6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff5408020000000f01000001001100
6go6ckt5b5idvals|162
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Kaposi’s sarcoma is a multifocal neoplastic proliferation of endothelial cells involving skin and other organs. This condition carries a variable clinical course ranging from minimal mucocutaneous disease to extensive organ involvement. The interval for development of Kaposi sarcoma is shortened in patients, where HIV infection precedes seroconversion to Human Herpes Virus 8 (HHV-8) positivity. In treatment of HIV-associated Kaposi sarcoma, Highly active anti retroviral treatment (HAART) and liposomal anthracyclines like doxorubicin are considered as first line systemic therapy for Kaposi’s sarcoma. The cause of low prevalence of KS in our country may be due to low prevalence of HHV-8 in our country. Very few such cases have been reported in Indian literature and this being novel in the sense that this patient responded excellently to traditional Anti-retroviral treatment and chemotherapy not mentioned elsewhere in Indian texts.
Case Report
A 52 year heterosexual married male presented with multiple, painful swellings over the right chest and lower leg of two months duration. This was accompanied by multiple oozing lesions over both axillae and neck for past 1 month. On taking detailed history he had history of multiple unprotected sexual exposures with Community Sexual Workers three years ago. On evaluation, tuberculous lymphadenopathy (cervical and axillary) was diagnosed for which he was on first line anti-tubercular treatment (ATT) for one month. There was no history of genital lesions or discharge, oral lesions, weight loss or any addiction.
General examination revealed bilateral axillary lymphadenopathy- 3 x 4 cm in size, discrete, firm, not attached to skin or overlying tissue. Cutaneous examination revealed multiple discrete reddish nodules and polypoidal growth on right side of chest ranging from 1 to 4 cm in diameter. Sinuses over right neck axilla and pectoral region were seen. Hyper-pigmented indurated plaque over right lower leg with few reddish nodules was also seen. Rest of the systemic examination was normal. A clinical differential diagnosis of Kaposi’s sarcoma was considered.
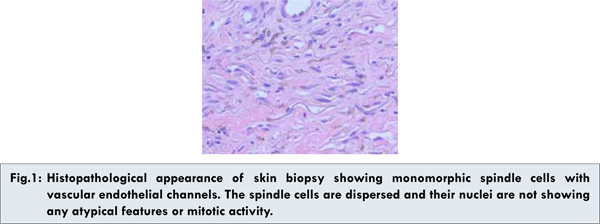
Routine haematological investigations, liver function test, X-ray chest were normal. Hepatitis B surface antigen, VDRL test for syphilis, Anti-Streptolysin O titre were negative. Mantoux test was positive along with HIV (1 and 2) positivity. Cluster differentiation-4 (CD4) count was 90/µl. Biopsy of right axillary lymph nodes was reported as Koch’s lymphadenitis. Ultrasonography of the abdomen revealed hepatosplenomegaly and of the chest showed right infraclavicular lymphadenopathy. Skin biopsy and axillary lymph node biopsy showed signs of Kaposi’s sarcoma [Figure 1]. Immunocytochemistry showed positivity of CD34 and negativity of CD31 and factor 8 with positive PAS and polymerase chain reaction for HHV8 confirming the diagnosis of Kaposi’s sarcoma in this seropositive patient.
There after he was started on Antiretroviral treatment (ART) with Lamivudine, Stavudine and Nevirapine. Chemotherapy with Vincristine, Bleomycin and Doxorubicin (6 cycles) was added. Later boosted Protease inhibitor regimen with Lamivudine, Stavudine, Ritonavir and Indinavir was given. Few lesions were treated with cryotherapy. His treatment for tuberculous lymphadenopathy was continued. Excellent clinical response was achieved and the cutaneous lesions regressed and CD4 count improved to 198/µl. Patient did not experience any significant side effects during this course of therapy.
