6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa89a1f0000002d07000001000900
6go6ckt5b5idvals|827
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Gastrointestinal duplication cysts are a group of anomalies which are somewhat rare and may occur anywhere along the gastrointestinal tract from the mouth to the anus [1,2]. Clinical presentation varies depending on the location and morphologic structure of the duplication cyst. Radiologic imaging is informative when the diagnosis is entertained. Early surgical intervention in symptomatic cases has been known to yield favorable outcomes [3].
Case Report
A six month old female infant presented with a 10 day history of recurrent post-prandial vomiting which was not projectile and consisted of ingested breast milk. It however was noticed to be mildly bile stained occasionally. Vomiting bouts occurred on an average of two times a day over a four day period, after which symptoms abated only to resurface later. Similar symptoms, albeit few and far between dated back to six weeks prior to presentation. There was no significant change in bowel habits.
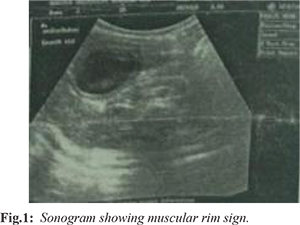
General examination findings were unremarkable except that she was moderately dehydrated. Abdominal palpation revealed an ovoid mass in the epigastric region to the right of the midline and a presumptive diagnosis of a hypertrophic pyloric stenosis was made. Hematological and biochemical investigations were normal. Abdominal ultrasonography revealed a large anechoic cystic mass which appeared to be abutting on the second part of the duodenum, impeding free flow of its contents. The cyst demonstrated the “muscular rim” sign – an echogenic serosa, hypo-echoic muscular layer and echogenic mucosa. A normal pyloric canal was noted [Fig.1]. A radiologic diagnosis of a duodenal duplication cyst was made and the patient was optimized for laparotomy.
Intra-operatively, a cystic, non-communicating gastric duplication, measuring 10×8 cm, attached to the distal third of the greater curvature of the stomach was found [Fig.2]. It contained slimy, clear fluid. No other associated anomaly was seen and complete excision of the cyst was achieved. Histopathology revealed an oval lesion with a unilocular cavity, lined with small intestinal mucosa. There were areas of hypertrophied muscular layer and no focus of atypia or malignancy [Fig.3,4]. The post-operative period was uneventful, oral feeds were commenced on the fourth day after surgery. She remained asymptomatic at two years post-operatively.
Discussion
Gastric duplication cysts (GDC) are one of the rare manifestations of gastrointestinal duplications, accounting for about 2-9% of cases [3-5]. About 75% of gastrointestinal duplications are said to be intra-abdominal and half of these are ileal duplications. In a series reported by Abdurahman et al. GDC were not encountered [6]. Varying degrees of gastric outlet obstruction, like in the index case, is one of the modes of presentation of GDC. This is similar to one of the cases of gastric duplications reported by Adejuyigbe et al. though in a 13 year old male [1] as well as that of a 10 month old female who in addition to vomiting had an abdominal mass as a presenting symptom [3]. A palpable abdominal mass was not noticed prior to presentation in our patient. Other documented presentations include gastrointestinal bleeding and abdominal pain [1,4]. Respiratory obstruction with associated difficulty in feeding is one of the less common presentations and is seen in sublingual gastric duplication cysts [7]. A high index of suspicion and appropriate radiologic imaging is helpful in making a diagnosis. Recurrent post-prandial emesis raised a suspicion of gastric outlet obstruction in the index case. The palpable epigastric mass further reinforced this suspicion necessitating relevant investigation.
Abdominal ultrasonography is one of the imaging modalities used in the diagnosis of duplication cysts. While various sonographic appearances have been ascribed to duplication cysts, however, the muscular rim sign (the 2 layer pattern), when seen is considered by some, as the most reliable indication of a duplication cyst [8]. It has been suggested that no further imaging modality is necessary after this [2]. In experienced hands, an abdominal ultrasound can indeed be reliable in diagnosing duplication cysts. In our case, a pre-operative diagnosis of a duodenal duplication informed a level of preparedness beyond what was eventually required bearing in mind the varied approaches to excision of a duodenal duplication without injury to the ampulla of Vater. Endoscopic ultrasonography has recently been employed in adult populations to make diagnosis of duplication cysts [5,9]. Some authors are of the opinion that a contrast enhanced Computer Tomography scan and endoscopic ultrasonography are the gold standard for the diagnosis of GDC [5]. While that is commendable, it may not find routine practical application in resource limited settings such as ours. The need for sedation in the children for these imaging modalities further limits its use.
