viagra prodej praha viagra cena
From the Central Institute of Orthopedics, VMMC and Safdarjung Hospital, New Delhi and Acharya Shri Chander Medical College and Hospital1, Jammu, J&K, India.
Corresponding Author:
Dr. Sumit Mahajan
Email: mahajan.sumit20@gmail.com
Abstract
Aneurysmal bone cysts are enigmatic, locally destructive, blood filled lesions of bone with unknown cause and unusual presentations. We report a case of 16 year old female with aggressive aneurysmal bone cyst of proximal left femur complicated by transcervical fracture neck of femur. As the age of the patient was not suitable for replacement, a successful attempt was made to salvage the hip with intralesional curettage and fixation with 2 fibular struts and a cancellous hip screw. Femoral head is viable till date.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff847d02000000b301000001000300 6go6ckt5b5idvals|181 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
The aneurysmal bone cyst (ABC) is an expansile cystic lesion that most often affects individuals during the second decade of life and may occur in any bone in the body. Although benign, the ABC can be locally aggressive and can cause extensive weakening of the bony structure and impinge on the surrounding tissues [1,2,3]. Pathological fractures of proximal femur secondary to benign bone tumors often are difficult to treat because of extensive bone destruction, periarticular location and high risk of local relapse [4]. A procedure that saves the joint and ensures low risk of recurrence is desirable. Thus, the treatment of such tumors is a challenge for Orthopaedic surgeons. We report a case of aneurysmal bone cyst of proximal femur complicated by fracture neck of femur, treated with curettage, fibular strut graft and cancellous hip screw.
Case Report
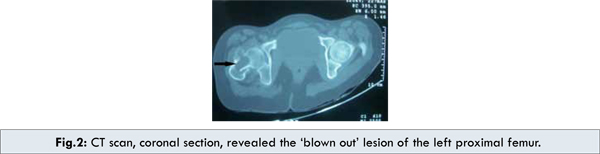
A 16 year old girl presented to the emergency with complaints of inability to bear weight on her left lower limb after history of trivial trauma. Examination revealed, externally rotated left lower limb with painful movements at hip joint. There was local tenderness on palpation with no distal neurovascular deficit. Roentgenogram revealed well defined expansile lesion involving proximal femur with extensive destruction associated with pathological fracture of neck of femur. Computerised tomography further delineates the radiographic findings [Fig.1,2]. Fine needle aspiration under image intensifier was performed and a provisional diagnosis of aneurysmal bone cyst was made.

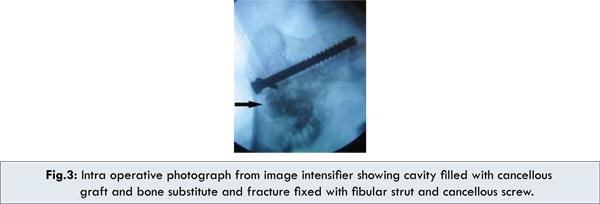
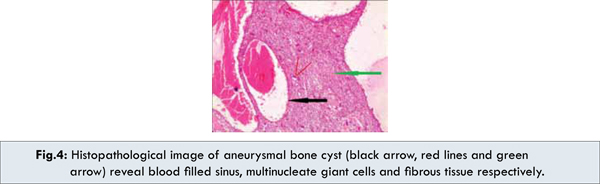
The patient was subsequently taken up for surgery and Watson Jones approach [5] was used to approach the hip and intralesional extended curettage was performed. The fracture was fixed with two fibular struts (taken from ipsilateral limb) and a 6.5 mm cancellous hip screw. The cavity was then filled with cancellous bone graft and bone graft substitutes (calcium triphosphate) [Fig.3]. Histology showed fibrous tissue with vascular spaces, haemosiderin deposits and multinucleated giant cells, consistent with aneurysmal bone cyst [Fig.4]. The patient was followed at 6 weeks, 3 months [Fig.5], 6 months and 12 months, and was evaluated with Harris hip score [6]. She was able to weight bear independently by 12 weeks and Harris hip score was 92.

Discussion
Aneurysmal bone cysts are locally destructive, blood-filled reactive lesions of bone. This entity was first described by Jaffe and Lichtenstein in 1942 [7]. It consists of blood-filled septate cavities lined by fibroblast and histiocytes. Hemosiderin-laden macrophages, chronic inflammatory cells, and multinucleated giant cells also are present [1,2,3,4,8]. Any bone may be involved, but the most common location includes the proximal humerus, distal femur, proximal tibia, and spine.
Approximately 85% of patients with ABCs present before age 20 and there is a slight female predominance [9,10]. Most patients with aneurysmal bone cysts complain of mild to moderate pain and swelling that has been present for weeks to several months. Pathologic fracture occurs in about 8% of ABC [9]. True etiology of these tumours is unknown. Most lesions arises de novo and are termed as ‘Primary ABCs’. They may also arise in conjunction with other lesions like fibrous dysplasia, osteoblastoma, chondromyxoid fibroma, nonossifying fibroma, chondroblastoma, osteosarcoma, chondrosarcoma, unicameral bone cyst, hemangioendothelioma, and metastatic carcinoma. Such tumours are designated as ‘Secondary ABCs’[11]. Features of the current case were consistent with primary ABC. Although the pathogenesis is uncertain, it is likely that aneurysmal bone cysts result from local circulatory disturbance leading to increased venous pressure and production of local haemorrhage [12].
