 hours of treatment and was successfully extubated by intensivist. Patient continued to be pacemaker dependent and her coronary angiography showed normal coronaries. She was taken for permanent pacemaker implantation (DDDR) on second day and was accomplished successfully [Fig.3,4]. Patient was discharged in hemodynamically stable condition and followed up in out-patient department after one month.
Discussion
Asystole also described as “flat-line” on ECG can be primary or secondary. Primary asystole results from failure of cardiac conduction system to reproduce ventricular depolarization. This may result from ischemia or from degeneration of the SA node or AV conducting system due to sclerosis. It is usually preceded by a brady-arrythmia, due to sinus arrest or complete heart block [
4].
Reflex asystole has been reported in various ocular surgeries, trauma or maneuvers involving vagal nerve stimulation. Asystole is also well documented in hypersensitive carotid sinus syndrome, or glossopharyngeal neuralgia. Brady-asystole is also documented in left temporal lobe complex partial seizures. Possibility of sudden cardiac death exists if asystole were to persist. The longest interval reported is 26 seconds [
5,
6].
Secondary asystole refers to failure of ventricular depolarization resulting from factors occurring outside of the heart's electrical conduction system. All these secondary factors attribute to severe tissue hypoxia with metabolic acidosis which culminates into asystole eg. suffocation, drowning, CVA (cerebro vascular accident), massive pulmonary embolism, hyperkalemia, myocardial infarction (MI) complicated by complex arrhythmias, post-defibrillation, and sedative-hypnotic or narcotic overdoses leading to respiratory failure [
7,
8].
Management of asystole includes early recognition and institution of CPR as per ACLS protocol. The only two drugs recommended by the American Heart Association are epinephrine and atropine. Inspite of full vagolytic doses of atropine (0.04 mg/kg) and high-dose epinephrine (0.20 mg/kg), few patients survive to leave the hospital neurologically intact.
Therapeutic hypothermia (TH) is usually indicated as a neuro-protective therapy in adult post-cardiac arrest victims whose initial cardiac rhythm is [ventricular fibrillation (VF)/ventricular tachycardia (VT)] and who remain comatose (GCS< 8) after ROSC – return of spontaneous circulation (class I; Level B), whereas the evidence of its effectiveness after asystole or PEA is doubtful (class IIb; level C). A study published in 2011 to study role of TH in both shockable (VT/VF) and non-shockable rhythms (asystole/pulseless electric activity) concluded that TH was independently associated with an improved outcome at hospital discharge in patients presenting with VF/VT with no clear effectiveness in non-shockable rhythm [
9,
10].
In our case (primary asystole) timely institution of active CPR (as per ACLS guidelines) along with temporary pacemaker implantation helped in early recovery with intact neurological status of the patient.
Conclusion
Prognosis of asystole depends on the etiology (primary or secondary) of the asystolic rhythm and success or failure of CPR. Primary asystole may be prevented by the appropriate use of a temporary/permanent pacemaker in those patients who have high-grade heart block or sinus arrest.
Contributors: GM: manuscript writing, literature review, and patient management; APS: critical inputs into the manuscript, and patient management. GM will act as guarantor. Both authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- American Heart Association: American Heart Association Emergency Cardiac Care Committee and Subcommittees: Guidelines for cardiopulmonary resuscitation and emergency cardiac care. JAMA.1992;268:2171-2302.
- Perers E, Abrahamsson P, Bang A. There is a difference in characteristics and outcome between women and men who suffer out of hospital cardiac arrest. Resuscitation. 1999;40:133-140.
- Richman PB, Nashed AH. The etiology of cardiac arrest in children and young adults: special considerations for ED management. Am J Emerg Med. 1999; Pt - Review, Tutorial(3):264-270.
- Ornato JP, Peberdy MA. The mystery of bradyasystole during cardiac arrest. Annals of Emergency Medicine. 1966;27:576-587.
- Monnie GT, Rees DL, Elton D. The oculocardiac reflex during strabismus surgery. Canadian Anaesth Soc J. 1964;11:621-632.
- Gold RS, Pollard Z, Buchwald IP. Asystole due to the oculocardiac reflex during strabismus surgery: A report of two cases. Ann Ophthalmol. 1988;20:473-477.
- Niemann JT, Cairns CB. Hyperkalemia and ionized hypocalcemia during cardiac arrest and resuscitation: possible culprits for post countershock arrhythmias? Ann Emerg Med. 1999;34:1-7.
- Niemann JT, Cairns CB. Hyperkalemia and ionized hypocalcemia during cardiac arrest and resuscitation: possible culprits for postcountershock arrhythmias? Ann Emerg Med. 1999;34:1-7.
- Dumas F, Grimaldi D, Zuber B, Fichet J, Charpentier J, Pène F, et al. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients? Circulation. 2011;123:877-886.
- Mallick PN, Upadhyay SP, Singh RKA, Singh SK. Two cases of asystolic cardiac arrests managed with therapeutic hypothermia. Indian J Crit Care Med. 2013;17:113-115.