Gastric duplication cysts, like duplications of other parts of the gastrointestinal tract may present during infancy or remain undiagnosed into adulthood. It has been reported that the majority of GDC, 67%, are diagnosed during the first year of life [9]. Those that are undiagnosed in this period are often encountered as incidental findings or intra-operatively in adults [9]. The presence of additional associated anomalies has been documented to occur in 35% to 50% of cases [4,5]. A coexisting mesenteric cyst in a 16 month old female and an absent upper left rectus abdominis in a 13 year old male were reported by Adejuyigbe et al [1]. Anomalies of the genitourinary system and vertebra have also been documented [4]. There was no associated anomaly noted in our case.
Complete excision remains the gold standard for treatment, especially in cystic, non-communicating GDC [3,4,10]. This was achieved in the index patient. Mucosal stripping may be employed if the common wall is contiguous, particularly in the tubular variety of duplications [1,4]. The future risk of malignancy reinforces the need for a complete excision.
Conclusion
Gastric duplication cysts, though a somewhat rare group of congenital anomalies, should be included in the list of differential diagnosis in infants presenting with symptoms of gastric outlet obstruction. Careful radiologic imaging should is encouraged to increase the yield of preoperative diagnosis. A high index of suspicion cannot be over-emphasized, given the varied modes of presentation.
Contributors: OCT, OF: Clinical diagnosis, patient management, manuscript editing; AOT: manuscript writing and editing; APA: critical inputs into the manuscript and imaging; MAA: critical inputs into the manuscript and histopathology. OCT will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Adejuyigbe O, Olayinka OS, Sowande OA, Abubakar AM. Gastrointestinal duplications in Ile-Ife, Nigeria. East Afr Med J. 2002;79:134-136.
- Deftereos S, Soultanidis H, Limas C, Tsalkidis A, Gouliamtzi E, Manavis J. Duodenal duplication. Is ultrasound appearance enough to confirm the diagnosis? Rom J Gastroenterol. 2004;13:345-347.
- Kumar KG. Gastric duplication cyst in an infant presenting with non-bilious vomiting. The Malaysian journal of medical sciences: MJMS. 2012;19:76-78.
- Halder P, Mandal KC, Debnath B, Mukhopadhyay M. Gastric Duplication Cyst in Children: A Case Report and Literature Review. SM J Pediatr Surg. 2016;2:1031.
- D’journo XB, Moutardier V, Turrini O, Guiramand J, Lelong B, Pesenti C, et al. Gastric duplication in an adult mimicking mucinous cystadenoma of the pancreas. Journal of Clinical Pathology. 2004;57:1215-1218.
- Olajide A-RL, Yisau AA, Abdulraseed NA, Kashim IOO, Olaniyi AJ, Morohunfade AOA. Gastrointestinal duplications: Experience in seven children and a review of the literature. Saudi Journal of Gastroenterology. 2010;16:105-109.
- Ameh EA, Jimoh AO, Rafindadi AH, Shehu SM. Sublingual gastric duplication cyst causing respiratory obstruction: Case report. East Afr Med J. 2000;77:394-395.
- Segal SR, Sherman NH, Rosenberg HK, Kirby CL, Caro PA, Bellah RD, et al. Ultrasonographic features of gastrointestinal duplications. J Ultrasound Med. 1994;13:863-870.
- Singh JP, Rajdeo H, Bhuta K, Savino JA. Gastric duplication cyst: two case reports and review of the literature. Case reports in Surgery. 2013;2013.
- Bidwell JK, Nelson A. Prenatal ultrasonic diagnosis of congenital duplication of the stomach. J Ultrasound Med. 1986;5:589-591.