6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff6892300000007207000001000a00
6go6ckt5b5idvals|2032
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Left main coronary artery (LMCA) either primary or secondary is harbinger to catastrophic vessel closure. It can be precipitated by manipulation of hardwares in LM ostium or during intervention of the ostial lesion of the left anterior descending artery (LAD). The incidence of dissection occurring during catheter-based procedures is around 0.1% [
1,
2]. Secondary coronary artery dissections may be due to an anterograde extension of an aortic dissection or iatrogenic during manipulation during routine catheterization or intervention. It can complicate into embolization, ischaemia, perforation, and terminally into ventricular fibrillation [
3].
Case Report
A 68-year-old diabetic and smoker male presented with exertional angina-Canadian Cardiovascular Society (CCS) - class II for past 4 years. His hemogram and routine biochemistry were normal. An electrocardiogram showed mild ST depression in V1-4 with preserved R wave. Cardiac markers for necrosis were negative. Echocardiography revealed mild concentric left ventricular hypertrophy, grade-II diastolic dysfunction, and normal systolic function with an ejection fraction of 60%.
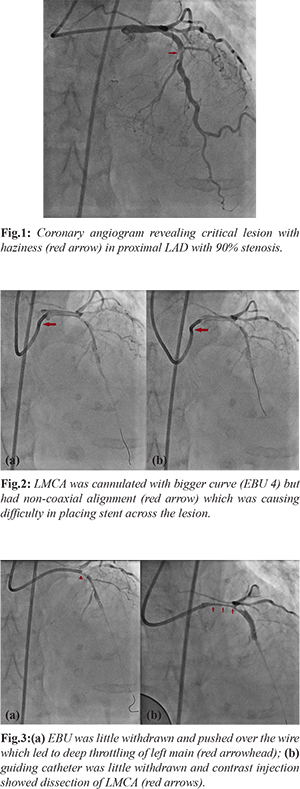
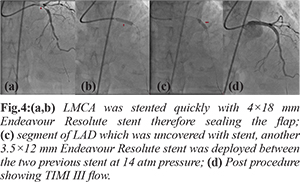
Coronary angiogram was performed after proper consent through transfemoral route which revealed critical lesion in proximal LAD with 90% stenosis [Fig.1]. Ascending aorta was dilated as LMCA could not be cannulated with Judkins left (JL) 3.5 diagnostic catheter. It was cannulated with JL 4 catheter with difficulty. LMCA could not be hooked with 6F extra backup guide catheter 3.5 (EBU- Medtronic, USA). Somehow it was cannulated with bigger curve (EBU 4). Lesion was crossed with 0.014" run through wire (Terumo, Japan) and was gradually predilated using 2×10, and 2.5×10 mm sapphire semicompliant balloons (Orbus Neisch, Netherland). 3×18 mm Endeavour Resolute Zotarolimus eluting stent (Medtronic, USA) was tracked across the lesion but could not be properly placed as guiding was not properly cannulating the ostium of left main artery [Fig.2a,b]. EBU was little withdrawn and pushed over the wire which led to deep throttling of left main artery [Fig.3a]. Stent was deployed at 12 atm pressure where the monitor showed ventricularization of pressure trace. Guiding catheter was little withdrawn and contrast injection showed dissection of LMCA as patient had severe chest pain, profound hypotension as blood pressure fell down to 60/40 mmHg and ST elevation in V1-6 [Fig.3b,4a]. Intravenous infusion of normal saline was started. In order to salvage the patient, LMCA was stented quickly with 4×18 mm Endeavour Resolute stent at 14 atm pressure which stabilized the blood pressure and ST changes [Fig.4b]. As there was another segment of LAD which was uncovered with stent, another 3.5×12 mm Endeavour Resolute stent was deployed between the two previous stent at 14 atm pressure [Fig.4c]. All the deployed stents were post-dilated using 4×10 mm and 3.5×10 mm non-compliant balloon at high pressure. Post-procedure, blood pressure rose to 112/48 mmHg with TIMI III flow and normalization of ST changes [Fig.4d]. He was discharged in stable condition with ticagrelor 180 mg, aspirin 75 mg, rosuvastatin 40 mg, metoprolol 100 mg, ramipril 10 mg, and gilbenclaimide 2 mg once daily. He is in regular follow up since then.
