Rajesh Sinha, Hari Shankar Pandey1, Monil Singhai2
From the Department of Dermatology, Pathology1 and Microbiology2
Government Medical College, Haldwani, Nanital, Uttarakhand- 263139, India.
Corresponding Author:
Dr. Rajesh Sinha
Email: sinhaderma@gmail.com
Abstract
Histoid leprosy is a rare form of multibacillary leprosy with unique clinical and histopathological features. Lesions of histoid leprosy can mimic neurofibroma, xanthoma, dermatofibromas, reticulohistiocytosis and cutaneous metastasis. We report a case of “de novo” histoid leprosy which mimicked neurofibromatosis in its clinical presentation.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa45401000000f800000001001300
6go6ckt5b5idvals|130
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Leprosy is a chronic granulomatous disease involving, mainly skin and peripheral nerves. Madrid Classification of leprosy classifies leprosy into four types namely lepromatous, tuberculoid, borderline and indeterminate [1]. Histoid leprosy is a rare distinct variant of lepromatous leprosy that occurs in patients who relapse after dapsone monotherapy, in the presence of dapsone resistance or very rarely de novo [2]. We report a case of “de-novo” histoid leprosy that was misdiagnosed as neurofibromatosis
Case Report
A 39 year old female presented to us with asymptomatic raised skin lesions all over her body for last 3 months. She was previously diagnosed as neurofibromatosis by a local physician. There was no history suggestive of any drug intake for leprosy. Clinical examination revealed presence of multiple, nontender, skin coloured nodules varying in size from 0.5 cm to 3 cm in diameter all over the body, mainly concentrated on back and abdomen [Figure 1]. There was no impairment of pain, touch, or temperature sensation. Peripheral nerve examination was normal. Provisional diagnosis of histoid leprosy/neurofibroma, were made and slit skin smear and biopsy was performed. Slit skin smear revealed plenty of acid-fast bacilli, with a bacterial index of 5+. Histopathology showed atrophic epidermis with a subepidermal grenz zone. The dermis showed sheets of round to spindle-shaped histiocytes arranged in interlacing bundles, whorls, and crisscross patterns. The nuclei were pyknotic and cytoplasm was foamy and vacuolated [Figure 2]. The Wade-Fite stain showed plenty of acid-fast bacilli [Figure 3]. All these finding confirmed the diagnosis of histoid leprosy. She was treated with ROM (Rifampicin, ofloxacin, minocycline) therapy initially, and then advised multidrug therapy (MDT).
 Figure 1: Multiple skin coloured nodules on back.
Figure 1: Multiple skin coloured nodules on back.
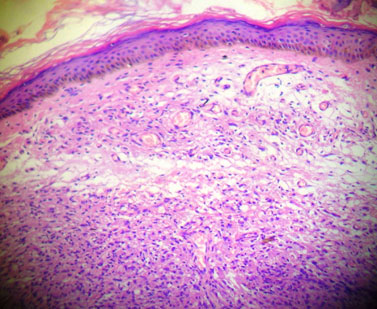 Figure 2: Histopathology of the nodule showing atrophic epidermis and grenz zone. The dermis is replaced by spindle-shaped histiocytes arranged in interlacing bundles, whorls, or crisscross patterns (10X, H & E).
Figure 2: Histopathology of the nodule showing atrophic epidermis and grenz zone. The dermis is replaced by spindle-shaped histiocytes arranged in interlacing bundles, whorls, or crisscross patterns (10X, H & E).
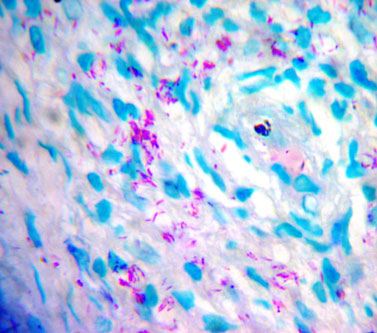 Figure 3: Photomicrograph showing numerous acid-fast bacilli (100X, Wade-Fite stain).
