how much does abortion cost buy abortion pill
From the Department of Chest Diseases, Nephrology1, Pathology2: MS Ramaiah Medical College, Bangalore & Department of Cardiothoracic surgery3, MS Ramaiah Narayana Hrudayalaya, Bangalore-560054, India.
Corresponding Author:
Dr. Gayathri Devi HJ
Email: joshyev@gmail.com
Abstract
Early detection and effective treatment of opportunistic infections in immune-suppressed renal transplant patients are a part of a renal transplant programme. We are reporting a successfully treated case of concomitant pulmonary mucormycosis and cytomegalovirus (CMV) in a patient who had undergone renal transplant, twice.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff548502000000b301000001000900 6go6ckt5b5idvals|182 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Fungal infections continue to be a major diagnostic challenge in kidney transplant recipients and are associated with high mortality rates. The renal transplant patient on immunosuppressive drugs is susceptible for opportunistic infections. Significant proportions of patients are affected by pulmonary infections. Successful outcome requires early identification and effective treatment of the infections [1]. We are reporting about the successful treatment of concomitant cytomegalovirus and pulmonary mucormycosis in kidney transplant recipient.
Case Report
A 26 year old male patient was referred to chest medicine for the evaluation of persistent fever and cough of one month duration. His first renal transplant was done almost 13 years ago for which he developed refractory rejection after 10 years. He was on maintenance haemodialysis, until he underwent second renal transplant 18 months back. He was on regular follow up from outpatient department with triple immunosuppressant medications consisting of prednisolone, tacrolimus and mycophenolate mofetil. Both the donor and the recipients were negative for CMV before transplantation.
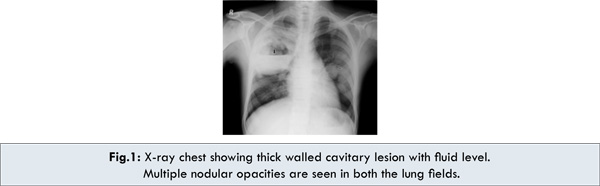
Physical examination revealed a thin young apprehensive man with fever and anemia having normal blood pressure and respiratory rate. Systemic examination was normal except for slightly decreased air entry on right side of chest. Investigations revealed a thick cavitary lesion in the right upper lobe suggestive of abscess with multiple nodular opacities in both the lungs. Sputum for acid fast bacilli was negative. Patient was treated with broad spectrum antibiotics with no response. Patient was put on anti-tubercular drugs by the nephrologist with the presumptive diagnosis of tuberculosis, when there was no response to broad spectrum antibiotics. Repeat chest X-ray showed persistence of the radiological abnormalities for which case was referred to pulmonology department.
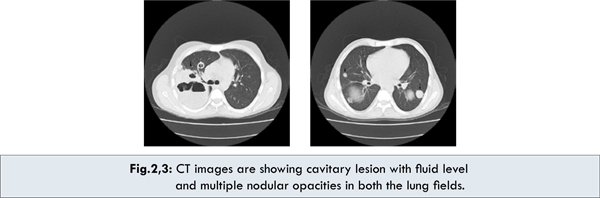
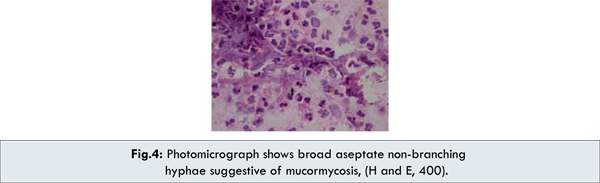
Chest X-ray and CT image shows a thick walled cavitary lesion occupying the right upper zone and mid zone [Fig.1]. Multiple nodular lesions like cannon ball shadows were seen in both the lung fields. Sputum was negative for fungal elements and malignant cells. Ultrasound examination of the kidneys did not reveal any evidence of malignancy. CECT Images showed a cavitary lesion with nodular opacities [Fig.2,3]. CT guided aspiration of the cavitary lesion showed fungal hyphae suggestive of mucormycosis [Fig.4].
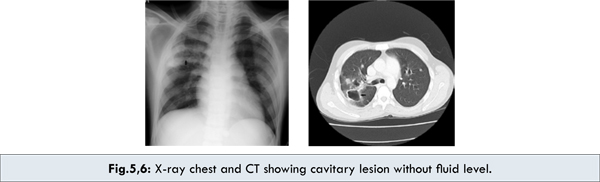
Patient was started on Amphotericin B (liposomal) with the diagnosis of mucormycosis. Patient showed symptomatic improvement. However, repeat chest x-rays showed persistence of the nodular opacities. Due to persistence of nodular opacities although patient was negative for CMV before transplant the same was retested and found to be positive. Patient was put on Gancyclovir along with Amphotericin B. Chest X-ray shows complete clearance of the nodular opacities with considerable reduction in the size of the right upper lobe cavitary lesion [Fig.5,6]. Patient underwent thoracotomy and right upper lobe segmentectomy in view of the persisting residual cavity. Histopathology examination revealed organizing pneumonia. Follow up chest X-ray appeared normal [Fig.7]. Patient remained asymptomatic during the last follow up.
Discussion
The renal transplant patient on immunosuppressive drugs is susceptible for opportunistic infections during the first 6 months. Common sites involved are lungs, urinary tract and surgical incision [2]. In a significant population of renal transplant recipients, main cause of death is pulmonary infection [3]. Fungal infections in solid organ transplant recipients are caused by Cryptococcus neoformans, Aspergillus, Candida species, Coccidiodomycosis, Histoplasma capsulatum and Mucormycosis [1].
