Azharuddin Mohammed Malik, Mehtab Ahmad1, Afreen Khan
From the Department of Medicine and Department of Radiodiagnosis1,
JN Medical College, Aligarh, India.
Corresponding Author:
Azharuddin Mohammed Malik
E-mail: malikazharuddin@gmail.com
Abstract
A 47 year old male with a history of hypertension and atrial fibrillation was found unconscious by his family members. His Glasgow Coma Scale score was 8 and the left pupil was dilated and nonreactive to light with the eye deviated downwards and outwards. MRI findings were consistent with subacute infarction in bilateral thalami and left anteromedial midbrain suggesting occlusion of the artery of Percheron. Transthoracic echocardiography revealed grade 2 left ventricular diastolic dysfunction with the presence of a clot in left atrium. A diagnosis of cardioembolic stroke was made and the patient was managed conservatively with anticoagulants.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64ac020000000b01000001001a00 6go6ckt5b5idvals|187 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Although infarcts restricted to the thalamus were reported for the first time more than 100 years ago, they remain a rare presentation of stroke and account for only 11% of all vertebrobasilar infarcts [1]. Bilateral infarctions in the paramedian artery territory are very rare and may result in a variety of clinical presentations. The paramedian thalamic territory is the median part of the thalamus including the intralaminar nuclei and most of the dorsomedian nucleus. The paramedian arteries usually arise from the first segment of posterior cerebral arteries (P1 segment) on both sides. An important anatomic variation of the blood supply of bilateral median part of thalamus is the origin of both paramedian arteries from a single pedicle which is known as the type B artery of Percheron [2]. Midbrain infarcts may result after occlusion of the artery of Percheron and they are usually limited to periaqueductal gray matter and affect the oculomotor and reticular nuclei. To date, the diagnosis of artery of Percheron infarction has been uncommon. In 2 large stroke series, the characteristic artery of Percheron infarct pattern was estimated to occur in 0.1% and 0.3% of all ischemic strokes [3]. We report the clinical and MR imaging findings in a patient who developed infarction in the typical distribution of the artery of Percheron.
Case Report
A 47 year old male with a past history of hypertension and atrial fibrillation was found unconscious in the early morning by his family members. He was noncompliant with his medications. On admission, his heart rate was 110/minute and irregularly irregular, blood pressure was 154/100 mm Hg, respiratory rate was 18/minute and axillary temperature was 37.2°C. On neurologic examination, his Glasgow Coma Scale (GCS) score was 8/15 (E1M5V2). Left pupil was dilated and nonreactive to light with the eye deviated downwards and outward. Right eye had normal pupillary reflexes. All limbs were moving in response to painful stimuli. All brainstem and deep tendon reflexes were present. Planter reflex was flexor on both sides. Rest of the systemic examination was normal.
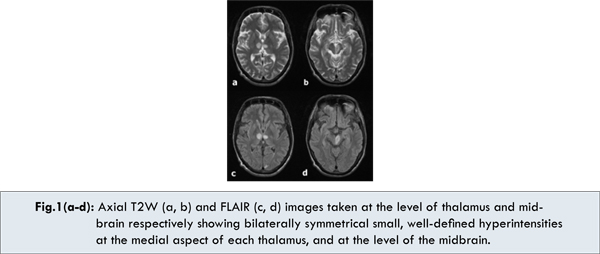
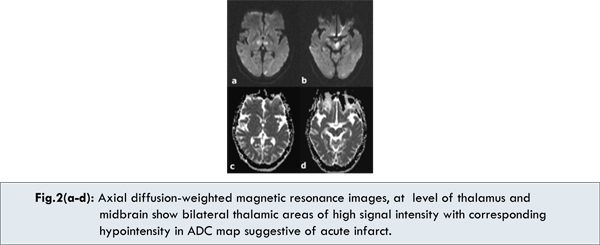
Laboratory test results showed haemoglobin 14.1 gm/dL, platelets 291x 103/mL; total cholesterol 221 mg/dL, triglycerides 126 mg/dL, high-density lipoprotein (HDL) 42 mg/dL, low-density lipoprotein (LDL) 83 mg/dL. Magnetic Resonance Imaging (MRI) showed bilaterally symmetrical infarcts in the medial thalamic region and rostral mid-brain region which appeared hyperintense on T2-weighted and FLAIR sequences, and hypointense on T1 weighted sequences of magnetic resonance imaging [Fig.1,2]. MR angiography did not reveal any significant finding. ECG showed atrial fibrillation with evidence of left ventricular hypertrophy. Transthoracic echocardiography showed grade 2 diastolic dysfunction with the presence of a clot in left atrium, both AV and semilunar valves were normal and EF was 57%. Patient was diagnosed as a case of cardioembolic stroke with bilateral thalamic and left periaqueductal midbrain infarction due of obstruction of artery of Percheron, the source of cardioembolism being left atrial clot secondary to atrial fibrillation.
The patient was started on mannitol, aspirin, atorvastatin, metoprolol in standard recommended dosages. Low molecular heparin was also given which was later overlapped with and then switched to oral warfarin, with dose titration to achieve an INR of 2.5. Telmisartan was also added later to optimise blood pressure control. Patient’s level of consciousness started improving with GCS Score of 14/15 (E4M6V4) on day seven of admission, although he remained disoriented. Anterograde amnesia and difficulty in looking upwards were discovered. The left oculomotor palsy had resolved partially. By eleventh day he became oriented with improvement in his memory, but disturbance of vertical gaze was persistent. He was discharged and is being followed-up on outpatient basis.