Discussion
Histoid leprosy was originally described by Wade in 1963 as discrete, firm, dome-shaped nodules which develop on apparently normal skin in patients of lepromatous leprosy [3].It is considered a variant of lepromatous leprosy and by others as distinct entity [3,4]. It is so called because the microscopic appearance of nodule shows spindle-shaped cells resembling those of dermatofibroma. It occurs in lepromatous patients who relapse after dapsone monotherapy or in the presence of dapsone resistance. But, histoid leprosy may occur rarely in patients presenting for the first time and have not received previous antileprotic treatment i.e. arising “de-novo” [5]. These cases are usually misdiagnosed and clinician should maintain high index of suspicion to diagnose this unusual presentation in absence of anaesthesia.
Figure 3: Photomicrograph showing numerous acid-fast bacilli (100X, Wade-Fite stain).
Discussion
Histoid leprosy was originally described by Wade in 1963 as discrete, firm, dome-shaped nodules which develop on apparently normal skin in patients of lepromatous leprosy [3].It is considered a variant of lepromatous leprosy and by others as distinct entity [3,4]. It is so called because the microscopic appearance of nodule shows spindle-shaped cells resembling those of dermatofibroma. It occurs in lepromatous patients who relapse after dapsone monotherapy or in the presence of dapsone resistance. But, histoid leprosy may occur rarely in patients presenting for the first time and have not received previous antileprotic treatment i.e. arising “de-novo” [5]. These cases are usually misdiagnosed and clinician should maintain high index of suspicion to diagnose this unusual presentation in absence of anaesthesia.
Clinically histoid leprosy is characterised by multiple, discrete, smooth, painless, firm skin coloured nodules and papules on apparently normal skin. The nodules may be cutaneous or subcutaneous, usually affecting extensor surface of extremities, back, buttocks and face. Histoid lesions may also occur along the course of peripheral nerve trunks and cutaneous nerves [6]. Histoid leprosy can clinically resemble with dermatofibromas, xanthomas, neurofibromas, reticulohistiocytosis and cutaneous metastasis. Occasionally, lesions may resemble molluscum contagiosum [1]. Histoid leprosy can be differentiated from above mentioned lesions on the basis of the characteristic histopathology and presence of mycobacterium on slit skin smear examination.
Classical histopathological findings of histoid leprosy include epidermal atrophy as a result of dermal expansion by the underlying leproma and acellular band (grenz zone) located below the epidermis. Dermis is filled with fusiform histiocytes arranged in a whorled, criss-cross or storiform pattern. These histiocytes resemble fibroblasts and it is suggested that fibroblast-like macrophages may have arisen from the tissue histiocytes rather than blood monocytes [2]. Within these histiocytes, abundance of acid-fast bacilli are seen which are longer than the normal bacilli, uniform in length and are arranged in parallel bundles along the long axis of histiocytes [2].
Clinical presentation of our case was suggestive of histoid leprosy, which was confirmed by slit skin smear and histopathological examination. Though rare, because of multibacillary character and high bacillary load, histoid leprosy poses a challenging problem especially in post leprosy elimination phase. Palit and Inamdar have suggested that histoid form of leprosy could serve as a reservoir of leprosy and as a source of new cases [7]. Our report of this case illustrates the importance of high index of suspicion for histoid leprosy, so that these cases are diagnosed early and promptly treated, thus preventing the further spread of the disease.
UK automatic cheap Replica Watches uk for men here are at affordable prices. All the collections are available.
Top Replica Watches UK – Buy Cheap 1:1 AAA Fake Watches: replica4u.com
References
- Sharma VK. Leprosy: Classification and clinical features. In: Valia RG,Valia AR. Eds. IVADL Textbook and atlas of dermatology.Vol II, 2nd edn, Bhalani publishing house, Mumbai 2001: p. 1578-1603.
- Pfaltzgraff RE, Ramu G. Clinical leprosy. In: Hastings C, Opromolla DVA, Eds.Leprosy. 2nd edn. Churchill Livingstone, Edinburgh, 1994: p. 266-268.3.
- Wade HW. The histoid variety of lepromatous leprosy. Int J Lepr 1963; 31:129-142.
- Sehgal VN, Srivasta G. Histoid leprosy. Int J Dermatol 1985;24:286-292.
- Rodriguez JN. The histoid leproma: its clinical characteristics and significance. Int J Lepr 1969;37:1-21.
- Ramanujam K, Arunthathi S, Chacko CJG, Jacob M. Neural histoid leproma in peripheral nerves – a case report. Lepr Rev 1984;54:63-68.
- Palit A, Inamadar AC. Histoid leprosy as reservoir of disease: a challenge to leprosy elimination. Lepr Rev 2007;78:47-49.
|