benadryl and pregnancy risks benadryl and pregnancy
From the Department of Orthopaedics,
ESI Hospital, Okhla, New Delhi, India.
Corresponding Author:
Dr. A.K.Dawar
Email: dawar101@gmail.com
Abstract
Muscle herniation of lower limb is a rare clinical entity. Tibialis anterior muscle hernia most commonly occurs as a result of an acquired fascial defect, often secondary to trauma. Most of them are asymptomatic and do not pose a diagnostic or therapeutic challenge. Large symptomatic hernias of leg are unusual and their treatment is controversial. We report such a case of large tibialis anterior muscle hernia that presented with chronic leg pain and was treated successfully by longitudinal fasciotomy.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff548b01000000b500000001000100 6go6ckt5b5idvals|138 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Herniation of muscle through a defect in the fascial sheath is rare. Muscle hernias generally occur in lower limb and affect tibialis anterior muscle. Occupational and sporting activities like foot soldiers, mountain climbers, skiers and athletes have been implicated as causes [1]. Large symptomatic muscle hernias are rarer. In this report, we present a case of large tibialis anterior muscle hernia presenting as cause of chronic leg pain. Muscle protrudes through a defect in the fascia into the subcutaneous fat and presents clinically as a soft-tissue mass.
Case Report
A 40 year old man with a history of blunt trauma in left leg 6 years back, presented with pain in left leg for last one year. The pain progressively increased on exertion and was relieved with rest. There was no history of backache or radiculopathy. He gave no history of smoking.
Local examination of leg was unremarkable except for slight bulge of muscle in anterior compartment of leg [Fig.1]. His peripheral pulses and reflexes were normal with no evidence of varicose veins and sensorimotor deficit of lower limbs. Routine blood and urine examination was normal with no abnormality seen on lower limb X-ray. CT spine to rule out spinal canal stenosis did not reveal any abnormality. Empirical treatment of leg pain failed to relieve his discomfort. Persistent questioning about leg pain revealed increased swelling of leg anteriorly after exertion and at time of increased leg pain. On examination a non-tender bulge of tibialis anterior was found after prolonged standing. Muscle hernia of leg was suspected and confirmed by ultrasound examination which showed 10 x 5 cm bulge of tibialis anterior muscle belly thorough weak covering fascia on muscle contraction.
 Fig.1: Pre-op photograph of affected leg showing diffuse bulge of anterior compartment of leg.
Provisional diagnosis of tibialis anterior muscle hernia was made. Conservative treatment in form of crepe bandage failed to relieve his symptoms. In view of disabling symptoms interfering with daily activities, surgical treatment was offered to him. During surgery, longitudinal skin incision was made and fascia exposed. A thinning of fascia was seen over a length of 14 cm [Fig.2]. Extensive longitudinal fasciotomy was done without any attempt to repair the fascial defect [Fig.3]. Following fasciotomy, patient was relieved of his leg pain and he remains symptom free 12 months after surgery with acceptable bulge of tibialis anterior.
Fig.1: Pre-op photograph of affected leg showing diffuse bulge of anterior compartment of leg.
Provisional diagnosis of tibialis anterior muscle hernia was made. Conservative treatment in form of crepe bandage failed to relieve his symptoms. In view of disabling symptoms interfering with daily activities, surgical treatment was offered to him. During surgery, longitudinal skin incision was made and fascia exposed. A thinning of fascia was seen over a length of 14 cm [Fig.2]. Extensive longitudinal fasciotomy was done without any attempt to repair the fascial defect [Fig.3]. Following fasciotomy, patient was relieved of his leg pain and he remains symptom free 12 months after surgery with acceptable bulge of tibialis anterior.
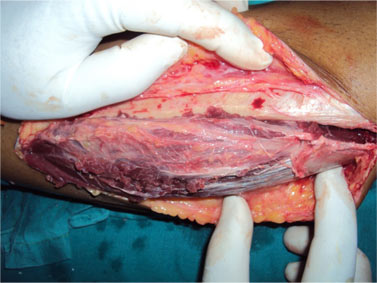 Fig.2: Per operative picture of hernia of tibialis anterior showing fascial defect.
Fig.2: Per operative picture of hernia of tibialis anterior showing fascial defect.
 Fig.3: Muscle hernia after longitudinal fasciotomy.
Discussion
About 200 cases of muscle hernias have been described in literature. Most of the cases are small in size and described in athletes and young adults requiring excessive strain on legs [2,4]. Because of superficial and tight fascial compartment, anterolateral tibial compartment is the commonest site affected by muscle herniation [2,3,4].
Muscle herniation can be classified as traumatic or constitutional. Traumatic muscle hernias are either direct following an open injury to the leg, or indirect following a repeated blunt trauma to a contracted muscle causing rupture of the fascia and consequent herniation of the muscle [5]. Constitutional hernias are caused by chronic stress on the fascia from the underlying muscle. It has been suggested that the fenestrations through which perforating veins enter enlarge and eventually muscle hernias bulge through these openings in the fascia [6]. In our case, blunt trauma to leg in road traffic accident 6 years back might have contributed to weakness of tibialis anterior fascia which led to symptomatic hernia later on. It is easier to diagnose small muscle hernias by local examination. When hernia is large, the diagnosis is difficult due to diffuse bulge. High degree of awareness about possibility of muscle hernia can help in early diagnosis which can be confirmed by dynamic sonography [4]. Muscle bulge through fascia is identified and dynamic examination of muscle is possible as muscle contracts and relaxes back through fascial defect.