Mucormycosis term is used for infections caused by fungi which belong to the order mucorales, first described by Paltauf in 1885 [4,5]. Mucor is found in soil and organic debris. The spores released by them can become airborne and inhalation can lead to germination and hyphae formation in an immunocompromised individual leading to variety of infections [6]. Most common manifestation of mucormycosis is rhinocerebral form. It can also manifest as pulmonary, cutaneous, gastrointestinal and disseminated forms [7]. Pulmonary mucormycosis is a rare fungal infection primarily seen in patients with immunocompromised states like diabetes mellitus, haematological malignancies, stem cell transplant patients and post renal transplant patients [8]. Methods of diagnosis include biopsy and CT guided aspiration of the involved organ. Surgical resection of the lesion and antifungal agents like Amphotericin B can be combined in resectable lesions [8].
Sharma A et al [8] have described a case of pulmonary mucormycosis presenting with multiple nodular opacities without obvious predisposing factors, successfully treated with Amphotericin B. High level of immune-suppression in the first 6 months of post transplant period carries the risk of opportunistic infections. The most common pathogens are tuberculosis and fungi [9]. More than two thirds of febrile episodes are caused by CMV during this period [10]. CMV infection is common after renal transplant [11]. It could be for the first time or a reactivation of a latent infection [3]. Besides, CMV infection causes increase in immunosuppression. Case reports of mixed infection by CMV and mucormycosis and potentiation of mucormycosis by CMV in renal transplant recipients is rare [7]. Early detection by isolation of virus or antibody titre is mandatory. Viral infection associated malignancies is another complication of immunosuppression. Nodular opacities in our patient prompted us to look for metastasis, since risk of malignancy is high in renal transplant recipients [12].
CT guided fine needle aspiration cytology technique is useful for the diagnosis of infections of the lung in immunocompromised patients [13]. Evaluation of the causative organism in our case required cytologic and serologic diagnosis. Incidence of post renal-transplant tuberculosis is high in developing countries. However, repeated sputum examination was negative for acid fast bacilli and CT guided aspiration of the pus was negative for TB culture in our patient.
Liposomal Amphotericin B is considered as the first line therapy for mucormycosis. Posaconazole is considered as second line drug currently for treating mucormycosis. It is used after control of the disease with liposomal amphotericin B as sequential therapy [14].
We report this case because of the prompt detection and early treatment of the causative organisms. Our patient was treated with Amphotericin-B, Gancyclovir and segmentectomy. Post-procedure, he had well preserved pulmonary reserve and allograft function.
Conclusion
High incidence of morbidity and mortality among renal transplant patients is caused by infections. Tuberculosis, fungal infections and cytomegalovirus are the most frequent causes [6]. High index of suspicion in diabetic and other immunocompromised patients is required to make an early diagnosis of pulmonary mucormycosis which is relatively uncommon but often fatal.
References
- Vinod PB, Sharma RK. Opportunistic infections (noncytomegalovirus) in live related renal transplant recipients. Indian J Urol. 2009;25:161-168.
- Masur H, Cheigh JS, Stubenbord WT. Infection following Renal Transplantation: A Changing Pattern. Reviews of Infectious Diseases. 1982;4;1208-1219.
- Crosbie WA, Parsons V, Culliford EJ, Bewick M. Opportunist Lung Infections in Renal Transplanted Patients. King’s College Hospital, London. www.era-edta.org/proceedings/vol13/vol13 206_210.pdf. Accessesd on 14 Jan 2013.
- Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clinical Microbiology and Infection. 2004;10:31–47.
- Bigby TD, Serota ML, Tierney LM, Matthay MA. Clinical spectrum of pulmonary mucormycosis. Chest. 1986;89:435-439.
- Atahan A Çagatay, Serkan S Öncü, Semra S Çalangu, Taner T Yildirmak, Halit H Özsüt, Haluk H Eraksoy. Rhinocerebral mucormycosis treated with 32 gram liposomal amphotericin B and incomplete surgery: a case report. BMC Infectious Diseases. 2001;1:22.
- Miladipour A, Ghanei E, Nasrollahi A, Moghaddasi H. Successful treatment of mucormycosis after kidney transplantation. Iranian Journal of Kidney Diseases. 2008;2:163-166.
- Sharma A, Gupta V, Singh RS, Kakkar N, Singh S, Bambery P. Angioinvasive pulmonary mucormycosis presenting as multiple bilateral pulmonary nodules in a patient without obvious predisposing factors. Singapore Med J. 2008;49:e269-271.
- Jha V, Chugh S, Chugh KS. Infections in dialysis and transplant patients in tropical countries. Kidney International. 2000;57:s85–s93.
- Erogul M. Renal Transplants; Medscape Chief E Erik D Schraga, MD. Updated: Nov 18, 2011. Accessed 14 January 2013.
- Alvin K, Sayeed M. Infections in Renal Transplant Recipients: Management Challenging, and Prevention Key. Nephrology times 2008;1:2-3.
- Flechner SM. Cancer and Renal Transplantation, Adv. Stud Med. 2007;7:411-419.
- Duggal, R, Rajwanshi A., Gupta N, Lal A, Singhal, M. Polymicrobial lung infection in postrenal transplant recipient diagnosed by fine-needle aspiration cytology. Diagn. Cytopathol. 2010;38:294–296.
- Nancy F Crum-Cianflon. Mucormycosis. emedicine.medscape.com/article/222551-overview. Accessed 14 Jan. 2013.
|