Discussion
The first report of AIDS associated Kaposi’s sarcoma (KS) in India was described in the year 1993 since then quite a case reports of AIDS associated Kaposi’s sarcoma are described in Indian literature [1]. Despite rapid growth in the prevalence of AIDS in India very little is known regarding the spectrum of neoplasm in patients with AIDS. This case of Kaposi sarcoma represents the unique character of disease in clinical presentation and diagnostic findings but the vulnerability lies in the response achieved though treatment that is not seen elsewhere.
With the advent of AIDS, KS emerged from its relative anonymity and was seen in AIDS affected patients. In United States of America, Kaposi’s sarcoma is 20,000 times more common in AIDS patients than in general population and 300 times more common in immune compromised individuals [2-5]. In AIDS patients, it is more common in homosexual than in heterosexuals and it’s incidence is more in males than in females [6]. Women were more likely to suffer from KS if their partner is bisexual than intravenous drug users. Studies evaluating various types of sexual practices have found that the risk of developing AIDS related KS increases with oral- anal contact, faecal contact and with receptive anal intercourse and rectal gonorrhoea [7]. In contrast to other variants of KS the initial lesions in AIDS patients frequently develop on the face- eyelids, ears, nose and trunk, follows lines of cleavage. The initial lesion may be a small, raised reddish-purple nodule on the skin, a discoloration on the oral mucosa, or a swollen lymph node. Because of the vascular nature of the tumors and the presence of extravasated red blood cells in the lesions, their colors range from reddish to purple to brown and often take the appearance of a bruise, with yellowish discoloration and tattooing. Lesions range in size from a few millimeters to several centimeters in diameter and may be either discrete or confluent. KS lesions most commonly appear as raised macules; however, they can also be papular, particularly in patients with higher CD-4 T cell counts. In contrast to most malignancies, in which lymph node involvement implies metastatic spread and a poor prognosis, lymph node involvement may be seen very early in KS and is of no special clinical significance.
In this case, patient also revealed bilateral axillary lymphadenopathy with sinuses over right neck axilla and pectoral region along with skin lesions creating a dilemma in diagnosis. Cattleman’s disease was thought which is a non-cancerous neoplastic proliferation of lymph node. In HIV infected patients, the plasma cell variety of Cattleman’s disease frequently turns into multicentric variety, which has a poor prognosis, as most of them changes into B cell type of non-Hodgkin’s lymphomas. But skin lesions and histological finding did not confer this diagnosis. Other possibilities were tubercular lymphadenitis with cutaneous tuberculosis, non-Hodgkin’s lymphoma, acralangio dermatitis. Biopsy of lymph nodes suggested tubercular lymphadenitis which was an associated disease in this case of AIDS patient. Histopathological and immunocytochemistry findings of cutaneous lesions were consistent with the diagnosis of Kaposi’s sarcoma.
HIV trans-activating gene- tat promotes growth of AIDS-KS cells [8]. In addition, anti-tat antibodies specifically inhibit AIDS-KS cell growth. These cells stimulate their own growth (autocrine) and support growth of other cells (paracrine) by producing angiogenic growth factors and cytokines like Fibroblast Growth Factor (FGF), Tumor Necrosis Factor (TNF)-alpha, Interleukin (IL)-1, Interleukin (IL)-6, Oncostatin M (potent mitogen). It was later discovered that there is an association between Human herpes virus 8 and KS [9]. Using polymerase chain reaction (PCR) it was detected that HHV-8 like DNA sequence was seen in all clinical forms of KS- 87% of classic, 70% of African endemic and 100% of AIDS associated KS. The normal skin of patients of AIDS-KS also showed herpes like virus which suggests that this virus is disseminated on the skin of these patients. Oral fluids is the likely source for HHV-8 transmission and high HHV-8 antibody titres may protect against circulating HHV-8 viruses and new KS lesions.
