6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff2450210000002607000001000400
6go6ckt5b5idvals|847
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Pulmonary edema is a life-threatening condition which results from a persistent imbalance between the forces that drive water into the air space in the alveoli and the physiologic mechanisms that remove it. Rapid ascent to altitudes greater than 2500 m in healthy individuals may lead to acute mountain sickness (AMS), high-altitude pulmonary edema (HAPE) or high altitude cerebral edema (HACE).
Case Report
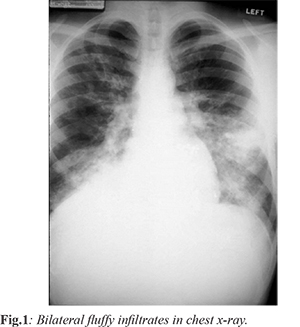
A 35 years old female who was a resident of Hyderabad (height - 505 m) was admitted in casualty with shortness of breath after one day stay at Shimla (height - 2276 m). Shortness of breath was insidious onset, gradually progressive to present even at rest and increased on lying down. This was associated with headache, dizziness, intermittent darkness in front of eyes and chest tightness. There was no history of paroxysmal nocturnal dyspnea, pedal edema, cough, sputum production, nausea, vomiting, fever or decreased urine output. She had upper respiratory tract infection before travel and was on 25 µg of thyroxine per day for hypothyroidism since last five years. On examination patient was cyanosed with blood pressure 160/100 mmHg; heart rate: 130/min; respiratory rate: 44/min; SpO2: 48% at room air; 65% on high flow oxygen. She was overweight with bilateral coarse crepitations and wheeze all over the chest. She was afebrile with normal jugular venous pressure. Rest all examination was normal. Her laboratory reports showed leucocyte count 17,200/L; hemoglobin 14.2 gm/dL; pH: 7.377; paO2: 35.6 mmHg; pCO2: 26.9 mmHg; HCO3: 15.4 mmol/L. Her chest X-ray view showed fluffy shadows in bilateral lung fields with no increased cardiac shadow whereas ECG was normal. Initially she was managed with 60% O2 inhalation at rate of 6L/min in propped up position, injection furosemide 40 mg intravenous repeated after 30 minutes, and urinary catheterization. Her SpO2 increased to 84%; HR: 108/min; BP: 130/80 mmHg. She was shifted to intensive care unit immediately. She was put on bilevel positive airway pressure (bipap) with pressure support of 12 cm H2O and ePAP of 6 cm H2O. She was administered injection morphine, furosemide (if SBP> 100 mmHg), injection dexamethasone , tablet nifedipine. Arterial blood analysis after 6 hours: pH: 7.398; paO2: 52.1 mmHg; pCO2: 38.3 mmHg; HCO3: 23.1 mmol/L. Differential diagnosis for this case were complicated: lower respiratory tract infection, cardiogenic pulmonary edema, high altitude pulmonary edema (HAPE). The patient being overweight, the diagnosis of obstructive sleep apnoea was also considered. However, paCO2 levels were not less than normal, hence obstruction was ruled out. Since she had sudden onset illness with normal ECG and was afebrile, we decided to treat her in the lines of HAPE. Patient was referred to a hospital in the plains to facilitate descent to a lower altitude with SpO2: 92%; BP: 130/70 mmHg; HR: 102/min and chest with decreased crepitations bilaterally. The patient was doing well and maintaining saturation at the hospital and was discharged after being kept under observation for three days.
Discussion
High altitude pulmonary edema is a non-cardiogenic pulmonary edema occurring mainly in low-landers with rapid ascent above 2500-3000 m (rarely below 2500m) in absence of acclimatization. Usually occurs within 2-4 days of ascent [1,2], it rarely occurs after more than 4 or 5 days at the same altitude, most likely because of remodelling and adaptation [3]. The first modern English language report of HAPE, was published by Houston was in 1960 [4]. First case was reported in the Rocky mountains. Prevalence of this in Rocky Mountains is 0.01- 0.1%, Greater Alpines: < 0.2%, Himalayas & Alps: 4%. A study conducted on 52 patients admitted to a hospital between 1992 and 2000 in the French Alps reported HAPE at moderate altitudes of between 1,400-2,400 m, though the incidence of HAPE at these altitudes is considered rare.
HAPE is commonly found to develop in association with AMS. Early symptoms include non-productive cough, dyspnea on exertion, reduced exercise performance. Later on there may be worsening of cough, breathlessness at rest or orthopnea. In advanced form there may be pink frothy sputum. There may be associated cyanosis, tachycardia, tachypnea, raised body temperature < 38.5º C, rales (typically in middle zone). Chest X-ray may show patchy opacities (often in right middle lobe). Ultrasound may show “Comet tail” pattern.
Prevention is best by slow ascent [6]. Other methods are acetazolamide [7] (125 mg 12 hourly starting as soon as possible, but not >5 days prior to ascent), nifedipine (an inhibitor of hypoxic pulmonary vasoconstriction) starting with the ascent and ending on the third or fourth day after arrival at the final altitude. Other less popular and effective methods are inhaled beta-2-receptor agonists (salmetrol), phosphodiesterase inhibitors and dexamethasone [8-10].
Conclusion
Even though HAPE is mostly observed in high altitudes, physicians working in intermediate altitudes should be aware of its occurrence when treating cases of breathlessness. Such cases are easily reversible and can save a good number of patients just by bringing them to low lands.
Contributors: SDA: manuscript writing, patient management; DS, KS: manuscript editing, patient management; AB: critical inputs into the manuscript. DS will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Hackett PH, Roach RC. High altitude medicine. In: Auerbach PS, editor. Wilderness medicine. 5th ed. Philadelphia: Mosby Elsevier;2007.
- Hultgren HN. High-altitude pulmonary edema: current concepts. Annu Rev Med. 1996;47:267-284.
- West JB, Mathieu-Costello O. Structure, strength, failure, and remodeling of the pulmonary blood gas barrier [review]. Annu Rev Physiol. 1999;61:543.
- Houston CS. Acute pulmonary edema of high altitude. N Engl J Med. 1960;263:478-480.
- Gabry AL, Ledoux X, Mozziconacci M, Martin C. High-altitude pulmonary edema at moderate altitude (<2,400 m; 7,870 feet): a series of 52 patients. Chest. 2003;123:49-53.
- Bärtsch P. High altitude pulmonary edema. Med Sci Sports Exerc. 1999;31:S23-S27.
- Swenson ER. Carbonic anhydrase inhibitors and ventilation: a complex interplay of stimulation and suppression. Eur Resp J. 1998;12:1242-1247.
- Matthay MA, Flori HR, Conner ER, Ware LB. Alveolar epithelial fluid transport: basic mechanisms and clinical relevance. Proc Assoc Am Physicians. 1998;110:496-505.
- Richalet JP, Gratadour P, Robach P, Pham I, Déchaux M, Joncquiert-Latarjet A, et al. Sildenafil inhibits altitude-induced hypoxemia and pulmonary hypertension. Am J Respir Crit Care Med. 2005;171:275-281.
- Maggiorini M, Brunner-La Rocca HP, Peth S, Bernheim A, Kiencke S, Bloch KE, et al. Both Tadalafil and Dexamethasone may reduce the incidence of high-altitude pulmonary edema: A randomized trial. Ann Intern Med. 2006;145:497-506.