6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa494200000001707000001000400
6go6ckt5b5idvals|839
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Despite the rare occurrence of hyper-natremic dehydration in neonates, number of cases have been reported with fatal outcome. There is no consensus so far on patho-physiology of this condition but early postpartum discharge with lack of knowledge about techniques and adequacy of breast feeding in mothers has been proposed as a major risk factor [1]. An early diagnosis is absolutely warranted in this clinical condition as delay may result in irreversible neuronal insult [2].
Case Report
A 35 years old second gravida delivered 40 week male neonate with birth weight of 3 kg by emergency cesarean section in view of meconium stained liquor. Baby cried after birth with uneventful post-natal period and was discharged on day five of life on exclusive breast feeding. On day 13 of life, baby was brought to the hospital with history of poor feeding, lethargy and decrease urine output of one day duration.
Baby was on exclusive breast feeds with no history of diarrhea or vomiting. Physical examination was suggestive of a sick looking neonate with irritability and moaning sounds. Baby looked emaciated with weight of 2.1 kg (significant weight loss of 30% since birth). His heart rate was 160/min with poorly felt peripheral pulses and prolonged capillary refill time (>3 sec). Axillary temperature was 97.2ºF with respiratory rate of 43/min. Neurological examination revealed moaning sounds, hypotonia with poorly elicitable neonatal reflexes. The baby was admitted in neonatal intensive care unit with strong clinical suspicion of sepsis with features of hypovolemia. Baby didn’t have any history of seizures.
Sepsis screen showed CRP (C-reactive protein) negative, hemoglobin: 15.3 g/dL, total leukocyte count: 10,200/mm3 (polymorphs 41%, lymphocytes 52%), platelets 2,10,000/mm3 and blood sugar 89 mg/dL. Blood urea and creatinine were 200 mg/dL and 2.8 mg/dL respectively at the time of admission. Serum electrolytes were deranged with sodium 178 mg/dL and potassium of 5.7 mg/dL. Arterial blood gas analysis was normal. Subsequently CSF analysis, blood and urine cultures were negative. Trans-cranial ultrasound ruled out any intra-cranial bleed. Baby was initially managed with two normal saline boluses of 20 ml/kg each to correct the hydration status. Thereafter, half normal saline (N/2) was infused followed by N/3 normal saline with 5% dextrose to correct hypo-volemia and hyper-natremia. Prophylactic intravenous antibiotics (cefotaxime plus amikacin) were stopped after three days as the culture results were negative. Baby showed marked recovery over five days of hospitalization with normalization of renal parameters and serum sodium [Table 1].
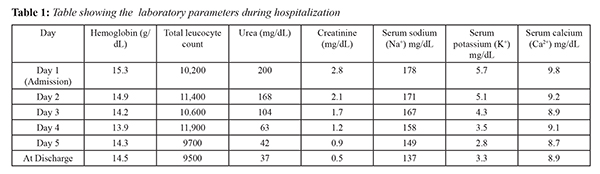
Baby was started on breast feeds with intermittent formula feeds on 5th day and discharged on 10th day of admission. Due to lack of resources, breast milk sodium could not be estimated. At the time of discharge it was ensured that mother was aware of correct breast feeding practices and to monitor the weight gain of the infant. On subsequent follow up neonate had normal renal parameters and developmental milestones.
Discussion
Exclusive breast feeding is strongly recommended to reduce neonatal morbidity and mortality in developing countries like India, but clinicians do encounter neonates with hyper-natremic
dehydration in their practice [3,4]. In elderly primigravida who are unaware of correct breastfeeding practices and reluctant to give formula feeds, the risk of developing hyper-natremic dehydration increases manifold [5]. In our case although mother was second gravida, she was very reluctant to give formula feeds to the baby at home despite noticing inadequate breast milk production and poor weight gain of the baby, clearly emphasizing the lack of knowledge about adequacy of breast feeding. A normal term neonate usually looses about 7-10% of birth weight and regains birth weight by day ten of life. Any loss of weight more than 10% is a matter of concern. In our case baby lost about 30% of birth weight despite exclusive breastfeeding.
The etio-pathogenesis of hyper-natremic dehydration in neonates is not exactly clear but most accepted explanation is that because of poor breastfeeding practices, the baby gets less volume of milk resulting in dehydration. In our case despite exclusive breast feeding, baby developed hyper-natremia and dehydration. We could not measure the breast milk sodium levels because of lack of good lab support. As also noticed in our case, the clinical presentation of these babies is usually between first to third week of life with severe dehydration and lethargy [3,4]. Other differential diagnosis like sepsis, meningitis and intra-cranial pathologies should also be ruled out before making a diagnosis of hyper-natremic dehydration.
The management protocol in hyper-natremic dehydration is to correct hypovolemic shock initially with ringer lactate or normal saline boluses and then to gradually bring down serum sodium by 10-15 mEq/litre/day, as sudden decrease can result in neuronal damage [6]. We used half normal saline (N/2) initially followed by N/3 saline in 5% dextrose as maintenance fluid. After initial fluid management babies can be restarted on breast feeds contrary to the belief that breast milk is contraindicated and formula feeds should be used [7]. We also tried to put baby on breast feeds but because of inadequacy of mother`s milk formula feeds were given.
With a trend of early postpartum discharges, it is the duty of medical and paramedical staff to ensure that the mothers have been properly sensitized about adequacy of breast feeding and to monitor weight gain of neonates after discharge. Mothers, relatives and health care professionals must be explained that if a neonate has weight loss of more than 10% since birth and not gaining weight despite exclusive breast feeding, they should immediately report to the health care facility [8]. The patients who requires special attention are primigravida mothers with breast feeding difficulties (improper positioning or latching), breast engorgement, flat or inverted nipples.
Conclusion
Early post-partum follow up and lactation counseling in these mothers can be a useful tool to identify the neonates at high risk of developing this entity. There is an urgent need to foster a greater awareness of this problem among lactating mothers and health care professional to prevent disastrous complications.
Contributors: PH: manuscript writing, patient management; AD: manuscript editing, patient management. PH will act as guarantor. Both authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References:
- Lock M, Ray JG. Higher neonatal morbidity after routine early hospital discharge: Are we sending newborns home too early? CMAJ. 1999;161:249-253.
- Gussler JD, Briesemeister LH. The insufficient milk syndrome: A bicultural explanation. Med Anthropol. 1980;4:145-174.
- Sofer S, Benezer D, Dagan R. Early severe dehydration in young breastfed newborn infants. Isr J Med Sci. 1993;29:85-89.
- Kini N, Zahn S, Werlin SL. Hypernatremic dehydration in breast fed infants. Wis Med J. 1995;94:143-145.
- Roddy OF, Martin ES, Swetenburg RL. Critical weight loss and malnutrition in breastfed infants. Am J Dis Child. 1981;135:597-599.
- Conley SB. Hypernatremia. Pediatr Clin North Am. 1990;37:365-372.
- Bajpai A, Aggarwal R, Deorari AK, Paul VK. Neonatal hypernatremia due to high breast milk sodium. Indian Pediatr. 2002;39:193-196.
- Laing IA, Wong CM. Hypernatremia in the first few days: Is the incidence rising? Arch Dis Child Fetal Neonatal Ed. 2002;87:158-162.