Sajid Ansari, Kaleem Ahmad, Kanchan Dhungel, Panna Lal Sah, Mukesh Kumar Gupta, RK Rauniyar , Meenu Agrawal1
From the Department of Radiodiagnosis & Imaging and Department of Pathology1,
B.P. Koirala Institute of Health Sciences, Dharan, Nepal.
Corresponding Author:
Dr. Sajid Ansari
Email: drsajidansari@yahoo.co.in
Abstract
Retinoblastoma recurrence following enucleation is relatively rare complication. It usually involves orbit, pineal, parasellar or suprasellar regions. Meticulous follow-up during the first two years after surgery should be done in all patients undergoing enucleation for retinoblastoma. Radiotherapy and intensive systemic chemotherapy may be useful in this disease. We describe an unusual case of orbital recurrence of retinoblastoma with intracranial metastases in a 3 year old girl child.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64b201000000f400000001000800 6go6ckt5b5idvals|144 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Retinoblastoma is the most common primary ocular neoplasm of early childhood [1]. After enucleation or irradiation the cure rate is excellent, however there is increased risk of recurrent tumors or other primary neoplasms in hereditary retinoblastoma [2,3]. Other primary neoplasms in association with retinoblastoma are osteosarcoma and various soft-tissue sarcomas. We report a case of post-enucleation recurrence of retinoblastoma involving left eye along with suprasellar and leptomeningeal metastases.
Case Report
A 3 year-old girl presented with leukocoria of left eye for 3 months associated with pain, redness and itching of the eye along with proptosis. The patient was physically well with no family history of retinoblastoma. Ophthalmologic examination revealed mild proptosis, congested conjunctiva, dense vitreous opacities with normal cornea, lens and iris of left eye. Right eye was normal with normal ocular movement of both eyes. A-scan Ultrasound of left eye was suggestive of calcification showing high spikes with reflectivity. Computed tomography (CT) of orbit [Figure 1] showed slightly enlarged left globe with mildly enhancing intravitreous irregular mass of size 2.5x2 cm with internal calcific foci involving the retina with normal bony orbit. The radiological findings were consistent with retinoblastoma and the patient underwent enucleation of the left eye and part of optic stump was left. Intraoperative findings were - hyphaema in anterior chamber, tumor mass protruding into the vitreous chamber with normal optic nerve. Gross pathology of the globe, the cut surface revealed irregular gray-white granular growth in the posterior chamber. On microscopy, representative section of growth showed histologic features of retinoblastoma along with necrotic and calcific areas. Stump of optic nerve was not indentified grossly and histologically.
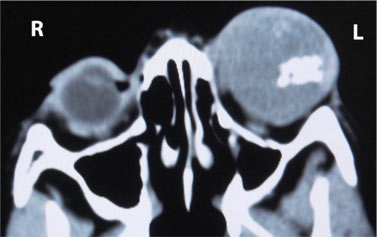 Figure 1: CT scan of orbits showing enlarged left globe with mildly enhancing intravitreous ill-defined mass with internal calcific foci involving the retina.
Post enucleation, radiotherapy/chemotherapy was advised due to advanced stage of the tumor, but was refused by patient’s family. Four months after enucleation she again came to the radiology department for CT scan of orbit and head with complains of exophytic growth in the left orbit [Figure 2]. CT scan of the orbit [Figure 3] revealed mildly enhancing mass of size ~ 5.5x4 cm in left orbit with a large exophytic component causing mild expansion of the bony orbit. Remaining part of left intraorbital optic nerve along with intracanalicular and intracranial part was diffusely thickened and showed mild enhancement on post-contrast study with widened optic canal. Mass involved all extraocular muscles, except small part of the superior rectus and inferior rectus muscles. CT scan of head [Figures 4a and 4b] revealed multiple enhancing ill-defined patchy and nodular lesions of variable sizes in basifrontal and right temporal regions along with bilateral sylvian fissures, falx cerebri, left cavernous sinus and suprasellar regions. The patient was again advised radiotherapy/chemotherapy but the patient’s family refused due to financial constraints and ultimately it came to our knowledge that the patient died of the metastatic disease.
Figure 1: CT scan of orbits showing enlarged left globe with mildly enhancing intravitreous ill-defined mass with internal calcific foci involving the retina.
