6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64f81f0000008402000001001300
6go6ckt5b5idvals|830
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Secondary hyper-parathyroidism is the over-production of parathyroid hormone secondary to a chronic abnormal stimulus for its production. Typically, this is due to chronic renal failure [
1]. Another common cause is vitamin D deficiency which is usually under-diagnosed. Virtually all patients with renal failure have hyper-parathyroidism to some degree and their clinical presentation is often that of renal failure. In patients with secondary hyper-parathyroidism due to vitamin D deficiency, the symptoms are mainly myopathy, bone pain and the patients may have increased risks of fractures. Pathological fractures due to secondary hyper-parathyroidism are uncommon. Here we report a case of seizures and severe shock presenting to the Emergency Department (ED) and diagnosed with pathological fractures and secondary hyper-parathyroidism.
Case Report
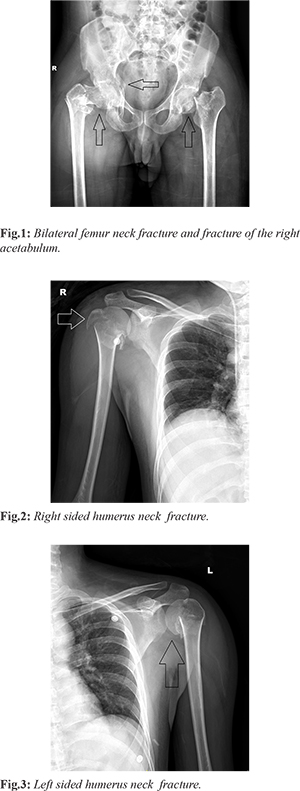
A 27 year old blind male with no known previous co-morbidities was brought to the ED with history of uneasiness, breathing difficulty and generalized bodyache since six hours before arrival. Patient had a history of seizures and fall on the same morning for which he was investigated in another hospital and was neurologically evaluated. He underwent Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) of the brain which were both normal. On examination patient had a heart rate of 124/minute, blood pressure was not recordable, respiratory rate of 33/minute, and SpO2 of 100% on room air. On systemic examination he was conscious, oriented with no focal neurological deficit, pallor was present, small hematoma over the right arm, chest was clear with no added sounds and rest of the systemic examination was unremarkable. He was started with aggressive fluid resuscitation, broad spectrum antibiotics and anti-convulsants. Patient was not fluid responsive and was subsequently started on inotropes. Initial blood gas analysis revealed severe metabolic acidosis with a pH of 6.930, bicarbonate of 9.2 meq/L and lactates of 14. His initial blood work showed a hemoglobin of 7.4 g/dL, total leucocyte count of 15,200/mm3, procalcitonin level of 23.9 ng/mL, urea of 41.2 mg/dL, creatinine of 1.9 mg/dL and creatine phosphokinase of 4996 IU/L. Patient was provisionally diagnosed as septic shock with suspected rhabdomyolysis (secondary to seizures) and shifted to the Intensive Care Unit (ICU) for further management. On the 3rd day in ICU, the patient complained of severe joint pains for which X-rays were done. The X-rays revealed the patient to be having comminuted fracture of the right acetabulum, fracture of bilateral femoral necks with displaced bone fragments and comminuted fractures of bilateral neck of humerus [Fig.1-3]. In view of the X-ray findings, the patient’s vitamin levels were done which revealed vitamin D of 3.5 ng/mL, calcium levels of 4.8 mg/dL and serum parathyroid (PTH) level of 607.2 pg/mL. Patient was finally diagnosed as a case of hypo-vitaminosis D, secondary hyper-parathyroidism, hypocalcemia with bilateral pathological shoulder and femur fractures. He was started on parenteral vitamin D supplementation and underwent surgical fixation of the fractures. The patient was discharged in a stable condition on the 14th day with follow up advice.
Discussion
Vitamin D deficiency is common in elderly and children, especially in the housebound and geriatric patients [
2]. It can cause rickets in children, will precipitate and exacerbate osteopenia, osteoporosis, fracture in adults and is also associated with increased risk of common cancers, autoimmune diseases and infectious diseases. The synthesis of vitamin D in the skin under the influence of ultraviolet light decreases due to insufficient sunlight exposure and a decreased functional capacity of the skin [
2]. Diet low in calcium may cause an increased turnover of vitamin D metabolites and thereby aggravate vitamin D deficiency. The effect of vitamin D depletion in the pathogenesis of secondary hyper-parathyroidism in elderly individuals or in the occurrence of PTH hyperplasia in patients with renal insufficiency is well established. Deficiency of vitamin D causes secondary hyperparathyroidism via its essential action on parathyroid cells, inhibiting parathormone secretion and parathyroid cell proliferation, which can lead to high bone turnover, bone loss, mineralization defect and less commonly myopathy and falls [
3]. Down-regulation of parathyroid, vitamin D and calcium sensing receptors represent critical steps that lead to abnormalities in mineral metabolism; high phosphate, low calcium, and vitamin D deficiency. Disregulation of calcium and phosphate homeostasis leads to decreased renal phosphate excretion, increase serum phosphorus, elevated levels of phosphatonin, fibroblast growth factor 23 and reduced synthesis of calcitriol [
4]. These changes result in increase synthesis and secretion of parathyroid hormone and parathyroid hyperplasia, contributing to the development of vicious cycle [
3]. Osteitis fibrosis cystica is a high-turnover bone disease that stems from elevated PTH concentrations stimulating osteoclast activity, bone breakdown, and resorption. This can lead to subsequent bone pain and fractures [
5].
Conclusion
Though secondary hyperparathyroidism usually presents with joint pains and myopathies but in rare circumstances the patient may present with severe manifestations like seizures, shock and multiple pathological bone fractures. Therefore secondary hyper-parathyroidism can be kept in the differential diagnosis while managing such patients in the ED.
Contributors: VS: Manuscript editing, patient management; AV: manuscript writing, patient management; WRS,MH,SJ: critical inputs into the manuscript, patient management. VS will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Felsenfeld AJ. Considerations for the treatment of secondary hyperparathyroidism in renal failure. J Am Soc Nephrol. 1997;8:993-1004.
- Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocrine Reviews. 2001;22:477-501.
- Slatopolsky E, Brown A, Dusso A. Pathogenesis of secondary hyperparathyroidism. Kidney Intsuppl. 1999;73:s14-s19.
- Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011;6:913-921.
- Yuen NK, Ananthakrishnan S, Campbell MJ. Hyperparathyroidism of renal disease. Perm J. 2016;20:78-83.