Radiographs typically show an eccentric, lytic lesion with an expanded, remodelled ‘blown out’ or ‘ballooned’ bony contour of the host bone [13,14]. The natural history of aneurysmal bone cyst has been described as evolving through four radiological stages: initial, active, stabilization and healing [14,15]. In the initial phase, the lesion is characterized by a well- defined area of osteolysis with discrete elevation of the periosteum. This is followed by a growth phase, in which the lesion grows rapidly with progressive ‘destruction’ of bone and development of the characteristic ‘blown-out’ radiologic appearance. The growth phase is succeeded by a period of stabilization, in which the characteristic ‘soap bubble appearance’ develops, as a result of the maturation of the bony shell. Final healing stage results in progressive calcification and ossification, with the lesion transformed into a dense body mass. The current case was coherent with the growing phase of ABC.
CT scanning can be used to define the lesion and is especially valuable for those lesions that are located in areas in which the bony anatomy is complex and that cannot be adequately evaluated by plain films. CT scanning will show an interrupted cortex in many instances, although in these instances the adjacent soft-tissue mass is smooth, sharp and well defined, indicative of an intact periosteum [13]. MRI shows typically shows well-defined lesion, often with lobulated contours. Internal septa with multiple fluid levels may be seen. In T1- weighted images fluid levels are better seen [16]. Bone scintigraphy will show increased uptake of radionuclide in all cases and it accurately reflects the extent of osseous involvement in approximately 88 % cases [17].
Curettage with bone grafting and bone graft substitute remains the gold standard in the treatment of aneurysmal bone cysts. Recurrence rate is seen as 10-44 % of cases [2,3,7]. Recently, embolotherapy has been used to treat vascular bone tumors to limit blood loss at surgery or as definitive therapy to when surgery is not
feasible [18].
Despite the importance of proper treatment of this problem, the literature on the treatment strategy of pathological fractures of the proximal femur secondary to benign bone tumors is limited. The literature on pathological fractures in benign tumors other than fibrous dysplasia is more limited. Jaffe and Dunham reported on one patient with a pathological femoral neck fracture through an aneurysmal bone cyst [19]. This was treated with curettage, cortical fibular autograft, and dynamic hip screw. This patient had avascular necrosis and required a total hip replacement.
The current case illustrates a successful treatment for extensive benign bone tumor of the proximal femur with pathological fracture. Using the principles of extensive curettage, internal fixation with fibular strut graft and cancellous screw and anatomical reconstruction with cancellous bone graft and bone substitutes, the femoral head can be preserved with good functional and oncological outcome.
Conclusion
There is always a dilemma regarding the treatment of such a destructive and aggressive lesion by an orthopaedic surgeon. Replacement in such young patients must be limited to situations, when there is no alternation. So, ideal treatment plan includes effective curettage through wide exposure in addition to grafting with cancellous bone graft and bone substitutes and a rigid fixation with cancellous screws and fibular struts.
References
- Vigorita VJ, Ghelman B. Aneurysmal bone cysts. Orthopaedic Pathology. Philadelphia, Pa: Lippincott-Williams and Wilkins; 1999:262-274.
- Canale ST. Aneurysmal bone cyst within benign tumors of bone. In: Campbell’s Operative Orthopaedics.Vol 1. 11th ed. St. Louis, Mo: Mosby Year-Book. 2008:868.
- Bullough PG, Vigorita VJ. Aneurysmal bone cyst within benign non-matrix-producing bone tumors.Orthopaedic Pathology. 3rd ed. Baltimore, Md: Mosby-Wolfe. 1997:402-424.
- Wai EK, Davis AM, Graffin A. Pathologic Fractures of the Proximal Femur secondary to Benign Bone tumors. Clinical Ortho & research. 2001;393:279-286.
- Watson-Jones R. Fractures of the neck of the femur. Br J Surg. 1935-1936;23:787.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by moldarthroplasty. An end-result study using a new method of result evaluation, J Bone Joint Surg. 1969;51A:737.
- Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004-1025.
- Mendenhal WM, Zlotecki RA. Aneurysmal Bone Cyst. Am J Clin Oncol. 2006;29:311–315.
- Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R. Aneurysmal bone cyst. A population based epidemiologic study and literature review. Clin Orthop Relat Res. 1999;363.
- Cottalorda J, Kohler R, Sales de Gauzy J, Chotel F, Mazda K, Lefort G et al. Epidemiology of aneurysmal bone cyst in children: a multicenter study and literature review. J Pediatr Orthop B. 2004;13:389-394.
- Levy WM, Miller AS, Bonakdarpour A, Aegerter E. Aneurysmal bone cyst secondary to other osseous lesions. Report of 57 cases. Am J Clin Pathol. 1975;63:1-8.
- Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg. 2007;127:105-114.
- Hudson TM. Fluid levels in aneurismal bone cysts: A Ct feature. AJR. 1984;141:1001-1004.
- Scully SP, Temple HT, O’Keefe RJ, Gebhardt MC. Case report 830. Aneursymal bone cyst. Skeletal Radiol. 1994;23:157-160.
- Dabska M, Buraczewski J. Aneurysmal bone cysts: pathology, clinical course and radiological appearance. Cancer.1969;23:371-388.
- Munk PL, Helms CA, Holt RG, Steinbach L, Neumann C. MR imaging of aneurismal bone cysts. AJR. 1989;153:99-101.
- Hudson TM. Scintigraphy of aneurysmal bone cyst. AJR. 1984;142:761-765.
- De Cristofaro R, Biagini R, Boriani S, Ricci S, Ruggieri P, Rossi G, et al. Selective arterial embolization in the treatment of aneurysmal bone cyst and angioma of bone. Skeletal Radiol. 1992;21:523-527.
- Jaafe KA, Dunham WK. Treatment of benign lesions of femoral head and neck. Clin Orthop.
1990;257:134-137.
|