Post enucleation, radiotherapy/chemotherapy was advised due to advanced stage of the tumor, but was refused by patient’s family. Four months after enucleation she again came to the radiology department for CT scan of orbit and head with complains of exophytic growth in the left orbit [Figure 2]. CT scan of the orbit [Figure 3] revealed mildly enhancing mass of size ~ 5.5x4 cm in left orbit with a large exophytic component causing mild expansion of the bony orbit. Remaining part of left intraorbital optic nerve along with intracanalicular and intracranial part was diffusely thickened and showed mild enhancement on post-contrast study with widened optic canal. Mass involved all extraocular muscles, except small part of the superior rectus and inferior rectus muscles. CT scan of head [Figures 4a and 4b] revealed multiple enhancing ill-defined patchy and nodular lesions of variable sizes in basifrontal and right temporal regions along with bilateral sylvian fissures, falx cerebri, left cavernous sinus and suprasellar regions. The patient was again advised radiotherapy/chemotherapy but the patient’s family refused due to financial constraints and ultimately it came to our knowledge that the patient died of the metastatic disease.
 Figure 2: Photograph of the patient showing exophytic growth in the left orbit, four months after enucleation.
Figure 2: Photograph of the patient showing exophytic growth in the left orbit, four months after enucleation.
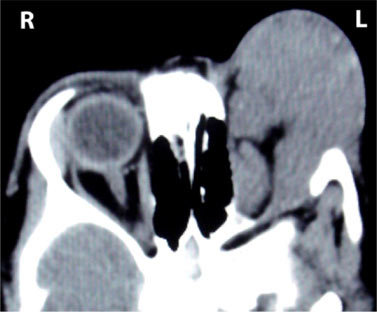 Figure 3: CT scan of the orbits showing mildly enhancing mass in left orbit with a large exophytic component causing mild expansion of the bony orbit with diffusely thickened part of optic nerve.
Figure 3: CT scan of the orbits showing mildly enhancing mass in left orbit with a large exophytic component causing mild expansion of the bony orbit with diffusely thickened part of optic nerve.
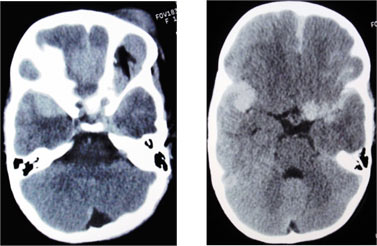 Figures 4 (a and b): CT scan of head showing multiple enhancing ill-defined patchy and nodular lesions in basifrontal and right temporal regions along with bilateral sylvian fissures, falx cerebri, left cavernous sinus and suprasellar regions.
Discussion
Retinoblastoma accounts for nearly 4% of all childhood malignancies and is bilateral in 35% of cases [4]. Bilateral retinoblastoma and 10-15% of unilateral retinoblastoma are usually hereditary in majority of the cases [5]. Inactivation of tumor suppressor gene (Rb1) is cause of retinoblastoma [6,7]. Cure rate of enucleation in patients with intraocular retinoblastoma is 90-95% [8]. Retinoblastoma recurrence following enucleation is relatively a rare complication; however its true incidence has not been estimated accurately [9].
The interval from enucleation to orbital recurrence is generally short, mean interval being 6.7 months [10,11]. In our case the patient had recurrence of the disease after four months. Three patterns of growth patternsare seen in primary retinoblastoma i.e. endophytic, exophytic and diffuse infiltrating pattern. Patients developing tumor recurrence following enucleation for intraocular disease should be distinguished from patients who present with extraocular retinoblastoma. On CT scan, the intracranial neoplasm appears usually isodense relative to gray matter and shows dense enhancement after intravenous contrast administration. On MRI, intracranial mass appears hypo- to isointense on T1-weighted images, hyperintense on T2-weighted images and enhances heterogeneously on contrast-enhanced MRI. Radiotherapy and intensive systemic chemotherapy may be useful in this disease [12].
For evaluation of metastasis in retinoblastoma recurrence, imaging modalities like MRI brain, CT abdomen, bone scan along with lumbar puncture, bone marrow aspiration and biopsy should be performed. Meticulous follow-up during the first two years after surgery should be done in all patients undergoing enucleations for retinoblastoma. Recurrence of the tumor may be asymptomatic or with subtle findings or may involve contralateral side, so, the clinicians should be well aware of these alarming features.In our case, the interval between onset of the initial symptoms and enucleation was 3 months. The patient did not receive any adjuvant chemotherapy/radiotherapy. The interval between enucleation and recurrence of the disease was 4 months. Unfortunately, the patient succumbed to a disease which still has a high mortality rate even with aggressive treatment.
Conclusion
This case report refers to a postenucleation recurrence of retinoblastoma with intracranial metastases. All patients undergoing enucleation for retinoblastoma, needs to be carefully followed-up after surgery for possibility of recurrences and development of metastatic disease. Multimodality approach for treatment of retinoblastoma has gradually improved the survival rate of these patients.
References
Figures 4 (a and b): CT scan of head showing multiple enhancing ill-defined patchy and nodular lesions in basifrontal and right temporal regions along with bilateral sylvian fissures, falx cerebri, left cavernous sinus and suprasellar regions.
