R.V.Dosi, S. Saraiya, R.D.Patell, N.N.Sonune, S.D. Sheth
From the Department of Medicine,
Government Medical College & S.S.G. Hospital, Vadodara, Gujarat, India
Corresponding Author:
Dr. R.V.Dosi
Email: rupal265@yahoo.com
Abstract
Sheehan’s syndrome or postpartum pituitary necrosis is hypopituitarism, caused by necrosis due to blood loss and hypovolemic shock as a complication of pregnancy. We describe a case of 45 year old woman with Sheehan’s syndrome who presented with recurrent symptomatic hypoglycaemia and pancytopenia. Association of Sheehan’s syndrome and pancytopenia is rare and to best of our knowledge only eight cases have been reported so far. The symptomatic treatment with levothyroxine, prednisolone, bisphosphonates, calcium and vitamin D cured her general symptoms, hypoglycemia and pancytopenia.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa854010000004e00000001000500
6go6ckt5b5idvals|131
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Sheehan’s syndrome is defined by varying degree of anterior pituitary hormone deficiency due to post-partum ischemic necrosis of the pituitary gland following massive bleeding [1]. Sheehan's syndrome has become uncommon with advanced obstetric care. In many patients, anterior pituitary dysfunction is often formulated after some years of inciting delivery. Hypoglycemia due to growth hormone, adrenal and other counter regulatory hormone deficiency is a known complication of Sheehan’s syndrome. The most frequent hematologic finding is anemia [2,3]. Pancytopenia is rarely observed and only eight cases showing association between Sheehan’s syndrome and pancytopenia have been reported till now [4]. We report a case of patient with Sheehan’s syndrome who had pancytopenia that recovered after replacement of glucocorticoids and thyroid hormones.
Top Swiss Made CHEAP Fake Watches UK - Best Replica Rolex Omega Breitling Replica Watches
Hope you find your uk best quality omega cheap replica watches UK here with less money.
Case Report
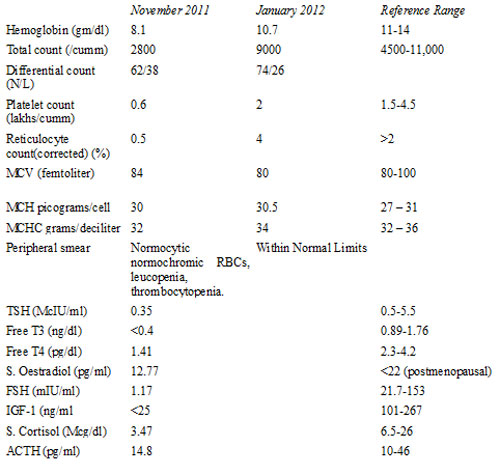
A 45 year old female patient presented to the emergency department with a history of sudden onset unconsciousness. The accompanying relatives reported that the patient was uneasy, perspiring and confused before she rapidly slipped into the presenting stupor. She was cold, diaphoretic and her random glucose was 34mg/dL. The patient regained consciousness following infusion of 50 grams of dextrose. She had similar history of frequent episodes of hypoglycemia over the past three years. Examination revealed pulse rate of 60 per minute, blood pressure of 100/66 mm Hg with pale and dry skin. The accompanying hoarseness of voice, facial puffiness, non-pitting pedal edema and delayed relaxation of ankle jerk suggested clinical diagnosis of myxoedema. The investigations were suggestive of low thyroid stimulating hormone (TSH), free thyroxine (FT4) and free triiodothyronine (FT3) suggestive of secondary (central) hypothyroidism [Table 1]. Her haemogram showed pancytopenia, with normal indices and a low reticulocyte count.
A detailed interview revealed history of postpartumhaemorrhage four years ago during her last pregnancy for which she wastransfused with nine units of blood The patient had amenorrhea sincethen and she presumed it to be due to hysterectomy done to controlpostpartum haemorrhage. Taking into consideration all of thesehypopituitarism was thought of; pituitary hormone studies werecompatible with pituitary insufficiency [Table 1]. The diagnosis ofSheehan’s syndrome was further supported by the MRI brain demonstratingan empty sella [Figure 1]. Patient was discharged on levothyroxine andprednisolone, along with bisphosphonates, calcium and vitamin D and onfollow up there was complete recovery of pancytopenia. Hormone therapyfor reproductive function was considered and decided against taking intoaccount of her age and personal opinion.
