6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffd4c3020000001601000001001400
6go6ckt5b5idvals|190
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Sebaceous carcinoma of eyelid is a rare, lethal neoplasm of ocular adnexa. It commonly originates in the tarsal Meibomian glands and rarely from glands of Zeis of cilia, sebaceous glands of eyebrow and glands of caruncle [1]. It frequently masquerades as a benign condition like chalazion, chronic blephero-conjunctivitis and kerato-conjunctivitis [2]. Early diagnosis is of extreme importance to avoid high morbidity and mortality. Fine needle aspiration cytology (FNAC) is a rapid, easy and inexpensive tool which can be valuable in early diagnosis of surface ocular lesion [2,3]. We present a case of eyelid sebaceous carcinoma diagnosed on cytology.
Case Report
A 45 year female presented with a diffuse swelling of right eye with sloughing of overlying skin since one year. To begin, it was a small-ulcerated lesion measuring 1x1 cm over the upper eyelid, which later on progressed to involve the lower eyelid resulting in obliteration of the palpebral fissure and loss of vision. Computerized Tomography showed a heterogeneous, enhancing, expansile, soft tissue mass in the right eye causing destruction of the floor and medial wall of the orbit displacing the globe laterally & extending into the right nasal cavity.
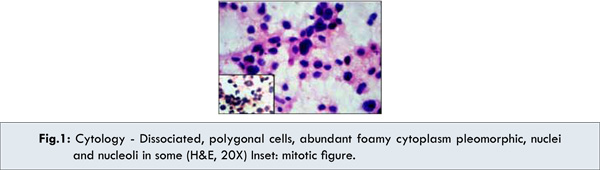
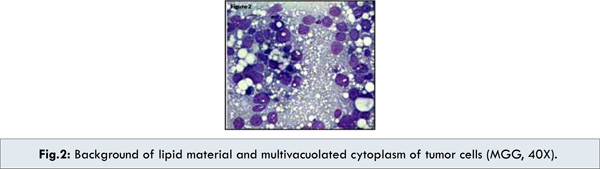
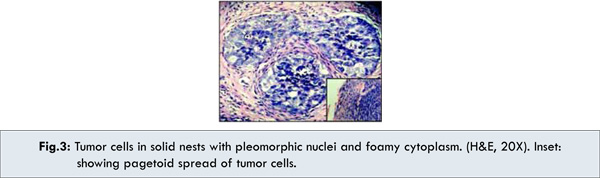
FNA was done from indurated area over lower eyelid. Some smears were fixed in 95% ethanol & others were air-dried. Wet fixed smears were stained with Papanicoloue stain and H&E stain, while air dried smears were stained with May Grunwald Giemsa stain (MGG). The smears were richly cellular, with cells in loose clusters, groups & singly scattered [Fig.1]. The individual cells were large, polygonal with abundant, foamy, cytoplasm and central, large, pleomorphic nucleus with coarse chromatic and prominent nucleoli. Multinucleated tumor giant cells & mitotic figures were evident [Fig.1,inset]. The multivacuolated cytoplasm and lipid rich background were better seen in MGG stain [Fig. 2]. The cytological diagnosis of sebaceous carcinoma of the eyelid was offered. Subsequent, biopsy from the lesion showed ulcerated epidermis with extensive inflammation. The underlying tissue revealed tumor comprising of lobules and nests of large polygonal cells with abundant foamy, lipid rich cytoplasm having hyperchromatic and pleomorphic nucleus [Fig. 3] with mitotic figures and pagetoid involvement of overly epidermis [Fig. 3, inset].
Discussion
Ocular surface lesions are easily accessible to the application of cytology. If the lesion is nodular FNA can be done, or if ulcerated, scrape smears can be taken [2]. Historically sebaceous carcinoma of eyelid is known for masquerading to more common benign conditions, often resulting in a long delay before the correct diagnosis is being made [2,4]. Delay is diagnosis can increase the chance of local recurrences & metastasis. Clinically, it may be mistaken for lesions like chalazion, chronic blepharo-conjunctivitis, kerato-conjunctivitis, basal cell carcinomas and squamous cell carcinoma. Early diagnosis is thus of extreme importance to avoid high morbidity and mortality.