Discussion
Retinoblastoma accounts for nearly 4% of all childhood malignancies and is bilateral in 35% of cases [4]. Bilateral retinoblastoma and 10-15% of unilateral retinoblastoma are usually hereditary in majority of the cases [5]. Inactivation of tumor suppressor gene (Rb1) is cause of retinoblastoma [6,7]. Cure rate of enucleation in patients with intraocular retinoblastoma is 90-95% [8]. Retinoblastoma recurrence following enucleation is relatively a rare complication; however its true incidence has not been estimated accurately [9].
The interval from enucleation to orbital recurrence is generally short, mean interval being 6.7 months [10,11]. In our case the patient had recurrence of the disease after four months. Three patterns of growth patternsare seen in primary retinoblastoma i.e. endophytic, exophytic and diffuse infiltrating pattern. Patients developing tumor recurrence following enucleation for intraocular disease should be distinguished from patients who present with extraocular retinoblastoma. On CT scan, the intracranial neoplasm appears usually isodense relative to gray matter and shows dense enhancement after intravenous contrast administration. On MRI, intracranial mass appears hypo- to isointense on T1-weighted images, hyperintense on T2-weighted images and enhances heterogeneously on contrast-enhanced MRI. Radiotherapy and intensive systemic chemotherapy may be useful in this disease [12].
For evaluation of metastasis in retinoblastoma recurrence, imaging modalities like MRI brain, CT abdomen, bone scan along with lumbar puncture, bone marrow aspiration and biopsy should be performed. Meticulous follow-up during the first two years after surgery should be done in all patients undergoing enucleations for retinoblastoma. Recurrence of the tumor may be asymptomatic or with subtle findings or may involve contralateral side, so, the clinicians should be well aware of these alarming features.In our case, the interval between onset of the initial symptoms and enucleation was 3 months. The patient did not receive any adjuvant chemotherapy/radiotherapy. The interval between enucleation and recurrence of the disease was 4 months. Unfortunately, the patient succumbed to a disease which still has a high mortality rate even with aggressive treatment.
Conclusion
This case report refers to a postenucleation recurrence of retinoblastoma with intracranial metastases. All patients undergoing enucleation for retinoblastoma, needs to be carefully followed-up after surgery for possibility of recurrences and development of metastatic disease. Multimodality approach for treatment of retinoblastoma has gradually improved the survival rate of these patients.
References
- Shields JA, Shields CL. Retinoblastoma. In: Shields JA, Shields CL, eds. Atlas of Intraocular Tumors. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999.
- Dunkel IJ, Gerald WL, Rosenfield NS, Strong EW, Abramson DH, Ghavimi F. Outcome of patients with a history of bilateral retinoblastoma treated for second malignancy: the Memorial Sloan-Kettering experience. Med Pediatr Oncol 1998; 30:59–62.
- Moll AC, Imhof SM, Bouter LM, Tan KE. Second primary tumors in patients with retinoblastoma: a review of the literature. Ophthalmic Genet 1997;18:27–34.
- Stolovitch C, Loewenstein A, Varssano D, Lazar M. Trilateral retinoblastoma. Metab Pediatr Syst Ophthalmol1992;15:57–59.
- Smith LM, Donaldson SS, Egbert PR, Link MP, Bagshaw MA. Aggressive management of secondary primary tumors in survivors of hereditary retinoblastoma. Int J Radiat Oncol Biol Phys1989; 17:499–505.
- Mayol X, Grana X. pRB, p107 and p130 as transcriptional regulators: role in cell growth and differentiation. Prog Cell Cycle Res 1997; 3: 157-169.
- Sellers WR, Kaelin WG Jr. Role of the retinoblastoma protein in the pathogenesis of human cancer. J Clin Oncol 1997; 15: 3301-3312.
- Honavar SG, Singh AD, Shields CL, Meadows AT, Demirci H, Cater J, Shields JA. Postenucleation adjuvant therapy in high-risk retinoblastoma. Arch Ophthalmol 2002; 120:923-931.
- Chantada GL, Dunkel IJ, de Davila MT, Abramson DH. Retinoblastoma patients with high risk ocular pathological features: who needs adjuvant therapy? Br J Ophthalmol 2004; 88:1069-1073.
- Ellsworth RM. Orbital retinoblastoma. Trans Am Ophthalmol Soc 1974; 72:79-88.
- Hungerford J, Kingston J, Plowman N. Orbital recurrence of retinoblastoma.Ophthalmic Paediatr Genet 1987; 8:63-68.
- Schvartzman E, Chantada G, Fandino A, Davila M, Raslawski E, Manzitti J. Results of a stage-based protocol for treatment of retinoblastoma. J Clin Oncol 1996; 14: 1532–1536.
|