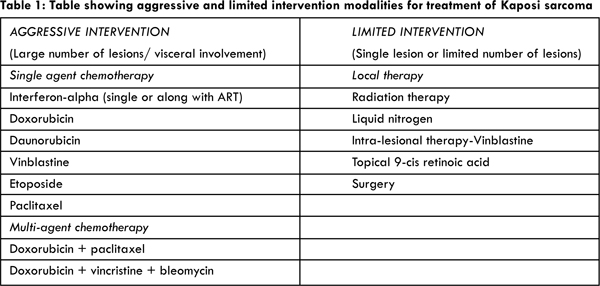
Local therapy in AIDS-KS is given for, limited number of cutaneous lesions, localized disease and associated complication caused by mass effects and cosmetic improvement. Liquid nitrogen cryotherapy has an 85% complete or partial clinical response rate at 11 weeks after therapy which lasts for 6 months for majority of the patients [Table1].
Chemotherapeutic agents for systemic therapy are now in use in our country along with combination of ART. Systemic interferon alpha has potent action as a modulator of immune function to augment natural killer cell activity; T-cell mediated cytotoxicity and macrophage activity along with direct antiproliferative activity, potent antiviral activity in vivo and ability to regress some malignant tumors. Synergistic action of Zidovudine combined with INF- alpha was seen in vitro. Neutropenia is the major limiting factor with this combination; others are anemia, thrombocytopenia, hepatotoxicity. Ritonavir- a protease inhibitor, acts as an anti-tumorigenic agent. Angiogenesis is thought to play a major role in the development of Kaposi’s sarcoma (KS), considered by many to be a hyperplastic disorder caused in part by local production of inflammatory cytokines. Ritonavir inhibits the production of these cytokines. It also improves immune cell viability and induces Ks cell apoptosis in vitro. It inhibits endothelial cell adhesion molecules like ICAM, VCAM, and Eselectin which act as pro-angiogenic agents.
Conclusion
AIDS associated Kaposi sarcoma though uncommon is seen in HIV positive patients with typical skin manifestations. Diagnosis of Kaposi sarcoma is never easy but it should be fore sought if cutaneous lesions give suspicion. Timely diagnosis with histopathological and serological evaluation could lead to better response with ART and chemotherapy of Kaposi sarcoma.
Acknowledgments
We would like to acknowledge our colleague Dr. B.E. Yathish for his kind guidance and support in this case report. No financial support is taken from any person or individual.
References
- Shroff HJ, Dashatwar DR, Deshpande RP, Waigmann HR. AIDS-associated Kaposi’s sarcoma in an Indian female. J Assoc Physicians India. 1993;41(4):241-242.
- Frisch M, Biggar RJ, Engels EA, Goedart JJ. JAMA. 2001;285(13):1736-1745.
- Goedert JJ, Coté TR, Virgo P, Scoppa SM, Kingma DW, Gail MH et al. Spectrum of AIDS-associated malignant disorders. Lancet. 1998;351:1833-1839.
- Mbulaiteye SM, Biggar RJ, Goedert JJ, Engels EA. J Acquir Immune Defic Syndr. 2003;32:527-533.
- Gallagher B, Wang Z, Schymura MJ, Kahn A, Fordyce EJ. Am J Epidem. 2001;154(6):544-556.
- Chandan K, Madnani N, Desai D, Deshpande R. AIDS - associated Kaposi’s sarcoma in a heterosexual male - A case report. Dermatol Online J. 8:19.
- Beral V, Bull D, Darby S, Weller I, Carne C, Beecham M, et al. Risk of Kaposi’s sarcoma and sexual practices associated with faecal contact in homosexual or bisexual men with AIDS. Lancet 1992;339:632-635.
- Ensoli B, Buonaguro L, Barillari G, Fiorelli V, Gendelman R, Morgan RA, Wingfield P, Gallo RC. Release, Uptake, and Effects of Extracellular Human Immunodeficiency Virus Type 1 Tat Protein on Cell Growth and Viral Transactivation. J. Virol. 1993;67:277-287.
- Schulz TF. KSHV/HHV8-associated lymphoproliferations in the AIDS setting. Eur. J. Cancer 2001; 37:1217-1226.