Treatment for tibialis anterior muscle herniation is controversial. Asymptomatic hernias require reassurance, but no specific treatment. Minimally symptomatic hernias may respond to conservative treatment with restriction of exercise and the use of an elastic support [7]. Traditional surgical options involve direct closure of the defect. However, this is often not possible and if attempted can fail, causing a recurrence of the hernia [5]. This technique is also likely to increase intracompartmental pressure because the compartment is, in effect, made smaller. This elevation of pressure is accentuated in the postoperative period by oedema, predisposing the patient to developing compartment syndrome in the anterior compartment [7,9,10]. The fascial opening can also be repaired with a patch of fascia lata or periosteal graft, but this requires the use of an additional donor scar and may still cause a compartment syndrome [11]. Hence, the recommended surgical treatment is longitudinal fasciotomy to prevent any possibility of the development of a compartment syndrome [8,10,12].
In conclusion, muscle hernias should be considered as a rare differential diagnosis whenever patients present with persisting limb pain. Diagnosis is mostly clinical, but can be confirmed by imaging techniques like ultrasound. If conservative treatment fails, we recommend fasciotomy to prevent development of compartment syndrome.
References
Fig.3: Muscle hernia after longitudinal fasciotomy.
Discussion
About 200 cases of muscle hernias have been described in literature. Most of the cases are small in size and described in athletes and young adults requiring excessive strain on legs [2,4]. Because of superficial and tight fascial compartment, anterolateral tibial compartment is the commonest site affected by muscle herniation [2,3,4].
Muscle herniation can be classified as traumatic or constitutional. Traumatic muscle hernias are either direct following an open injury to the leg, or indirect following a repeated blunt trauma to a contracted muscle causing rupture of the fascia and consequent herniation of the muscle [5]. Constitutional hernias are caused by chronic stress on the fascia from the underlying muscle. It has been suggested that the fenestrations through which perforating veins enter enlarge and eventually muscle hernias bulge through these openings in the fascia [6]. In our case, blunt trauma to leg in road traffic accident 6 years back might have contributed to weakness of tibialis anterior fascia which led to symptomatic hernia later on. It is easier to diagnose small muscle hernias by local examination. When hernia is large, the diagnosis is difficult due to diffuse bulge. High degree of awareness about possibility of muscle hernia can help in early diagnosis which can be confirmed by dynamic sonography [4]. Muscle bulge through fascia is identified and dynamic examination of muscle is possible as muscle contracts and relaxes back through fascial defect.
Treatment for tibialis anterior muscle herniation is controversial. Asymptomatic hernias require reassurance, but no specific treatment. Minimally symptomatic hernias may respond to conservative treatment with restriction of exercise and the use of an elastic support [7]. Traditional surgical options involve direct closure of the defect. However, this is often not possible and if attempted can fail, causing a recurrence of the hernia [5]. This technique is also likely to increase intracompartmental pressure because the compartment is, in effect, made smaller. This elevation of pressure is accentuated in the postoperative period by oedema, predisposing the patient to developing compartment syndrome in the anterior compartment [7,9,10]. The fascial opening can also be repaired with a patch of fascia lata or periosteal graft, but this requires the use of an additional donor scar and may still cause a compartment syndrome [11]. Hence, the recommended surgical treatment is longitudinal fasciotomy to prevent any possibility of the development of a compartment syndrome [8,10,12].
In conclusion, muscle hernias should be considered as a rare differential diagnosis whenever patients present with persisting limb pain. Diagnosis is mostly clinical, but can be confirmed by imaging techniques like ultrasound. If conservative treatment fails, we recommend fasciotomy to prevent development of compartment syndrome.
References
- Azar FM. Sports medicine. In: Canale ST, Beaty HJ (eds). Campbell’s Operative Orthopaedic, Vol. 3, 11th ed. Philadelphia, CA: Mosby Elsevier, 2008; 46: 2737–2882.
- Kim M, Hong SP, Hwang SM, Park H, Ahn SK. Tibialis anterior muscle herniation developed after trauma. Int. J. Dermatol. 2008; 47: 845–847.
- Agarwal A, Agarwal R. Abnormal presentation of tibialis anterior herniation. Eur. J. Orthop. Surg. Traumatol. 2006; 16: 271–272.
- Rho NK, Kim WS, Kim YJ, Yoo KH, Kim BJ, Kim MN. The use of dynamic ultrasonography for the confirmation of lower leg muscle herniation. Ann. Dermatol. 2008; 20: 190–193.
- Marques A, Brenda E, Amarante TJ. Bilateral multiple muscle hernias of the leg repaired with Marlex mesh. Brit J Plast Surg 1994; 47: 444–446.
- Obermayer ME, Wilson JW. Fascial hernias of the legs. JAMA, 1951;145: 548–549.
- Wolfort GF, Mogelvang C, Filtzer HS. Anterior tibial compartment syndrome following muscle hernia repair. Arch Surg 1973; 106: 97–99.
- Miniaci A, Rorabeck CH. Tibialis anterior muscle hernia: a rationale for treatment. Can J Surg 1987; 30: 79–80.
- Almdahl SM, Due J, Samdal FA. Compartment syndrome with muscle necrosis following repair of hernia of tibialis anterior. Acta Chir Scand 1987; 153: 695.
- Miniaci A, Rorabeck CH. Compartment syndrome as a complication of repair of a hernia of the tibialis anterior. J Bone Joint Surg Am 1986; 68: 1444–1445.
- Hartzell J. The use of living fascia transplant to repair a hernia of the tibialis anterior muscle. JAMA 1936; 107: 492–493.
- Bloem JJAM The treatment of muscle hernias by fascial splitting. Brit J Plast Surg 1976; 29:291–294.
|