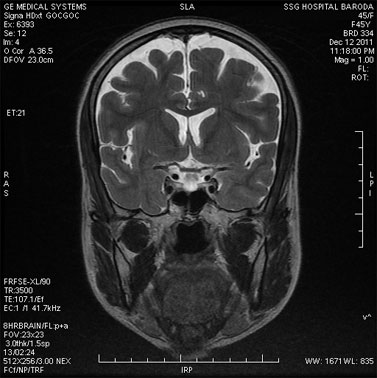
Fig.1: MRI Brain shows pituitary fossa with empty sella.
Table 1: Investigations of patient
Discussion
Hypoglycemia as a presenting feature for hypopituitarism is more often seen in the setting of pituitary apoplexy than Sheehan’s [1]. Our patient presented with recurrent admissions for life threatening hypoglycemia, along with pancytopenia. The misconception of obstetric hysterectomy done during her last caesarean section prevented her from revealing history of secondary amenorrhea. The stormy obstetric history in the past and clear signs of hypothyroidism on examination led us to the diagnosis. Later, pelvic exam and sonogram, confirmed the presence of the uterus and ovaries proving that the amenorrhea was in fact due to hypogonadotrophic hypogonadism. Moreover, while hypoglycaemia and pancytopenia occur in many systemic conditions, they can even dominate the clinical picture and possess a challenge for clinicians in the diagnosis.
Hormonal deficiencies, such as hypothyroidism, adrenal insufficiency and gonadal hormone deficiency can explain normochromic anemia in hypopituitarism[4,5]. As pituitary hormones modulate the production of erythropoietin it can be the result of a physiologic adjustment to low oxygen in the kidney. This is supported by the low erythropoietin levels found in these patients [5]. However, pancytopenia is rarely observed in Sheehan’s syndrome and is best explained as a result of loss of effect of pituitary hormones on metabolic reactions to hematopoiesis. The association between the hypopituitarism and hematological abnormalities are further supported by a complete reversal in hematological parameters with hormone replacement, both in the case reported as well as in literature [6,7,8,9]. In women having previous pregnancy with postpartum haemorrhage and current amenorrhea, Sheehan’s syndrome can be a cause of pancytopenia. Initial screening in the form of thyroid function tests revealing secondary hypothyroidism would be a pointer towards the possibility of Sheehan’s syndrome, before full evaluation is undertaken.
This case report emphasizes the long duration of time that may elapse between the postpartum haemorrhage and the eventual diagnosis of hypopituitarism along with rare association of Sheehan’s syndrome with pancytopenia.
References
- Tessnow AH, Wilson JD. The Changing Face of Sheehan's Syndrome. The Am J Med Sci. 2010;340: 402-406.
- Patrelli TS, Soncini E, Chiodera P, Fadda GM, Nardelli GB. A case report of Sheehan's syndrome with acute onsethyponatremia and severe anemia. Acta Biomed 2009;80:73-76.
- Fatma M, Mouna E, Nabila R, Mouna M, Nadia C, Mohamed A. Sheehan's syndrome with pancytopenia: a case report and review of the literature. J Med Case Reports 2011; 5: 490.
- Akoz AG, Atmaca H, Ustundag Y, Ozdamar SO. An unusual case of pancytopenia associated with Sheehan's syndrome. Ann Hematol 2007,86:307-308.
- Gokalp D, Tuzcu A, Bahceci M, Arikan S, Bahceci S, Pasa S. Sheehan's syndrome as a rare cause of anemia secondary to hypopituitarism. Ann Hematol 2009,88:405-410.
- Kim DY, Kim JH, Park YJ, Jung KH, Chung HS, Shin S et al Case of complete recovery of pancytopenia after treatment of hypopituitarism. Ann Hematol 2004,83:309-312.
- Laway BA, Bhat JR, Mir SA, Khan RS, Lone MI, Zargar AH. Sheehan's syndrome with pancytopenia--complete recovery after hormone replacement (case series with review). Ann Hematol 2010,89:305-308.
- Ferrari E, Ascari E, Bossolo PA, Barosi G. Sheehan's syndrome with complete bone marrow aplasia: long-term results of substitution therapy with hormones.Br J Haematol 1976;33:575-582.
- Ozdogan M, Yazicioglu G, Karadogan I, Cevikol C, Karayalcin U, Undar L. Sheehan's syndrome associated with pancytopenia due to marrow aplasia: full recovery with hormone replacement therapy. Int J Clin Pract 2004,58:533-535.
|