Discussion
The thalami contain strategic nuclei and integrate several important cortical functions. The posterior communicating artery contributes to thalamic blood supply in 60% of humans. This is accomplished by a well characterised artery, the polar artery. Percheron described possible variations involving the paramedian thalamic-mesencephalic arterial supply [2]. Our patient demonstrated infarcts in bilateral paramedian thalamus as well as parts of mesencephalon consistent with occlusion of one of the less common variants, a common trunk arising from a P1 segment (ie, the artery of Percheron). The obstruction was likely a consequence of cardiac embolism occurring as a result of atrial fibrillation.
Occlusion of the artery of Percheron results in bilateral medial thalamic and rostral midbrain infarctions with a relative symmetrical distribution [4]. Infarcts in this region may result in complex clinical syndromes, with patients manifesting varying symptoms and signs ranging from motor deficits to behavioral and sensory alterations. The four main symptoms found in literature are vertical gaze palsy (65%), memory impairment (58%), confusion (53%), and coma (42%) [5]. Our patient presented with all these typical features of this stroke syndrome over his course of illness. The changes in mental status may be due to involvement of reticular activating system and the interruption of connections between the thalamus and parts of the prefrontal cortex involved in behavioral control. Vertical gaze palsy is due to disruption of the cortical input that traverses the thalamus to reach the rostral interstitial medial longitudinal fasciculus. The presence of left oculomotor palsy in our patient is due the simultaneous involvement of the mesencephalic periaqueductal gray matter at the level of superior colliculus which is the location of the third cranial nerve nuclei. Early diagnosis is best made by a diffusion-weighted imaging (DWI) sequence using MRI.
Similar cases of bilateral paramedian thalamic infarction with clinical and MR findings suggestive of artery of Percheron occlusion have been reported [6,7]. Cassourret et al reported a case of occlusion of the artery of Percheron, comatose at presentation, with normal early imaging by head computed tomography (CT) and MRI [8]. A new head CT two days later revealed a bilateral paramedian thalamic infarct at the origin of the initial symptoms. Matheus and Castillo reported 3 cases with typical symmetric thalamic and mesencephalic lesions on MR imaging with distribution conforming to the occlusion of the artery of Percheron [9]. Successful artery of Percheron in situ thrombolysis using tissue plasminogen activator in an angiographically diagnosed patient has been reported [10].
In the case reported here, conventional MR imaging and the diffusion-weighted imaging confirmed the presence of infarction in bilateral thalamic and left anteromedial midbrain region typically seen in occlusion of the artery of Percheron [11]. These infarcts should be recognized as due to occlusion of a possible single rare artery that is a normal anatomic variant showing its peculiar supply and not be blamed on occlusion of multiple vascular territories or other pathologic conditions such vasculitis or infectious disease. When bilateral paramedian thalamic infarcts with or without associated mesencephalic involvement are found, occlusion of the artery of Percheron should be considered as the foremost differential diagnosis. Performing conventional angiography is usually not indicated in such cases. Because of the small size of the artery and its highly variable origin and course, lack of visualization of the artery does not exclude its presence, however interventional explorations focused on potential treatment of occlusion of the artery of Percheron may be encouraged.
Conclusion
• In patients presenting with bilateral paramedian thalamic infarction the possibility of artery of Percheron of infarction should be considered.
• In artery of Percheron of infarction, there can be additional involvement of periaqueductal grey matter of the midbrain.
• Clinical features may vary but loss of consciousness, memory impairment, vertical gaze palsy and behavioural disturbances are most common.
• Possibility of cardioembolism should always be kept in the etiological differentials of stroke.
References
- 1. Bogousslavsky J, Melle GV, Regli F. The Lausanne Stroke Registry: analysis of 1,000 consecutive patients with first stroke. Stroke. 1988;19:1083–1092.
- Percheron G. Arteries of the human thalamus. II. Arteries and paramedian thalamic territory of the communicating basilar artery. Rev. Neurol. (Paris). 1976;132:309–324.
- Lazzaro NA, Wright B, Castillo M, Fischbein NJ, Glastonbury CM, Hildenbrand PG, et al. Artery of Percheron Infarction: Imaging Patterns and Clinical Spectrum. Am J Neuroradiol. 2010;31:1283–1289.
- Castaigne P, Lhermitte F, Buge A, Escourolle R, Hauw JJ, Lyon-Caen O. Paramedian thalamic and midbrain infarct: clinical and neuropathological study. Ann. Neurol. 1981;10:127–148.
- Monet P, Garcia P-Y, Saliou G, Spagnolo S, Desblache J, Franc J, et al. Bithalamic infarct: is there an evocative aspect? Radioclinical study. Rev. Neurol. (Paris). 2009 ;165:178–184.
- López-Serna R, González-Carmona P, López-Martínez M. Bilateral thalamic stroke due to occlusion of the artery of Percheron in a patient with patent foramen ovale: a case report. J Med Case Rep. 2009;3:7392.
- Raphaeli G, Liberman A, Gomori JM, Steiner I. Acute bilateral paramedian thalamic infarcts after occlusion of the artery of Percheron. Neurology. 2006;66:E7.
- Cassourret G, Prunet B, Sbardella F, Bordes J, Maurin O, Boret H. Ischemic Stroke of the Artery of Percheron with Normal Initial MRI: A Case Report. Case Report Med. 2010;2010:425734. doi:10.1155/2010/425734
- Matheus MG, Castillo M. Imaging of Acute Bilateral Paramedian Thalamic and Mesencephalic Infarcts. Am J Neuroradiol. 2003;24:2005–2008.
- Kostanian V, Cramer SC. Artery of Percheron Thrombolysis. Am J Neuroradiol. 2007;28:870–871.
- Küker W, Weise J, Krapf H, Schmidt F, Friese S, Bähr M. MRI characteristics of acute and subacute brainstem and thalamic infarctions: value of T2- and diffusion-weighted sequences. J. Neurol. 2002;249:33–42.
|