The incidence of sebaceous carcinoma in western literature is reported to be less than 1% off all eyelid tumors and accounts for 1-5% of all malignant eyelid tumors [3]. Recent studies from India and China have shown that sebaceous carcinoma accounts for 33-60% of malignant eyelid tumors. It thus seems that the incidence of sebaceous carcinoma has a geographical variation and is more common in Asian population [3]. Presence of cytoplasmic vacuolation in smears is a helpful clue for diagnosing sebaceous carcinoma [4]. Another important feature is tendency for pagetoid spread within the conjunctival epithelium or the overlying skin. If the sebaceous carcinoma is unknown then the pagetoid spread can easily be mistaken for in situ squamous cell carcinomas of conjunctiva unless cytopathologist detects the vacuolated tumor cells. The differentials, which need to be excluded, were basal cell carcinoma, squamous cell carcinoma and pilomatricoma. Smear from basal cell carcinomas are parvi- cellular comprising of more tightly packed cohesive clusters of small monomorphic basaloid cells with hyper chromatic nuclei, high nucleo-cytoplasmic ratio and a narrow rim of cytoplasm. The cells show peripheral palisading. They rarely metastasize and have a predilection for lower eyelid [4-6]. In contrast to this sebaceous carcinoma reveal richly cellular smears comprising of loose clusters and dissociate cells against lipid rich background, which is highlighted in MGG stain. The cells were large with abundant, multivacoulated foamy cytoplasm [7]. Squamous cell carcinoma show polygonal, tadpole to fiber cells with central, dark, hyperchromatic, pleomorphic nucleus and abundant dense eosionophilic cytoplasm, which may show keratinization [2]. In a few cases of sebaceous carcinoma, the fatty content liberated from sebaceous glands due to ductal obstruction might evoke a granulomatous response accompanied by neutrophils creating confusion with blepharitis and chalazion. Smears from chalazion displayed features of inflammatory granuloma comprising of lymphocytes, plasma cells, multinucleated giant cells and extracellular fat and absence of atypical cells [2,4]. Rarely pilomatricoma may come in the differential diagnosis, which typically shows bland sheets of basaloid cells, ghost cells and calcification [4,5,7].
The poor prognostic factors are duration more than six months, infiltrative and pagetoid spread, orbital and lymphatic invasion. Mortality is about 23%, spread by direct extension is usual but metastasis to lymph node, lung, liver, brain, and skull is possible [8]. The prognosis in our patient was poor due to infiltrative and pagetoid spread along with orbital involvement. The treatment of sebaceous carcinoma without orbital involvement is wide local excision with clear margins. In cases of orbital involvement, excenteration is required. Radiation is useful when surgery cannot be tolerated [9]. In our patient, because of widespread involvement, she was given radiotherapy.
FNA being an OPD procedure needs less preparation and is less painful in comparison to biopsy. Sebaceous carcinoma was diagnosed on cytology and later confirmed on histopathology.
Conclusion
Fine needle aspiration cytology holds an important role and can be a safe and effective tool in early diagnosis of surface ocular neoplasm like sebaceous carcinoma.
References
- Gardetto A, Rainer C, Ensinger C, Baldisserra I, Piza-Katzer H. Sebaceous carcinoma of eyelid : a rarely worth considering. Br. J. Ophthal. 2002;86:243-244.
- Vemuganti GK, Rai NN. Symposiun on ophthalmic cytology: Neoplastic lesions of eyelid, eyeball and orbit. Journal Cytol. 2007;24:30-36.
- Maheshwari M, Mahashwari S, Shedke S. Role of FNAC in diagnosis of eyelid sebaceous carcinoma. Indian Journal Ophthalm. 2007; 55:217-219.
- Aarthi CA, Vijaya C. Scrape cytology on early diagnosis of sebaceous carcinoma. Journal Cytol. 2010; 27:140-142.
- Gao L. Lin W H, Gong ZJ, Liu YM, Zhu MH. Fine needle aspiration cytology of eyelids sebaceous carcinoma and its differential diagnosis. Zhonghua Bing Li Xuv Za Zhi. 2004;33:36-39.
- Sadeghi S, Pitman B, Weir MM. Cytological features of metastatic sebaceous carcinoma: two cases comparison to three cases of basal cell carcinoma. Diagnostic Cytopath. 1990;21:340-345.
- Gill M, Garg S, Kalra R, Sen R. Sebaceous carcinoma of eyelid diagnosed on fine needle aspiration Cytology J Cytol. 2012;29:75-76.
- Rao NA, Hidayat AA, McLean, Zimmerman LE. Sebaceous carcinoma of ocular adnexa. A clinicopathologic study of 104 cases with five-year follow up data. Hum Pathol. 1982;13:113-122.
- Zürcher M, Christoph R, Hintschich, Garner A, Bunce C, J Richard O Collin. Sebaceous carcinoma of the eyelid: a clinicopathological study. Br J Ophthalmol. 1998; 82:1049-1055.