Discussion
Catheter-induced left main coronary artery dissection is a rare but well-recognized life-threatening complication of coronary intervention. Emergent coronary artery bypass surgery (CABS) is indicated and has been associated with good clinical outcomes. In our case, it was either distal dissection of left main or proximal dissection of ostium of LAD which progressed retrograde involving the whole of left main artery. Although the exact mechanism of iatrogenic left main dissection with retrograde progression is not exactly known, mechanism is progressive retrograde dispersion of the sub-intimal space created by entry point which originates within the dissection plane as a result of trauma induced by guide catheter. These can be result of vigorous hand injection of contrast medium, sub-intimal passage of the guidewire, and/or inadvertent handling of the guiding catheter. Predisposing factors are cystic medial necrosis, hypertension, Marfan syndrome, and atherosclerosis. Plaque disruption may serve as an entry point for the pulsatile flow of blood as atherosclerosis also weakens the media.
Iatrogenic LMCA dissection results from excessive manipulation of the catheter; changing catheters to others with greater curvature or of different forms (Amplatz), to overcome difficulties found in LMCA catheterization due to its unusual location at the aortic root; vigorous contrast medium injection with the catheter in a no coaxial alignment; use of hard-tip catheters; and deep intubation of the catheter [
1,
2]. In our case, vigorous manipulation as well as deep engagement, both were responsible. EBU guide (Medtronic; USA) are relatively stiffer compared to XBU (Cordis Corp; USA) or Mac 1(Boston Scientific; USA). Management of iatrogenic left main dissection stent implantation is an appropriate alternative to coronary artery bypass graft surgery, because it is a rapid and effective treatment [
2]. Conservative treatment is applicable for hemodynamically stable patient with a low-grade dissection [
2]. Intervention is indicated for hemodynamic instability. Catheter based intervention, in the form of stenting (covered stent, bare metal stent, drug eluting stent) of the coronary dissection entry point, is reserved for patients with “limited” aortic involvement (within 40 mm from the coronary ostium) [
2]. IABP and temporary pacing may be needed in some cases but sudden and rapid downhill hardly gives any time, and therefore timely recognition of the isolated left main dissection is of paramount importance as early and prompt stenting of the entry point in the coronary tree may prevent retrograde aortic extension. Survival rates of approximately 90% and restenosis rates at six months ranging from 0-30% have been demonstrated in small series of patients with iatrogenic LMCA dissection over 12-30 months period. One should remain vigilant and perform angiography to rule out LMCA restenosis as they may manifest as sudden death [
5,
6].
Conclusion
Catheter-induced left main coronary artery dissection can be precipitated by vigorous manipulation. Early recognition of the isolated left main dissection and prompt stenting of the entry point in the coronary tree may prevent further complication.
Contributors: SKS: Drafting the work and patient management; VK: substantial contributions to the conception and critical review of the work. SKS will act as a study guarantor. Both authors approved the final version of the manuscript and are responsible for all aspects of the study.
Funding: None; Competing interests: None stated.
References
- Ertas G, Ural E, Van Der Giessen WJ. Successful stenting of catheter-induced unprotected left main coronary artery dissection. Cardiovasc J Afr. 2012;23:e6-e7.
- Awadalla H, Sabet S, Sebale A, Rosales O, Smalling R. Catheter-induced left main dissection incidence, predisposition and therapeutic strategies experience from two sides of the hemisphere. J Invasive Cardiol. 2005;17:233-236.
- Boyle AJ, Chan M, Dib J, Resar J. Catheter-induced coronary artery dissection: Risk factors, prevention and management. J Invasive Cardiol. 2006;18:500-503.
- Awadalla H, Salloum JG, Smalling RW, Sdringola S. Catheter-induced dissection of the left main coronary artery with and without extension to the aortic root: A report of two cases and a review of the literature. J Interven Cardiol. 2004;17:253-257.
- Onsea K, Kayaert P, Desmet W, Dubois CL. Iatrogenic left main coronary artery dissection. Neth Heart J. 2011;19:192-195.
- Lee SW, Hong MK, Kim YH, Park JH, Rhee K, Lee CW, et al. Bail-out stenting for left main coronary artery dissection during catheter-based procedure: acute and long-term results. Clin Cardiol. 2004;27:393-395.